Study Finding - Asociatia AntiParkinson
advertisement
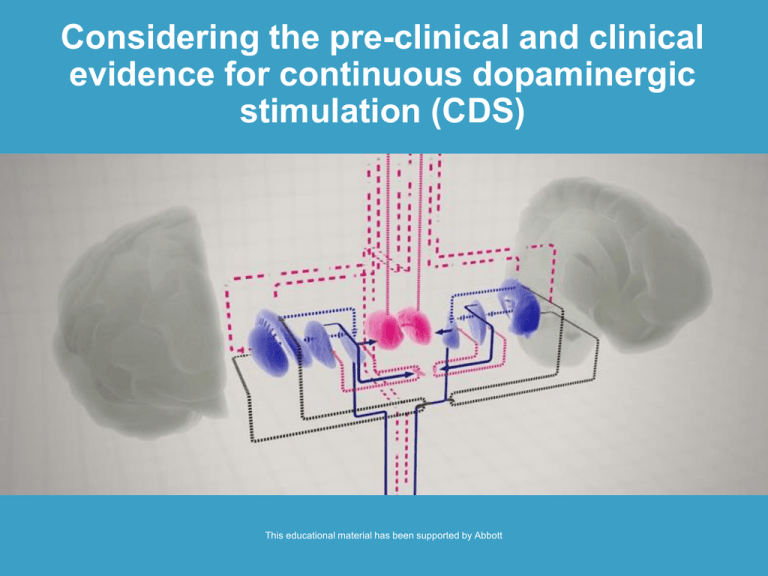
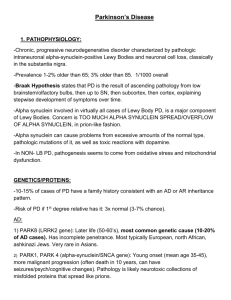
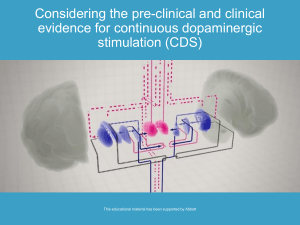
Considering the pre-clinical and clinical evidence for continuous dopaminergic stimulation (CDS) This educational material has been supported by Abbott Considering the pre-clinical and clinical evidence for continuous dopaminergic stimulation (CDS) Motor fluctuations and dyskinesias: what have we learned from the laboratory? <<Insert speaker’s name and affiliation>> Learning objectives At the end of this section you will have: • An understanding of the animal models that have been developed to study motor complications in Parkinson’s disease • Greater knowledge of the mechanisms underlying motor fluctuations and dyskinesias in Parkinson’s disease Animal models of motor complications in Parkinson’s disease Model Physiological effect Behavioural effects Rodent 6-OHDA lesion (unilateral intracerebral injection) Selective permanent dopaminergic depletion of the nigrostriatal pathway • Unilateral dopamine denervation causes motor deficits in the contralateral limbs and postural asymmetry, mimicking Parkinson’s disease • Levodopa treatment improves these deficits but also causes AIMs mimicking dyskinesia. In most (but not all) rodent models, levodopainduced AIMs are accompanied by contralateral rotation Non-human primate MPTP-treated Metabolite (MPP+) is taken up by the dopamine transporter and inhibits complex I of the mitochondrial respiratory chain • Bradykinesia, rigidity, and postural deficits similar to Parkinson’s disease • Levodopa improves motor performance and reduces disability • Chronic intermittent levodopa treatment leads to AIMs (dyskinesia) AIMs = abnormal involuntary movements 6-OHDA = 6-hydroxydopamine MPTP = 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine; MPP = 1-methyl-4-phenylpyridinium Adapted from: Chapter 1: The continuous dopaminergic stimulation concept and evidence to date. M Maral Mouradian. Managing Advanced Parkinson’s Disease: The role of continuous dopaminergic stimulation. Aquilonius and Lees (Ed). 2007. Pre-clinical studies of motor complications Dopamine denervation is necessary for the occurrence of motor complications Study Finding Papa et al, 1994 • Rats with 95% dopamine neuron loss due to 6-OHDA lesions manifest ‘wearing-off’, while rats with less severe lesions do not Di Monte et al, 2000 • Moderate nigrostriatal denervation (60-70% striatal dopamine depletion) in MPTP treated primates led to levodopa-induced dyskinesias; the severity of the lesions’ enhanced sensitivity to levodopa Winkler et al, 2002 • Intrastriatal 6-OHDA-lesioned rats exhibited a lower predisposition to levodopa-induced dyskinesia than rats with complete bundle lesions • Selective and partial denervation in the sensorimotor part of the striatum can confer cellular and behavioural supersensitivity to levodopa Paillie et al, 2007 • Levodopa given twice daily caused dyskinesias in bilateral 6-OHDA lesioned rats • Dyskinesia severity correlated with extent of dopamine neuron loss increasing abruptly when neuron loss approached 75% Papa SM, et al. Brain Res 1994;662(1-2):69-74. Di Monte DA, et al. Mov Disord 2000;15(3):459-66. Winkler C, et al. Neurobiol Dis. 2002;10(2):165-86. Paillie V, et al. Mov Disord. 