Esophagus
advertisement
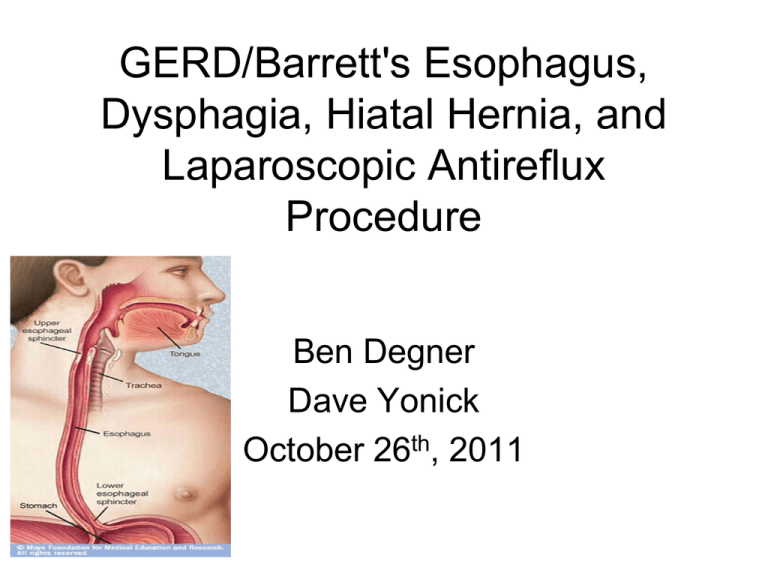
GERD/Barrett's Esophagus, Dysphagia, Hiatal Hernia, and Laparoscopic Antireflux Procedure Ben Degner Dave Yonick October 26th, 2011 Anatomy • Mucosa, submucosa, muscularis propria, and adventitia • Lack serosa vs. other GI tract • Mucosa innermost (4 layers) – contains squamous epithelium Muscularis Propria •Continuation of inferior constrictor of the pharynx •Two muscle bundles •inner circular •outer longitudinal •Striated upper 1/3 -vagus and its recurrent laryngeal branches •Smooth lower 2/3 -visceral nerve plexus derived from neural crest cells •Left vagus anterior-liver/biliary tree •Right vagus posterior-celiac plexus Esophageal Arteries Upper-Inferior Thyroid Artery Lower-Left Gastric and Inferior Phrenic arteries, bronchial arteries and 4-6 aortic branches Esophageal Veins Esophageal Lyphatics Lymphatics: upper 2/3 cephalad, lower 1/3 caudad Anatomy Anatomic Areas of Narrowing • Cricopharyngeal muscle • Left mainstem bronchus and aortic arch • Diaphragm Anatomic Areas of Narrowing UES • 15 cm from incisors • Cricophayrngeus muscle, recurrent laryngeal nerve • Site of perforation is cricopharyngeus muscle (with EGD), aspiration if UES fail • 40 cm from incisors • No anatomic landmarks LES – rise in pressure when transducer is pulled from the stomach • Increased Pressure: Alphaadrenergics, BBs, gastrin, motilin, antacids, cholinergics, metoclopramide • Decreased Pressure: Alpha blockers, Beta andrenergics, CCK, estrogen, glucagon, progesterone, somatostatin, secretin, barbiturates, CCBs, caffeine, diazepam, dopamine, meperidine, ethanol, coffee, fat LES • High pressure except: 1. passage of food into the stomach 2. when fundus is distended with gas, LES eliminated to allow venting of the gas • Loss of the normal high-pressure zone leads to GERD (transient vs permanent) Gastroesophageal Reflux Disease • 1/3 Western population experience symptoms at least once a month • 4-7% daily • Most patients with mild symptoms carry out selfmedication • The prevalence and severity of GERD is increasing Typical GERD Symptoms • Heartburn – substernal burning or chest pain – worse with spicy foods, tomato sauce, citrus juices, chocolate, coffee, and alcohol – 1 to 2 hours after eating, often at night, relieved by antacids and OTC H2 blockers • Regurgitation – sensation that fluid or food is returning into the esophagus – worse at night or when lying down after a meal • Dysphagia – up to 40% of pts with GERD have sensation of food hanging up in the lower esophagus-esophageal dysphagia – typically limited to only solid food, with normal passage of liquids, suggesting mechanical disorder – develops slowly enough that the patient may adjust eating habits unknowingly Atypical GERD Symptoms • Cough, asthma, hoarseness, and noncardiac chest pain • primary complaint in 20-25% • more difficult to prove a causeand-effect relationship • trial of high-dose PPIs is helpful • make sure patient doesn’t have another cause for pain Pathophysiology of GERD • Fundic distention because of overeating • LES is taken up by the expanding fundus, exposing the squamous epithelium/LES to gastric juice – Worsened by delayed gastric emptying with high-fat diet and hiatal hernia • Compensated with increased swallowing – Saliva bathe the injured mucosa and alleviate the discomfort = aerophagia, bloating, repetitive belching • More distension leads to further exposure and repetitive injury to the terminal squamous epithelium leading to inflammation • continued epigastic pain and possibly epithelial columnarization • Extension of the inflammatory process into the muscularis propria – leading to a permanently defective sphincter Diagnosis of GERD • Based on symptoms alone? – Correct in only 2/3 of patients – these symptoms are not specific for GE reflux • achalasia, diffuse spasm, esophageal carcinoma, pyloric stenosis, cholelithiasis, gastritis, gastric or duodenal ulcer, and coronary artery disease – need objective diagnosis before the decision is made for surgical treatment Diagnosis of GERD • First episode – Initial therapy with H2 blockers or PPI for 12 weeks • Failure of H2 blockers or PPI to control the symptoms suggests that either the diagnosis is incorrect or the patient has severe disease EGD – Opportunity for assessing the severity of mucosal damage 24-hour pH and bilirubin monitoring – Measurement degree and pattern of esophageal