“MDR-Pseudomonas: Another Horse of the Apocalypse”
advertisement
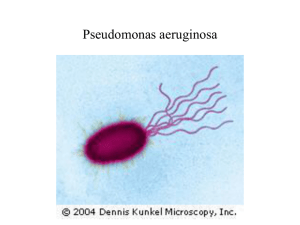
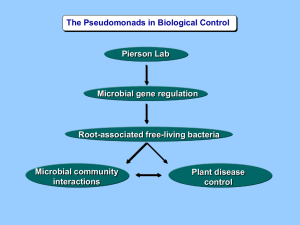
“MDR-Pseudomonas: Another Horse of the Apocalypse” Jeanette Harris MS, MSM, MT(ASCP), CIC MultiCare Health System Tacoma, WA MultiCare Infection Prevention team Jeanette with Marcia, Steve, Sue, Stacia and Roxy Pseudomonas sp. • ''Pseudomonad'' = 'false unit' – Greek pseudo (ψευδο 'false') and monas (μονάς / μονάδα 'a single unit') – "monad" was used in the early history of microbiology = single-celled organisms – First described 1894 – Gram-negative, rod-shaped and polar-flagella bacteria. – Pseudomonas aeruginosa is the type species of its group contains 12 other members Pseudomonas aeruginosa • Free-living bacterium, found in soil and water • Occurs regularly on the surfaces of plants and animals • Genus is well known to plant microbiologists groups of bacteria that are plant pathogens • Emerging opportunistic pathogen of clinical relevance • Epidemiological nosocomial transmission • Antibiotic resistance is increasing in clinical isolates. Pseudomonas aeruginosa • Epitome of an opportunistic pathogen of humans • Never infects uncompromised tissue – there is hardly any tissue that it cannot infect if the tissue defenses are compromised in some manner • Causes urinary tract infections, respiratory system infections, dermatitis, soft tissue infections, bacteremia, bone and joint infections, gastrointestinal infections and a variety of systemic infections, particularly in patients with severe burns and in cancer and AIDS patients who are immunosuppressed. • Serious problem in patients hospitalized with cancer, cystic fibrosis, and burns • The case fatality near 50 percent Pseudomonas aeruginosa • Primarily a nosocomial pathogen • Overall incidence of P. aeruginosa infections in U.S. hospitals averages about 0.4 percent (4 per 1000 discharges) • Fourth most commonly-isolated nosocomial pathogen accounting for 10.1 percent of all hospital-acquired infections* *CDC Pseudomonas aeruginosa • Ubiquitous in soil and water • On surfaces in contact with soil or water • Metabolism is respiratory and never fermentative • But it will grow in the absence of O2 if NO3 is available as a respiratory electron acceptor. Pseudomonas aeruginosa • In nature might be found in a biofilm, attached to some surface or substrate, or in a planktonic form, as a unicellular organism, actively swimming by means of its flagellum • The most vigorous, fast-swimming bacteria seen in hay infusions and pond water samples • Do you have a hot tub? Swimming pool? Pseudomonas aeruginosa • Very simple nutritional requirements • Observed "growing in distilled water", which is evidence of its minimal nutritional needs • In the laboratory, the simplest medium for growth of Pseudomonas aeruginosa consists of acetate as a source of carbon and ammonium sulfate as a source of nitrogen Pseudomonas aeruginosa • Organic growth factors are not required, can use more than seventy-five organic compounds for growth • Optimum temperature for growth is 37 degrees, able to grow at temperatures as high as 42 degrees • Resistant to high concentrations of salts and dyes, weak antiseptics, and many commonly used antibiotics • Predilection for growth in moist environments, reflection of its natural existence in soil and water • Contribute to success as an opportunistic pathogen • May produce three colony type – Natural isolates from soil or water - small, rough colony – Clinical samples • Tissue - smooth colony type • Respiratory and urinary tract secretions - mucoid attributed to the production of alginate slime • smooth and mucoid colonies are presumed to play a role in colonization and virulence. Capable of growing in diesel and jet fuel---WILL be a part of the oil spill P. aeruginosa • Two types of soluble pigments – Pyoverdin = Fluorescent pigment – Pyocyanin = blue pigment • produced abundantly in media of low-iron content and functions in iron metabolism • (from "pyocyaneus") refers to "blue pus", which is a characteristic of suppurative infections Pyocyanin = Blue Pigment • Impairs the normal function of human nasal cilia, disrupts the respiratory epithelium, and exerts a proinflammatory effect on phagocytes • plays a role in invasion if it extracts iron from the host for bacterial growth in a relatively iron-limited environment Resistance to Antibiotics • Notorious for resistance to antibiotics • Naturally resistant to many antibiotics due to permabiliity barrier Gram-negative outer membrane • Biofilm form makes the cells impervious to therapeutic concentrations antibiotics • Lives with actinomycetes and molds – acquired resistance to naturally occurring antibiotics • Maintains antibiotic resistance plasmids, both R-factors and RTFs, and it is able to transfer these genes by means of the bacterial mechanisms of