2007;22(4):533-9. Pre-clinical studies of motor complications Pulsatile levodopa treatment is a cause of motor complications Study Finding Juncos et al, 1989 • 30-day intermittent levodopa, but not continuous levodopa treatment, produced behavioural sensitisation in 6-OHDA rats Bibbiani et al, 2005 • Continuous apomorphine infusion improved motor function in primates for up to 6 months without dyskinesias • Intermittent apomorphine produced dyskinesias within 7-10 days of treatment Blanchet et al, 2001 • • Schmidt et al, 2008 • • Dyskinesias <10 days of intermittent dopaminergic treatment in MPTP-treated primates Only 3 of 6 primates developed dyskinesias with continuous dopaminergic stimulation, but complications diminished in intensity In unilateral 6-OHDA lesioned rats, pulsatile levodopa injections (1-2/day) caused contraversive rotations and AIMs Pulsatile (1-2/day) injections of the dopamine agonist rotigotine resulted in more contraversive rotations than a slow release formulation Stockwell et al, 2009 • Continuous rotigotine delivery (via osmotic minipump) produces less dyskinesias than pulsatile rotigotine administration (twice daily) in MPTP-treated primates Stockwell et al, 2010 • Switching from pulsatile levodopa or rotigotine administration to continuous rotigotine infusion reduced the severity and duration of dyskinesias in primates Juncos JL, et al. Ann Neurol 1989;25(5):473-8. Bibbiani F, et al. Exp Neurol 2005;192(1):73-8. Blanchet PJ, et al. Adv Neurol 2001;86:337-44. Schmidt WJ, et al. J Neural Transmiss 2008;115(10):1385-92. Stockwell KA, et al. Exp Neurol 2009;219(2):533-42. Stockwell KA, et al. Exp Neurol 2010;221(1):79-85. A primate model of motor complications Effect of continuous versus intermittent dopaminergic treatment Reproduced from Exp Neurol 2005;192(1) Bibbiani F, et al. Continuous dopaminergic stimulation reduces risk of motor complications in parkinsonian primates. p 73-8, Copyright (2005) with permission from Elsevier. The development of pulsatile levodopa-induced dyskinesias Study background • Unilateral 6-OHDA in the nigrostriatal fibre bundle • Severe (> 90%) striatal dopamine denervation • Daily levodopa injections for 2-3 weeks • Peak-dose abnormal involuntary movements (AIMs) Dyskinetic [movie] Permission kindly granted by Dr Angela Cenci-Nilsson. Non-dyskinetic [movie] Potential mechanisms underlying pulsatile levodopa-induced dyskinesias Large peaks-and-troughs of extracellular dopamine: • Rise and decline of levodopa and dopamine levels in the striatal extracellular fluid correlate with the timing of AIMs • Larger increases in striatal levodopa and dopamine in dyskinetic 6-OHDA lesioned rats than in non-dyskinetic animals • Chronic levodopa treatment may alter dopamine regulation and metabolism in striatum and may lead to treatment-related adaptations Serotonergic system: • Treatment with serotonin autoreceptor agonists blunts the peak in extracellular dopamine levels in dyskinetic rats • Removal of serotonin afferents blocks levodopa-induced dyskinesias in 6-OHDA lesioned rats • Thus, dysregulated dopamine release from serotonergic neurons likely play a key role in dyskinesia development Cenci MA, Lundblad M. J Neurochem 2006;99(2):381-92. Lindgren H et al. J. Neurochem 2010;112(6):1465-76. Carta M, et al. Brain 2007;130(7):1819-33 . Serotonergic