MJFF_PET-imaging-levodopa-dyskinesias-v8
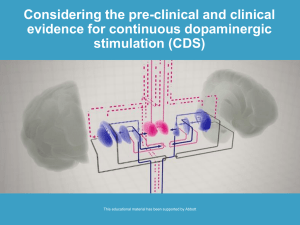
advertisement

The Idea We outline a study to develop a new PET imaging-based predictor of the onset of dyskinesia from levodopa therapy for Parkinson’s disease (PD). Dyskinesias are a debilitating complication of levodopa therapy that affect many PD patients but there is no clear means of identifying patients who are likely to develop them. What causes dyskinesias? Preliminary work by researchers using PET [1, 2] suggests dyskinesias are related to overly rapid but poorly sustained production of dopamine (DA) from levodopa. These findings highlight the need for observing dysregulated levodopa-induced DA release in finer temporal detail. Recent work by the PI has lead to novel PET image analysis techniques for observing drug-induced DA changes ( “DA signatures”) with minute-scale temporal resolution. We propose a pilot study to apply the PI’s new methods to PET studies of PD patients after levodopa and to identify the aspects of the DA signature that are associated with dyskinesias. A reliable means of identifying patients who are at risk of developing levodopa-induced dyskinesias (LID) would greatly improve PD treatment management. Need for predictors of response to PD therapies: The most common pharmacological treatment for PD is DA replacement therapy (DRT) with carbidopa/levodopa. While effective for motor symptoms, DRT may result in severe motor side-effects, such as LID. Impact Motor complications are common, affecting up to 20% of all PD patients treated by specialists at the Yale Movement Disorders Clinic over the last 5 years. Ultimately, 90% of PD patients on levodopa experience LID within 10 Figure 1. Bars represent amount of DA, by displacement of tracer, at 1 and years of treatment [5]. Today, there is no reliable way to measured 4 hrs post levodopa in caudate of stable anticipate which patients will proceed to these complications. responders (white) and dyskinetics (black). Imaging-based early predictors of poor response to Data are from[1]. Blue and red curves our speculation - based on the two therapy would greatly aid the management of treatment represent time points measured - what the continuous DA response curves (blue – stable; red – as well as inform our understanding of the disease. What do we know from imaging? PET imaging at the dyskinetics) might look like in each group. University of British Columbia (UBC) [1] suggests that the post-levodopa DA signatures of patients with PD are different in patients who have developed clinically significant dyskinesias than in those who have not. Using the DA D2/D3 tracer [11C]raclopride (RAC), striatal DA levels in vivo were assayed with PET by comparing the amount of blockade of the tracer before and (1 or 4 hrs.) after levodopa. Blockade of RAC by endogenous DA appeared more stable and longlasting in patients who were free of LID. Blockade is measured as change in binding potential (BP) - an estimate of the steady state ratio of bound to free RAC[6, 7]. An added appeal of the UBC work is that a cohort of patients in the early stages of PD were scanned before any had developed LID. Short-lived DA release was predictive of LID in 3 of 4 patients at follow-up after 3 years[8]. Fig. 1 shows the data from the UBC study. On top of their data we have superimposed curves representing our speculation as to what the time-courses for each group (stable responders to levodopa vs. dyskinetics) might be. With only two time points measured (each an average over an hour-long scan) it is not possible to know what is happening on a finer time-scale. Extrapolating from two time-points to a continuous DA response curve is even more difficult than one might imagine. As we have demonstrated elsewhere [9-11], BP, the conventional index of DA release used by the UBC team, can be biased by the particular temporal pattern of DA release. Under some circumstances, a larger amount of DA released spread over a longer period could cause a smaller change in BP than a lesser amount of DA released over a shorter period. A given amount of DA release yields less change in RAC BP if it occurs in the latter part of the PET scan. Thus, stable responders and dyskinetics might have identically shaped DA signatures but the brains of stable responders may delay their responses. 0 A second PET-raclopride study of DA in LID took an inventive approach to delayed responses[2]. Researchers at Hammersmith Hospital (HH) determined how long it took each patient to turn “on” after taking levodopa. Subjects were then scanned beginning at their individual “on” time. If responses of all patients were otherwise identical save for a time-delay, the resulting changes in BP would have been the same for all. The HH group found that despite their individualization of scans, shorter “time to on” correlated with larger changes in BP. Whatever the exact explanation, it is clear from the UBC and HH studies that the pattern and amount of DA released by PD patients post-levodopa are intertwined and a new method of analysis is needed to tease them apart to identify key aspects of the response most relevant to