Exercise and Sport for Amputees
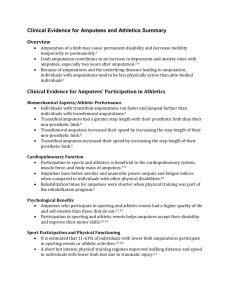
advertisement
Exercise and sport for amputees Erin Kennedy Physiotherapist, Westmead Hospital 2014 What does the research tell us about amputees and physical activity? • The amputee population is largely elderly with low levels of fitness or activity (Davies and Datta, 2003). • Those with limb absence could and should engage in physical activity to improve their health and social inclusion (Webster et al 2001). • Common for amputees in a rehabilitation program to achieve a level of physical functioning which may not challenge them to move beyond the basic goal of walking (Deans et al, 2008). A recent review of 12 articles in Prosthetics and Orthotics International asked the following questions: • Are people with amputations participating in physical activity? • Are these people participating at the same level as before their amputation? • What are their motivations and barriers to participation? » Deans et al (2012) And found…. • People with amputation are generally inactive. – 68% of amputee population V 40% general population • There is a decrease in the level or leisure activity following lower limb amputation. • However, satisfaction with changed physical status remains high. • Likelihood of participating in physical activity exercise and sport increased if they participated prior to amputation. • If they do return to physical activity they opt for less strenuous activities where a prosthesis is not required or not functionally dependent on a prosthesis to participate » Deans et al (2012) Motivations for physical activity include: • • • • • • Health benefits Social interaction Stress relief Increasing self esteem Improving body image Mastery theory – Mastery of prosthesis • increased self efficacy • increased prosthetic use • Increased physical activity » Deans et al (2012) Barriers for physical activity include: • • • • • • • • • Physical limitation Lack of confidence / embarrassment Body image attitude Services Climate/physical environment Income Stump pain Prosthesis » Deans et al 2012 So…. • How can we encourage our patients to engage in regular physical activity? – Setting goals – Education • • • • • Health benefits Recommended daily activity Appropriate forms of exercise Looking after skin/stump Address misconceptions – Providing a positive environment And… • Which patient should be challenged beyond walking? – Those who were previously physically active and are medically well – Age range ?? – Level and number of amputations?? – K 3-4 • Community ambulation, able to vary cadence and perform activities beyond basic locomotion – Amp pro score • > 37 – 6mwt • > 250m Gailey et al (2002) How do we enable them to realise their potential? • First rehab them to walk well!!! – Flexibility, strength, balance, specific gait exercises…. • Gait asymmetries due to tightness, weakness, impaired balance (Kapp, 2004) – – – – – – – – • altered base of support decrease weight-bearing and stance time on prosthetic limb increase stance time on the intact lower limb increase double support time asymmetrical step length with a shorter faster stride on the intact limb longer stride on the prosthetic limb lateral trunk bending toward the prosthetic side reduced walking velocity. These gait asymmetries will cause limitations in the amputees ability to perform high-level mobility activities. Flexibility • General stretches – – – – – – Hip flexors Glutes Hamstrings Quads Adductors Lower back – Calf Strength • To successfully walk and take part in sports or physical activity the amputee needs to be strong! • Muscles critical to amputee mobility – – – – Hip extensors Hip extensor and abductor muscle power have been found to predict mobility. (Raya et al 2010, Powers et al, 1996). Hip abductors Knee extensors Remaining plantar flexors • Healthy amputees can increase residual limb hip and knee strength with training (Nolan, 2009). • Can assess/measure/strengthen LL power functionally (Raya et al, 2010). – STS, SIT, ↑↓Stairs can be used as measures of lower limb power, balance, coordination, speed, and gait symmetry to determine their impact on high-level mobility performance of lower limb amputees??? Glute training exercises • • • • • • • • Hip ext in prone (neutral and 30 abd) Hip abd in SL with circles TB in standing Stair drills Bridging +/- gym ball Single leg bridge foam roller Plank with hip ext Crab walks +/- theraband Quads training exercises • • • • • Step ups/downs Squats, +/- resistance Bulgarian squats lunges Stair drills – 2 at a time, sideways, grapevine • Controlled SIT Hamstring training exercises • • • • • Bridging Single leg bridging Gym ball hamstring curls Hamstring curls in 4pt kneeling Hamstring pulses in prone Core/abdo training exercises • TrA – – – – Supine crook lying establish core control Bridging Bird dog/superman Standing with UL or LL TB • Abdo crunches/obliques • Abdo roll with gym ball • plank Balance • Lower limb amputees typically present with impaired balance due to motor and/or sensory deficits. • For lower limb amputees, hip strategies need to be trained to work differently and more efficiently in order to compensate for the missing ankle strategy. Buckley et al (2002) Balance • weight shift – Straddle stance – Step stance • • • • • • • Side stepping braiding Step taps Throwing and catching ball Bouncing ball Kicking and trapping ball Wobble board Walking drills • • • • • • • Walking F/B/S Walking along line braiding High knees Monster steps Ski walking Walking with resistance ** concentrate on foot placement ** ** don’t forget arm swing ** Endurance • Running and Sports participation is hard work so need to work on endurance. – – – – – Walking Swimming Cycling Rowing machine Arm cycle When to teach the amputee to run • • • • • Walking well unaided Amp pro >37 6mwt > 250m?? Good socket fit Motivated - The Comprehensive High-level Activity Mobility Predictor (CHAMP) • CHAMP is a measure of agility typically used to test highlevel performers who tend to max-out their ratings on other performance-based measures. • This measure includes activities that are designed to test motion in all three planes, like turning, cutting, side-toside movement, and backward running. • It consists of four tasks and can be administered in 15-20 minutes. – – – – SLS Edgren side step test T-test Illinois agility test CHAMP • Found to be – – – – – Safe Reliable Valid Clinically friendly responsive performance based outcome measure of highlevel mobility • Has the potential to direct rehabilitation goals and treatment, determine when to return to high level activity and aid in discharge planning. Amputee Running Technique • Prosthetic trust – reaching out with the prosthetic limb and knowing it will be there – Get used to the impact of landing on prosthetic side • Training exercises – Repeated single hops on prosthetic side (TTA only) – Side skip » http://www.oandp.com/articles/2003-12_05.asp Amputee Running Technique • Backward thrust – Forceful hip extension on heel strike to propel body over prosthesis – Accelerates body forwards – Increases speed • Training exercise – Push down and pull back with limb at same time inside the socket – Standing with hip flexed 90. Therapist provides few seconds of medium resistance to extension then lets go and amputee drives heel to floor, pushing into back wall of socket. – Use glutes and hamstring muscle groups » http://www.oandp.com/articles/2003-12_05.asp Amputee Running Technique • Sound limb stride – Novice athletes will have a shorter stride. • Training exercise – extend hip by pulling down and back into socket – Leap from prosthesis onto sound side – Focus on long stride with sound limb » http://www.oandp.com/articles/2003-12_05.asp Amputee Running Technique • Stride symmetry – Strive for equal stride length and frequency • Training exercise – Choose a comfortable jogging pace that produces equal stride length for both limbs – Concentrate on maintaining stability over prosthetic limb – Relax and jog a little » http://www.oandp.com/articles/2003-12_05.asp Amputee Running Technique • Arm swing – Novice runners keep arms close to their bodies – Encourages stride length and timing • Training exercise – Focus on arm swing and trunk rotation • Shoulders relaxed • Elbows flexed 90 • Hands… – Should rise to shoulder level when driving forwards – Should point just behind hip when driving backwards » http://www.oandp.com/articles/2003-12_05.asp Considerations!! Socket design • Well fitting prosthesis – Comfort • Shape, interface material, alignment, adapt to forces imposed at the stump socket interface – ROM • Adequate hip/knee ROM – Stability – Adaptability to volume changes • Constant challenge for endurance athletes – Gailey and Harsh (2009) Foot selection for running • Considerations – Residual limb length • Clearance 17-25cm – Distance • Sprint: carbon fibre ‘J shaped’ foot • Endurance: carbon fibre ‘C shaped’ foot • Multisport carbon fibre foot with heel – Athletes preference – Athletes skill • Novice V’s professional • Gailey and Harsh (2009) Knee selection running • Use of a prosthetic knee permits a more traditional style of running with knee flexion and extension. • Endurance knees • Mauch (single axis, hydraulic) • Ossur total knee 2100 (polycentric hydraulic) • Ossur 3R55 (poycentric, hydraulic swing) • Gailey and Harsh (2009) Equipment • Small towel – Perspiration constant problem • Moist wipes – Cleaning socket, liners, suspension sleeves immediately after training/sport • Skin dressings – If abrasions or blister occur • Extra stump socks – Limb volume may change with muscular contractions, altered diet, weight loss due to training. • Elastic sleeve or auxillary suspension • Gailey and Harsh (2009) references • • • • • • • • • • • • • Deans S, Burns D, McGarry A, Murray K and Mutrie N (2012) Motivations and barriers to prosthesis users participation in physical activity, exercise and sport: a review of the literature. Prosthetics and Orthotics international 36(3) 269-269. Czerniecki J, Gitter A, Munro C (1991). Joint moment and muscle power output characteristics of below knee amputees during running; the influence of energy storing feet. J Biomech 24:63-75 Nolan L, Lees A (2000) the kinematic charateristic of above and below knee amputee long jumpers. Ergonomics. 43:16371650. Nolan L (2009) Lower limb strength in sports active transtibial amputees. Prosthetics and Orthotics international. 33:230241 Wetterhahn K, Hansen C, Levy C (2002) effects of participation in physical activity on body image of amputees. Am J Phys Med Rehab 81(3):194-201. Davies D and Datta D (2003) Mobility outcomes following unilateral lower limb amputation. Prosthetics and Orthotics International. 27:16-190. Webster J, Levy C, Bryant P, and Prusakowski P (2001) sports and recreation for people with limb deficiency. Arch Phys Med Rehab 82(3):88-44 Deans S, McFayden A and Rowe P (2008) Physical activity and quality of life: A study of lower-limb amputee population. Prosthetic and Orthotic International 32(2):186-200. Kapp S (2004) Ch 13:Visual analysis of prosthetic gait. In: Atlas of amputated and limb deficiencies: Surgical prosthetic and rehabilitation principles. Rosemont IL. p 385-394. Buckley, J O’Driscoll D, Bennett S (2002) Postural sway and active balance performance in highly active lower limb amputees. Am J phys Med Rehab 81:13-20. Powers C, Boyd L, Fontain C, Perry J (1996). The influence of lower extremity muscle force on Gait characteristics in individuals with Below-knee amputations secondary to vascular disease. Phys therapy 76(4):369-377 Raya M, Gailey R, Fiebert I, Roach K (2010) Impairment Variables Predicting Activity Limitation in Individuals with Lower limb amputation. Prosthetics and orthotics intrnational.34(1):73-84. Gailey R (2003) http://www.oandp.com/articles/2003-12_05.asp accessed 20/3/14