exposure to gastric and duodenal juice Manometry – Assess the status and function of the LES and esophageal body • • • • These studies identify features that predict a poor response to medical therapy, frequent relapses, and the development of complications Complications of GERD • Mucosal complications-esophagitis and stricture • Extraesophageal or Respiratory complications, such as laryngitis, recurrent pneumonia, and progressive pulmonary fibrosis • Reflux (aspiration) vs reflex (vagal bronchoconstriction) • Metaplastic and Neoplastic complications, Barrett's and esophageal adenocarcinoma • Prevalence/severity of complications related to the degree of loss of the GE barrier and content of refluxed gastric juice, not symptoms Barrett’s Esophagus • Squamous epithelium metaplasia columnar epithelium • 7-10% of patients with GERD • Normally, the SCJ should coincide with the GEJ (linear gastric mucosal folds) • Presence of any columnar mucosa extending at least 3 cm into the esophagus (goblet cells)=Barrett’s – predisposed to malignant degeneration • Increased risk of adenocarcinoma x50 Classification and Management of Barrett’s Esophagus with Dysplasia • Indefinite for Dysplasia: Aggressive antireflux therapy (60 mg PPI per day) and repeated biopsy in 3 months • Low Grade: Aggressive antireflux therapy vs. surgical treatment • High Grade-Esophagectomy and PPI Dysphagia • Difficulty in transferring a food from the mouth to the stomach • Regurgitation, chest pain, heartburn, and coughing or choking spells • Oropharyngeal – functional disturbance in the swallowing mechanism • Esophageal – mechanical obstruction or esophageal motility disorder Dysphagia • Evaluation of a patient with dysphagia must be performed in a systematic manner – Barium swallow • Additional diagnostic tests – EGD, manometry, 24-hour pH study, and possibley bronchoscopy and endoscopic ultrasonography (EUS). – Diagnostic imaging by CT and PET in assessing patients with esophageal cancer Oropharyngeal Dysphagia – inability to chew food, drooling, coughing during a meal, and nasal regurgitation of solids or liquids – dysphagia within 1 second of swallowing • The common causes can be grouped into three broad categories: 1) generalized systemic conditions: CVA, Myasthenia gravis 2) intrinsic functional disturbances: Zenker's diverticulum 3) fixed mechanical obstruction: Neoplasm, webs, previous surgical treatment, previous radiation therapy Esophageal Dysphagia Dysphagia with solids? =Mechanical Obstruction • Intermittent? Esophageal Ring or Esophagitis • Progressive with GERD? Peptic Stricture • Progressive with weight loss and anorexia? Esophageal Cancer Dysphagia for both liquids and solids? =Motility Disorder • Intermittent? Spasm (DES) • Progressive with GERD? Scleroderma • Progressive? Achalasia Schatzki's Ring • symmetrical narrowing at SCJ, small hiatal hernia • correlation with GERD • barium swallow and esophagoscopy to confirm • Asymptomatic? no specific treatment is needed • Definitive treatment? dilatation of the ring with medical therapy for GERD. If refractory, dilatation plus antireflux surgery Peptic Stricture • H/o GERD – worsening dysphagia for years without weight loss • End stage of ulcerative esophagitis, healing ulcer causes annular fibrosis • Dx: barium swallow followed by upper GI endoscopy • greater length and more tapered than Schatzki’s Esophageal Webs • localized narrowing of the esophagus caused by intraluminal extension of the mucosa and part of the submucosa • congenital or acquired (mc), usually secondary to conditions such as iron deficiency anemia/Plummer-Vinson syndrome and ulcerative colitis. • Tx: endoscopic dilatation Achalasia • Dysphagia for liquids and solids and possibly weight loss. • Barium swallow shows absent peristalsis and a dilated esophagus, possibly tapered narrowing in distal esophagus=bird's beak • Achalasia risk factor for squamous cell cancer • Tx: Pneumatic dilatation or surgery Diffuse esophageal spasm • unknown etiology • Nonprogressive dysphagia with solids and liquids and nonexertional chest pain that responds to nitroglycerin • corkscrew on barium • The diagnosis by manometry – periodic occurrence of simultaneous high-amplitude contractions with intervening periods of normal peristalsis. • Tx: r/o CAD, then medical management of reassurance, nitrates, and CCBs • Botulinum toxin injection, surgery does not have an established role