LID. Newly established techniques lend in-depth view of DA response to drugs: The PI and collaborators have recently developed ntPET - a suite of image analysis techniques designed to extract detailed information on DA dynamics from a series of RAC scans with and without challenge [3, 4, 11-14]. This type of analysis has not been accomplished previously, and no other existing noninvasive technology appropriate for human use offers an estimate of the temporal Fig 2. DA signature (blue) calculated by behavior of DA. We have demonstrated that ntPET applied ntPET model from RAC PET study of rat to simultaneous microdialysis to PET scans of rats produced estimates of the striatal DA compared (red) in striatum of rat following signature that agreed well with the ‘gold standard’, direct methamphetamine challenge. Data from [4]. intracranial measurements via microdialysis [4] (see Fig 2). We have also introduced voxel-by-voxel images that capture the spatio-temporal pattern of DA action throughout the striatum [3, 12, 13]. Such images were validated in our most recent paper. Fig. 3 shows two images of the time-of-maximal DA, Tmax(DA), of a person performing a cued motor task at two separate times[3]. If ntPETbased characterization the DA response to levodopa in PD patients could predict therapy outcome, it would have direct clinical relevance. Hypothesis and Objectives We hypothesize that striatal DA signatures and Tmax(DA) images will Fig 3. Tmax(DA) images of the striatum for a research performing a motor task early (left) or late (right) differ between PD patients with and without subject during a RAC PET scan. Hotter colors (scale bar at right complications of therapy and thus may be clinically represents minutes) indicate that maximal release of DA valuable as indices/predictors of risk LID associated occurs later when a DA-ergic motor task is performed later. Data from[3]. with DRT. This study is designed to acquire key pilot data to evaluate the DA signature in complications of DRT through the use of newly validated techniques. Objective 1. To recruit 6 PD patients in two groups (on levodopa therapy who do/ do not suffer dyskinesias); to characterize the severity of their disease and complications of treatment, and to scan them with PET and RAC pre- and post levodopa challenge. Objective 2. To generate detailed DA signatures (ala Fig 2) in striatal brain regions and Tmax(DA) images (Fig 3) in both cohorts and to correlate these quantitative characteristics of the DA response to levodopa with the presence and severity of dyskinesia. The Study Recruitment: Two cohorts of idiopathic PD patients, as defined by the United Kingdom Parkinson’s Disease Brain Bank Diagnostic Criteria, on levodopa will be recruited. All subjects will have been on a stable drug regimen for at least 4 weeks. Subjects will be divided into two groups: 1) those with LID as determined using the Unified Parkinson Disease Rating Scale (UPDRS) Part IV, and 2) those without any complications of levodopa therapy. 1 Groups will be matched for disease severity according to the Hoehn and Yahr Staging of PD, UPDRS Parts I-III, duration of disease, sex, duration of DRT and levodopa equivalent daily dose (LEDD) [15]. Feasibility: The Yale Movement Disorders Clinic sees over 400 PD patients per year and the number in their PD database continues to grow. Scanning Protocol: Subjects will undergo three RAC PET scans in two days. Subjects will stop taking levodopa beginning the evening prior to their scan session and will be off this medication for at least 12 hours by the scan start. All scans will be 2 hrs in duration. The ‘baseline’ scan will be conducted one morning and will commence with a bolus injection of RAC. ‘Challenge’ scans will be performed on a separate morning. The first of the two challenge scans (c1) will commence with oral administration of 25 mg carbidopa/250 mg levodopa. Patients will receive their challenge dose 15 min prior to start of c1. The second post-challenge scan (c2) will be performed (with only a short break) following c1. The second injection is required due to the short halflife of 11C (20 min). Each injection of RAC will be a minimum of 10 mCi with minimum specific activity of 0.75 mCi/umol at time of injection. Scan days will be randomized. All scans will be conducted on the Siemens High Resolution Research Tomograph (HRRT). Hardware motion correction will be performed on an event-by-event basis. The HRRT’s 2-3 mm resolution will allow us to look for distinct DA signatures within substructures (e.g., dorsal and ventral striatum) and to create high resolution Tmax(DA) images. Data Analysis: Using ntPET, each of the two scans acquired following levodopa challenge will be analyzed in combination with the baseline (b) scan separately (i.e., b+c1, b+c2) to produce regional and voxel-wise DA signatures for a 4 hr period following levodopa. The DA take-off and peak times from the resulting extended DA signature will be correlated with LID severity to determine which aspects of the DA signature and Tmax(DA) images are most closely associated with a good or bad response to DRT. Based on the UBC and Hammersmith findings, we