Document
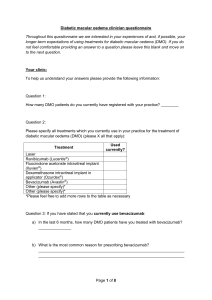
advertisement

DIABETIC MACULAR OEDEMA AND RELATED SIGHT LOSS AT FIRST SCREENING FOR EYE DISEASE The Wales Diabetic Retinopathy Screening Service (WDRSS) Darwin Minassian1, David Owens2, Angela Reidy1,3, Pritti Mehta4 Affiliations: 1 EpiVision , 2 Cardiff University, 3 London Metropolitan University, 4 UK Vision Strategy ABSTRACT Aims: To provide estimates for the prevalence of diabetic macular oedema (DMO) and the attributable sight loss in persons with diabetes attending a national Diabetic Retinopathy Screening Service, and the proportion that are potential candidates for referral to hospital for assessment and treatment. Methods: Analysis of data obtained on 27,178 diabetic persons at first presentation for screening at the Diabetic Retinopathy Screening Service for Wales (WDRSS), 2004-2005. Estimation of prevalence proportions, by age and gender. Results: DMO was present in one or both eyes of 7.05% of patients. The condition was unilateral in 4.72%, and bilateral in 2.33%. Clinically significant DMO with impaired vision attributable to DMO was present in 2.75% of patients, 0.11% being blind, and the remaining 2.64% having impaired visual acuity of <6/6 attributable to DMO. Conclusions: The estimates pertain to the prevailing mix of Type-I and Type-II diabetes in the population, and should be of interest as inputs for epidemiological and economic models for DMO. INTRODUCTION The initial call of WDRSS 2004/5 for formal screening was treated as a pilot survey of the prevalence of sight loss and of diabetic retinopathy in a diabetic population, and was prepared for reporting at the Liverpool, UK 17th – 18th November 2005 conference and also reported at the EASDEC 2006 conference. The rates for DMO quoted here are an expansion of the reporting on those analyses by Minassian and Reidy (EpiVision). The work was an aspect of the “Future Sight Loss UK” project commissioned by the RNIB / UK Vision Strategy in 2008. Age distribution Figure 1. Table 2 (a) & (b). Diabetic Retinopathy (DR) and Macular Oedema (DMO) coexistence in the same patient at first presentation for screening at the Diabetic Retinopathy Screening Service for Wales (2004-2005) 30% 25% a) in patients with DR &/or DMO in any eye. 20% Diabetic Retinopathy (any grade) 15% 10% DMO Absent DMO Present Totals DR Absent 0.00% 3.85% 3.85% DR Present 78.28% 17.88% 96.15% Totals 78.28% 21.72% 100.00% 5% METHODS 0% 12 – 19 Data were obtained on 27,178 individuals at first presentation for screening at the Diabetic Retinopathy Screening Service for Wales (WDRSS) (2004-2005). The source of recruitment was from a country-based register derived from General Practice registers of persons with diabetes. Grading of diabetic retinopathy was performed on digitalised fundus images, using the WDRSS scheme. Fundus photographs were assessed by a minimum of two trained graders and were quality controlled against the gold standard provided by the Clinical Director and a consulting ophthalmologist. Statistical methods included estimation of prevalence by age and gender. – 29 – 39 – 49 – 59 – 69 – 79 RESULTS 15.2) and 64 years respectively. About half (49%) of the patients were 65 or older (Figure1), and 56% were male. 90 + Table 1. Prevalence of Diabetic Macular Oedema & attributable sight loss in 27,000 persons at first presentation for screening at the Diabetic Retinopathy Screening Service for Wales (2004-2005). Ocular Morbidity Demographic Features of the Sample: The mean and median age were 62.6 years (sd – 89 % of All Diabetic Patients Diabetic Macular Oedema (DMO) in one or both eyes: Unilateral Bilateral 7.05 4.72 2.33 Clinically Significant DMO Causing Impaired Vision 1 Clinically Significant DMO Causing Blindness 2 2.64 0.11 b) in ALL patients with diabetes. Diabetic Retinopathy (any grade) DMO Absent DMO Present Totals DR Absent 67.52% 1.25% 68.77% DR Present 25.42% 5.81% 31.23% Totals 92.95% 7.05% 100.00% Type of Diabetes Treatment: Seventeen percent were on insulin treatment, 53% on OHA and the remaining 30% were managed on diet alone. Diabetic Macular Oedema (DMO) DMO was present in one or both eyes of 7.05% of patients. The condition was unilateral in 4.72%, and bilateral in 2.33% (Table-1). Clinically significant DMO with impaired vision attributable to DMO (best corrected visual acuity <6/6 in the worst affected eye) was present in 2.75% of patients. In 0.11% of diabetic patients the best-corrected visual acuity was ≤ 6/60 in both eyes, one or both being attributable to DMO. This may be considered as an estimate of candidates for referral to LVA services and for blindness or partial-sight registration. The remaining 2.64% of diabetic patients with impaired vision due to DMO but not blind may be considered as an estimate of the pool of potential candidates for referral to hospital services for assessment & treatment (Table-1). Among patients with diabetic retinopathy &/or DMO, about 18% had both conditions coexisting. In all patients with diabetes, this proportion was around 6% (Table-2) 1: Best corrected visual acuity <6/6 to >6/60 attributable to DMO, in one or both eyes of patient. 2: Best corrected visual acuity ≤ 6/60 in both eyes, one or both attributable to DMO. DISCUSSION The findings pertain to the mix of Type-I and Type-II diabetes prevailing in the population at the time. Our estimate of 2.64% of the ‘screened’ as potential candidates for referral to eye hospital for assessment & treatment, is in line with the reported proportion (2.11%) of the diabetic population (Type-II) having laser treatment for DMO during the first round of screening at Tayside, Scotland (Vallance et al, Diabetes Care 31:1126–1131, 2008). In our study, the analysis involved multi-way classification of individual eyes according to grades of retinopathy, DMO, and levels of visual impairment attributable to DMO. The focus, however, was on classification, counts and proportions of patients, as these estimates were considered to be more useful in construction of epidemiological and economic models for diabetic macular oedema.