Nutcracker Esophagus • unknown etiology • women>men • Manometry: peristaltic waves with significantly elevated amplitude (> 180 mm Hg). • Treatment is primarily medical Hypertensive LES • unknown etiology • can occur alone or in association with achalasia, nutcracker esophagus, or DES • Manometry-LES pressure over 45 mm Hg • Tx: primarily medical, but balloon dilatation is done Esophageal Diverticula • < 5% of all cases of dysphagia. • False diverticula (pulsion) include only the mucosal layer – underlying motor dysfunction • True diverticula (traction) include all layers of the esophageal wall – inflammatory process • Esophageal diverticula may also be classified into three categories on the basis of the anatomic level at which they occur Pharyngoesophageal/Zenker’s Diverticula • MC • from muscle incoordination that leads to herniation of the mucosa in prox esophagus • Dysphagia mc symptom, halitosis, regurgitation, throat discomfort, palpable neck mass, recurrent aspiration pneumonia • The best initial diagnostic tool is a barium swallow • perforation in EGD Midesophageal diverticula • True traction diverticula • Caused by periesophageal inflammation in granulomatous inflammation of the subcarinal lymph nodes from TB or fungal infection • Frequently asymptomatic and are often found incidentally • Dysphagia does occur but is a rare symptom Epiphrenic diverticula • Acquired pulsion diverticula of distal esophagus • Associated with other esophageal motor disorders (achalasia, DES, and hypertensive LES) but can occur alone • Absent or mild symptoms? – Conservative management is appropriate • Significant dysphagia? – Surgical management Chemical Ingestion • Alkali household cleaning agents • Most occur accidentally in children, but suicide in adults • Magnitude and site of the injury? – Related to the length of the contact time – Injury at any level, MC is distal esophagaus • lead to submucosal scar formationstricture and dysphagia • Endoscopic exam is first step • A barium swallow should be done in the first month after injury to detect any stricture and then serial swallows Hiatal Hernia I-Sliding, dilation of hiatus, most commonly associated with GERD -most with reflux have sliding, most with sliding don’t have reflux II-Paraesophageal, defect in diaphragm alongside esophagus with normal GE junction --chest pain, dysphagia, early satiety III-Combined I and II IV-entire stomach in chest plus another organ (colon, spleen) Laparoscopic Antireflux Procedure • Most commonly performed procedure is a fundoplication • Nissen Fundoplication: 360 degree fundoplication • Laparoscopic approach reduces postoperative pain and shortens length of hospital stay – Rapid increase in surgical treatment of GERD • Preoperatively – h/o recurrent heartburn enough to clinically establish GERD and initiate empiric medical therapy – Those patients with recurrent or refractory symptoms require further evaluation prior to surgery • Endoscopy – Evaluate for Barrett’s Esophagus • Manometry – Evaluate for other causes of esophageal dysmotility • 24 hour pH – May be helpful, especially in those patients with atypical GERD symptoms or other GI comorbidities • Indication – Failure of maximal medical therapy • Short 2 month trial – Failure of lifestyle modification • Weight loss • Alteration in diet (avoid chocolate, peppermint, fat, onions, garlic, alcohol, caffeine, nicotine) • Avoid food 2-3 hours prior to sleep • Elevation of head of bed 6 – 10 inches • Limit potentially precipitating activities (bending over or strenuous exercise) – Complications of GERD • Esophagitis, stricture, recurrent aspiration or pneumonia, Barrett’s esophagus – Associated with paraesophageal hernia – Intolerance to medical therapy or patient desiring discontinueation of medical therapy • Contraindication – Absolute • Inability to tolerate general anesthetic or laparoscopy • Uncorrectable coagulopathy – Relative • • • • • Previous upper abdominal surgery Morbid obesity Severe esophagitis with or without stricture Small-body habitus Short esophagus – Particularly for fundoplications • Paraesophageal hiatal hernia • Basic tenets of antireflux surgery – Restoration of an effective LES – Creation of a gastroesophageal valve – Mechanical effects of a fundoplication • Fundus exhibits a physiologic phenomenon of receptive relaxation – Decreased tone of the gastric fundic smooth muscle in association with swallowing-induced