horizontal gene transfer (HGT), mainly transduction and conjugation • Few antibiotics are effective – Fluoroquinolones, gentamicin and imipenem – Cystic fibrosis - so resistant that it cannot be treated Pathogenesis • Opportunistic pathogen – disease process begins with some alteration or circumvention of normal host defenses – Multifactorial - wide array of virulence determinants possessed by the bacterium – Include septicemia, urinary tract infections, pneumonia, chronic lung infections, endocarditis, dermatitis, and osteochondritis • Invasive and toxinogenic – Three distinct stages • bacterial attachment and colonization • local invasion • disseminated systemic disease Colonization • Part of the normal flora of humans – healthy individuals outside the hospital is relatively low (024%) • Pili adhere to epithelial cells of upper respiratory tract • Adhesins bind to specific galactose or mannose or sialic acid receptors on epithelial cells • Respiratory tract requires pili adherence and production of a protease enzyme that degrades fibronectin in order to expose the underlying pilus receptors on the epithelial cell surface • Tissue injury plays a role in colonization of the respiratory tract – +Adhere to tracheal epithelial cells infected with influenza virus Invasion • Production of extracellular enzyme toxins break down barriers and damage host cells, as well as resistance to phagocytosis and the host immune defenses • Bacterial capsule or slime layer protects bacteria from opsonization by antibodies, complement deposition, and phagocyte engulfment • Extracellular proteases provide virulence at the invasive stage – elastase and alkaline protease – a cytotoxin (mw 25 kDa) and two hemolysins Toxinogenesis-2 • Exoenzyme S – produced by bacteria growing in burned tissue and may be detected in the blood before the bacteria are – may act to impair the function of phagocytic cells in the bloodstream and internal organs as a preparation for invasion by P. aeruginosa. • Exotoxin A (Similar to diphtheria toxin) – enters cells in the same manner and has the exact enzymatic mechanism – local and systemic disease processes – necrotizing activity at the site of bacterial colonization – toxinogenic strains cause a more virulent form of pneumonia than nontoxinogenic strains – purified Exotoxin A is highly lethal for animals including primates Cell-to-Cell Signaling • They TALK to each other! • Sense their own cell density • Behave as a population instead of individual cells • Express specific genes as a population instead of individual cells • Think of the Borg from Star Trek Diseases • • • • • • • • • • Endocarditis Respiratory infections Bacteremia and septicemia Central nervous system infections Ear infections including external otitis Eye infections Bone and joint infections Urinary tract infections Gastrointestinal infections Skin and soft tissue infections, including wound infections, pyoderma and dermatitis Host Defenses • Killing is most efficient in the presence of type-specific opsonizing antibodies • Phagocytosis plus opsonizing antibody is principal functional • Once infection is established, other antibodies, such as antitoxin is important • Cystic fibrosis is the exception Epidemiology and Control • Found EVERYWHERE • Hospital: – disinfectants, respiratory equipment, food, sinks, taps, toilets, showers and mops – fruits, plants, vegetables, visitors, patients transferred from other facilities – patient to patient on the hands of hospital personnel, by direct patient contact with contaminated reservoirs, and by the ingestion of contaminated foods and water Control • Isolation procedures, aseptic technique, and careful cleaning and monitoring of respirators, catheters, and other instruments • Topical therapy of burn wounds with antibacterial agents such as silver sulfadiazine, coupled with surgical debridement Patterns Event: 11.8 times higher incidence of Hospital Pseudomonas aeruginosa Respiratory Isolates from ICU. Active period (3 months) compared to base line period (9 months) *^&%$#@$%^((((*%###%!!!!!! What we did 1. 2. 3. 4. Switch to sterile water for feeding tubes BLEACH for cleaning Staff Education Check for sources of moisture contamination 5. Inspection of unit - guess what we found 6. “What’s different?” 7. Should we just nuke the rooms? How it worked Not ZERO….but MUCH better What’s next? Pseudomonas bioremediation was used was the Exxon Valdez Oil Spill …..remember, Pseudomonas eats EVERYTHING! Crude Oil = Carbon + Hydrogen • Pseudomonas can use over 100 different molecules as carbon sources, including proteins, fats, carbohydrates, and hydrocarbons • Found in carbon dioxide and organic compounds. Hydrogen •Together with oxygen, essential to all aspects of cell Clean-up crews use the Pseudomonas putida bacteria to decontaminate soil polluted by oil spills. So….Maybe there’s some good news after all