involvement in pulsatile levodopa-induced motor complications Levodopa-induced rat AIMs are abolished by dampening of serotonin neuron activity† † Similar study carried out in primates by Munoz et al * = significant versus sham/vehicle Carta M, et al. Dopamine released from 5-HT terminals is the cause of L-DOPA-induced dyskinesia in parkinsonian rats. Brain 2007;130(Part 7):1819-33, reproduced with permission of Oxford University Press. †Munoz A, et al. Combined 5-HT1A and 5-HT1B receptor agonists for the treatment of L-DOPA-induced dyskinesia. Brain 2008;131(2):3380-94. Abnormal molecular responses to levodopa in striatal neurons in dyskinetic animals Dyskinetic rat Non-dyskinetic rat ERK1/2: extracellular signalregulated kinases 1 and 2. Phospho-ERK1/2 (15 min to 2 h post-dosing) Master regulator of neuronal plasticity. Become active when phosphorylated on specific amino acid. ∆FosB (2 h to >2 weeks post-dosing) ERK 1/2 MSK-1 PDyn Prodynorphin mRNA (3 h to >2 weeks post-dosing) Elk1 ∆FosB Causes changes in gene expression (via transcription factors and histone kinases) and changes in protein translation (via the mTOR pathway) ∆FosB: nuclear transcription factor Prodynorphin: effector gene (codes a neurotransmitter precursor) Cenci MA, et al. Eur. J. Neurosci 1998;10(8):2694-2706. Andersson M, et al. J. Neurosci 2001;21(24):9930-9943. Andersson M, et al. Eur. J. Neurosci 2003;17(3): 661-666. Westin JE et al. (2007) Biol. Psychiatry 62: 800-810. Aubert I, et al. Biol Psychiatry 2007;61:836-44. Santini E, et al. Sci Signal 2009;21(2):ra36. (Images developed under the guidance of Dr Angela Cenci Nilsson). Enhanced response to dopamine Pulsatile dopaminergic stimulation leads to downstream changes in striatal dopamine neurones Aetiology of dyskinesias: what we have learned from the laboratory Adapted from Thanvi B, et al. Postgrad Med J 2007;83:384-88 Aetiology of ‘wearing off’: what we have learned from the laboratory Nigrostriatal pathology Reduced dopamine storage capacity ‘Wearing-off’ (also postsynaptic changes can be important) early: several days effect late: only hours effect of oral levodopa Mechanisms of levodopa-induced dyskinesia and clues to treatment Dopaminergic denervation Loss of nigrostriatal dopamine storage capacity Dopamine release from serotonin terminals Dopamine-R supersensitivity Drugs acting on postsynaptic receptors and/or signaling pathways (e.g. mGluR5 antagonists) Deep brain stimulation Large intermittent surges of extracellular dopamine 5HT1A and 1B agonists Abnormal signaling in striatal D1R-rich GABA+, Dyn+ neurons Altered firing patterns in GPi/SNr Adapted from Cenci MA. Parkinsonism Relat Disord 2007;13 (Suppl 3):S263-7 Levodopa treatment Pulsatile drug delivery Microvascular remodeling New levodopa delivery methods (duodenal delivery; gene therapy) Summary • Pre-clinical studies have identified the potential mechanisms involved in the development of motor complications observed in patients with Parkinson’s disease • In rodents and primates, the ‘wearing off’ phenomenon and dyskinesias are apparent with intermittent dopaminergic administration • Basal ganglia undergo plastic changes following denervation and long-term pulsatile dopaminergic exposure • These changes are at least partly reversible upon switching from pulsatile to continuous drug delivery