relaxation of the LES Laparoscopic Port Placement Belsey Mark IV Repair • Transthoracic repair to control GERD • Typically performed through a left thoracotomy – May be performed thoracoscopically • McKernan and Champion modified Belsey • Distal esophagus and proximal stomach are mobilized and ddelivered through the esophageal hiatus • Anterior 270 degree plication of the fundus is performed onto the esophagus • The fundoplication is buttressed by the diaphragmatic crura Nissen Fundoplication • 360 degree wrap around esophagus – – – – Circumferentially dissecting the distal esophagus Mobilizing the gastric fundus Plicating the fundus around the lower esophagus Creating a high-pressure zone • Increases the resting tone of the sphincter mechanism • Improves its response to elevated intragastric pressure – Fundoplication varied from 3 – 6 cm and included the esophageal wall in the fundoplication – No division of the short gastric vessels • Rossetti-Hell modification – Included wrapping the anterior portion of the fundus around the esophagus – No division of the short gastric vessels – Minimal moblization of the upper stomach – Created a 3 – 6 cm 360 degree fundoplication • Short, floppy Nissen – Most common modification used today – The short gastric vessels are divided – Full fundic mobilization and the lateral border of the fundus is wrapped around the esophagus • Sutured to the medial edge of the medial fundus – Short fundoplication, < 2.5 cm – Fashioned over a 50 to 60F bougie • Complication of total fundoplication – Dysphagia – Inability to belch – Gas-bloat syndrome – Hypercontinent Partial Fundoplication • Indication – Poor esophageal clearance because of esophageal motility abnormality – Severe aerophagia, daytime reflux associated with belching – Insufficient gastric fundus • Previous gastrectomy • Tubular stomach – Psychological inability to tolerate side effects of fundoplication – Association with Heller myotomy for achalasia • Dor Fundoplication – 180 to 200 degree anterior wrap – Used in association with Heller esophagomyotomy for achalasia • Watson fundoplication – Plication of the fundus along the left anterolateral border of the esophagus • More physiologic • 120 degree anterolateral wrap • Toupet fundoplication – Most common partial fundoplication laparoscopically – 270 degree posterior wrap – Fundus pulled posterior to esophagus with suture of leading edge to right anterior aspect of the esophagus Hill Repair • Indication – Reflux symptoms refractory to medical management – Younger patients asymptomatic but requiring high-dose medication • Avoid lifetime dependence on medication – Chronic esophagitis, inflammatory shortening of the esophagus and paraesophageal hernia • Advantage – Posterior fixation of GE junction • Prevent recurrent herniation and improve distal esophageal clearance by improving longitudinal function – Distal high-pressure zone can be calibrated; avoiding late dysphagia – Does not require a gastroplasty with a short esophagus – Can be preformed in patients that have undergone a gastrectomy – Shorter hospital stay and faster recovery compared to open procedure • Contraindication – Morbid obesity – Failed previous antireflux operation – Prior extensive upper abdominal surgery • Pre-operative – Endoscopy • Evaluate for Barrett’s esophagus • Evaluate and grade gastroesophageal valve – Grade I: normal musculomucosal valve – Grade II: valve that is slightly less defined and shorter than Grade I – Grade III: valve is poorly defined; stays open, allows reflux and is associated with a hiatal hernia – Grade IV: no definition to the musculomucosal fold; stays open constantly and is associated with a hiatal hernia – Manometry • Evaluate for Motility disorder – 24 hour pH study • Evaluate and confirm the diagnosis of GERD • Hill Repair – A 43F bougie is passed through the GE junction along with a manometry probe during the repair. – Intraoperative manometry is performed to calibrate the GE junction • Reconstructed LES is approximately 3 to 4 cm • Peak pressure during pull through > 45 mm Hg than sutures are loosened • Peak pressure < 20 mm Hg, sutures are tightened – Following calibration; sutures are fixed permanently over a bougie – Fundus is secured to the rim of the diaphragm • Accentuate the angle of His and elongate the gastroesophageal flap valve Failed Fundoplication • Learning curve requires 30 to 50 operations – Decreasing