hypothesize that short and abrupt DA signatures, characterized by early DA take-off and peak-times, will be associated with the most severe cases of LID, whereas the most prolonged and slowly-changing DA signatures will correlate with absence of LID. Although it is difficult to predict the appearance of the Tmax(DA) images based on current knowledge, it is reasonable to expect that the cluster of early-peaking voxels (low values on the Tmax(DA) image) will be larger in more severe cases of LID. We will also examine the laterality of the Tmax(DA) images as an indicator of the status/progression of LID. Timeline: 6 Patients will be recruited in 2 months and scanned within the following 4 months. Data will be analyzed and interpreted within 4 months and results will be written up and used to apply for future large-scale funding within the year. Note: Two contiguous injections of RAC post-levodopa are likely to be more sensitive to DA changes than one bolus of a slower tracer, e.g., [18F]-fallypride or [18F]FLB (see [9]). Budget: RAC scans at Yale (no blood sampling or metabolite processing) cost $3300 (includes tracer synthesis, scan, image reconstruction and basic analysis for BP (ala UBC and HH groups) but not the advanced ntPET processing above). The PI will devote 1% effort; a grad student will run the studies and produce DA signatures and Tmax(DA) images (5.5% effort). The Team Dr. Morris is an experienced modeler of PET imaging data. He is the principal inventor of ntPET analysis. He is Co-director for Imaging at the Yale PET ce nter. The Yale PET facility is one of the most active centers for brain imaging in the world (12-20 research scans per week). It has 2 human scanners, and an incomparable battery of over 30 tracers in use (including RAC). As a co-director, Morris has direct input into scheduling scanners and resources needed to ensure completion of the project. Dr. Machado, a movement disorders neurologist, saw approximately 150 PD patients at Yale New Haven Hospital last year. Dr. Vives, chief of Stereotactic and Functional Neurosurgery, has been treating PD patients with deep brain stimulation and other therapies for 8 years. He is active in NIH-funded research on alternative PD therapies. Vives and Machado will recruit and evaluate patients, and advise the PI. 2 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. de la Fuente-Fernandez, R., et al., Levodopa-induced changes in synaptic dopamine levels increase with progression of Parkinson's disease: implications for dyskinesias. Brain, 2004. 127(Pt 12): p. 2747-54. Pavese, N., et al., Clinical correlates of levodopa-induced dopamine release in Parkinson disease: a PET study. Neurology, 2006. 67(9): p. 1612-7. Morris, E.D., et al., Noninvasive visualization of human dopamine dynamics from PET images. Neuroimage, 2010. Available online. Morris, E.D., M.D. Normandin, and W.K. Schiffer, Initial comparison of ntPET with microdialysis measurements of methamphetamine-induced dopamine release in rats: support for estimation of dopamine curves from PET data. Mol Imaging Biol, 2008. 10(2): p. 67-73. Voon, V., et al., Chronic dopaminergic stimulation in Parkinson's disease: from dyskinesias to impulse control disorders. Lancet Neurol, 2009. 8(12): p. 1140-9. Innis, R.B., et al., Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab, 2007. 27(9): p. 1533-9. Mintun, M.A., et al., A quantitative model for the in vivo assessment of drug binding sites with positron emission tomography. Ann Neurol, 1984. 15(3): p. 217-27. de la Fuente-Fernandez, R., et al., Biochemical variations in the synaptic level of dopamine precede motor fluctuations in Parkinson's disease: PET evidence of increased dopamine turnover. Ann Neurol, 2001. 49(3): p. 298-303. Morris, E.D. and K.K. Yoder, Positron emission tomography displacement sensitivity: predicting binding potential change for positron emission tomography tracers based on their kinetic characteristics. J Cereb Blood Flow Metab, 2007. 27(3): p. 606-17. Yoder, K.K., C. Wang, and E.D. Morris, Change in binding potential as a quantitative index of neurotransmitter release is highly sensitive to relative timing and kinetics of the tracer and the endogenous ligand. J Nucl Med, 2004. 45(5): p. 903-11. Normandin, M.D. and E.D. Morris, Estimating neurotransmitter kinetics with ntPET: a simulation study of temporal precision and effects of biased data. Neuroimage, 2008. 39(3): p. 1162-79. Constantinescu, C.C., C. Bouman, and E.D. Morris, Nonparametric extraction of transient changes in neurotransmitter concentration from dynamic PET data. IEEE Trans Med Imaging, 2007. 26(3): p. 359-73. Constantinescu, C.C., et al., Estimation from PET data of transient changes in dopamine concentration induced by alcohol: support for a non-parametric signal estimation method. Phys Med Biol, 2008. 53(5): p. 1353-67. Morris, E.D., et al., ntPET: a new application of PET imaging for characterizing the kinetics of endogenous neurotransmitter release. Mol Imaging, 2005. 4(4): p. 473-89. Evans, A.H., et al., Punding in Parkinson's disease: its relation to the dopamine dysregulation syndrome. Mov Disord, 2004. 19(4): p. 397-405. 3