operative time – Diminishing rates of complications • Dysphagia – Excessively tight closure of the esophageal hiatus • Tight wrap or tension on the wrap • Sliding hiatal hernia with wrap in abdomen • Migration of the wrap into the mediastinum – Most common complication – New-onset substernal or epigastric pain • Slipped Nissen – Secondary to disruption or migration of the wrap onto the stomach Questions A 55-year-old man with chronic gastrointestinal reflux undergoes upper endoscopy and is found to have a 4cm segment of Barrett’s esophagus. Biopsy of the lesion is positive for low-grade dysplasia. Current surveillance recommendations include fourquadrant biopsies every: A) 3 months B) 6 months C) 9 months D) 12 months E) 24 months A 55-year-old man with chronic gastrointestinal reflux undergoes upper endoscopy and is found to have a 4-cm segment of Barrett’s esophagus. Biopsy of the lesion is positive for low-grade dysplasia. Current surveillance recommendations include four-quadrant biopsies every: A) 3 months B) 6 months C) 9 months D) 12 months-every 2 cm along the length of the Barrett’s segment E) 24 months A 47-year-old woman has acid reflux that has not responded to therapy with proton pump inhibitors. Her body mass index (BMI) is 43 and she is hypertensive and diabetic. Upper endoscopy reveals grade 1 esophagitis. Esophageal manometry shows good progression of peristalsis with normal lower esophageal sphincter (LES) tone and relaxation. The procedure MOST likely to help this patient overall would be: A) total fundoplication B) partial fundoplication C) gastric bypass D) endoscopic antireflux procedure E) vertical banded gastroplasty A) total fundoplication B) partial fundoplication C) gastric bypass D) endoscopic antireflux procedure E) vertical banded gastroplasty -GERD is seen in up to 72% of obese persons -GERD is usually only one of many co-morbidities in obese: OSA, HTN, DM, HL -Fundoplication directed solely at treating GERD does not adequately address the underlying cause, nor does it do anything to help with the other comorbid conditions -A bariatric procedure allows for weight loss and improvement or resolution of other associated Conditions including GERD A 42-year-old man has had a long history of gastroesophageal reflux disease (GERD). He has attempted many medication trials, with only minimal relief. A recent endoscopy revealed grade II esophagitis. He is considering surgery. Which of the following studies should be performed before performing a laparoscopic fundoplication? A. Barium swallow B. Esophageal manometry C. Ambulatory pH monitoring D. All of the above A 42-year-old man has had a long history of gastroesophageal reflux disease (GERD). He has attempted many medication trials, with only minimal relief. A recent endoscopy revealed grade II esophagitis. He is considering surgery. Which of the following studies should be performed before performing a laparoscopic fundoplication? A. Barium swallow B. Esophageal manometry C. Ambulatory pH monitoring D. All of the above -All candidates for a laparoscopic Nissen fundoplication should undergo a preoperative evaluation that includes symptomatic evaluation, barium swallow, endoscopy, esophageal manometry, and ambulatory pH monitoring. -Ambulatory pH monitoring is the most reliable test for the diagnosis of GERD; it has a sensitivity and specificity of about 92%. A 60 year-old otherwise healthy man has symptomatic GERD that has not responded to medical therapy, including PPIs. Esophagoscopy shows moderately severe esophagitis. Multiple biopsies of the esophageal mucosa in the area of esophagitis show columnar epithelium replacing the normal squamous epithelium. As the patient’s treatment is being planned, a biopsy report shows highgrade dysplasia. Treatment should be: A. Continued medical treatment with yearly esophagoscopy and biopsies B. Laparoscopic Nissen fundoplication C. Photodynamic therapy D. Esophagectomy E. Laser ablation of normal mucosa A 60 year-old otherwise healthy man has symptomatic GERD that has not responded to medical therapy, including PPIs. Esophagoscopy shows moderately severe esophagitis. Multiple biopsies of the esophageal mucosa in the area of esophagitis show columnar epithelium replacing the normal squamous epithelium. As the patient’s treatment is being planned, a biopsy report shows highgrade dysplasia. Treatment should be: A. Continued medical treatment with yearly esophagoscopy and biopsies B. Laparoscopic Nissen fundoplication C. Photodynamic therapy D. Esophagectomy E. Laser ablation of normal mucosa Four years ago, a 47 year-old woman had a laparoscopic fundoplication. It failed after three years and she had severe, recurrent gastroesophageal symptoms. Through a celiotomy incision, the surgeon performed a redofundoplication with a 360-degree, 2 cm wrap around a 56 Fr dilator. For the past three months she has had severe early satiety, postprandial epigastric pain, and weight loss. The most likely cause of these symptoms is: A. The wrap is too tight B. The wrap is too loose C. Vagal injury D. Irritable bowel syndrome E. Esophageal motor disorder Four years ago, a 47 year-old woman had a laparoscopic fundoplication. It failed after three years and she had severe, recurrent gastroesophageal symptoms. Through a celiotomy incision, the surgeon performed a redofundoplication with a 360-degree, 2 cm wrap around a 56 Fr dilator. For the past three months she has had severe early satiety, postprandial epigastric pain, and weight loss. The most likely cause of these symptoms is: A. The wrap is too tight B. The wrap is too loose C. Vagal injury D. Irritable bowel syndrome E. Esophageal motor disorder Barrett’s esophagus: A) will usually regress after Nissen fundoplication B) carries an increased risk of squamous cell carcinoma C) is an indication for esophagectomy D) should be followed by endoscopic surveillance E) is a contraindication to laparoscopic Nissen fundoplication Barrett’s esophagus: A) will usually regress after Nissen fundoplication B) carries an increased risk of squamous cell carcinoma C) is an indication for esophagectomy D) should be followed by endoscopic surveillance E) is a contraindication to laparoscopic Nissen fundoplication A 47-year-old woman presents with a 1- to 2-month history of postprandial, mild epigastric pain on swallowing solid food. The x-rays shown are obtained. What is the diagnosis and which of the following is appropriate for this patient? A) Esophageal lengthening procedure B) Observation C) Partial gastrectomy D) Stamm gastrostomy E) Surgical reduction A 47-year-old woman presents with a 1- to 2-month history of postprandial, mild epigastric pain on swallowing solid food. The xrays shown are obtained. Which of the following is appropriate for this patient? A) Esophageal lengthening procedure B) Observation C) Partial gastrectomy D) Stamm gastrostomy E) Surgical reduction of the hernia -the chest x-ray suggests a paraesophageal hernia What indicate(s) presence of hiatal hernia? A) Distal esophageal web B) Cervical esophageal web C) Both D) Neither What indicate(s) presence of hiatal hernia? A) Distal esophageal web B) Cervical esophageal web C) Both D) Neither Distal esophageal web, or Schatzki’s ring, is an annular constriction of the esophagus that indicates the presence of a sliding hiatal hernia. Plummer-Vinson syndrome is cervical esophageal dysphagia associated with iron-deficiency anemia. The condition is commonly associated with cervical esophageal webs. Plummer-Vinson syndrome is considered a premalignant condition; 10% of patients develop SCC of hypopharynx, oral cavity, or esophagus. Treatment: of correction of iron deficiency and dilation of cervical webs Gastroesophageal reflux disease increases risk developing of: A) Adenocarcinoma of the esophagus B) Squamous cell carcinoma of the esophagus C) Both D) Neither Gastroesophageal reflux disease increases risk developing of: A) Adenocarcinoma of the esophagus B) Squamous cell carcinoma of the esophagus C) Both D) Neither -SCC related to lye ingestion, achalasia and EtOH and tobacco -Adenocarcinoma now MC esophageal cancer, related to GERD Regarding the anatomy of the esophagus: A) the cervical esophagus lies to the right of the midline B) the thoracic esophagus is anterior to the aortic arch C) the left vagus nerve passes posterior to the esophagus D) the cervical esophagus is supplied by the inferior thyroid artery E) the abdominal esophagus is supplied by the right gastric artery Regarding the anatomy of the esophagus: A) the cervical esophagus lies to the right of the midline B) the thoracic esophagus is anterior to the aortic arch C) the left vagus nerve passes posterior to the esophagus D) the cervical esophagus is supplied by the inferior thyroid artery E) the abdominal esophagus is supplied by the right gastric artery