Assessment of Mood and Adjustment Disorders in Individuals
With Visual Impairment
3
Watson
3
Kilpatrick
3
Yoon BS,
2
Wool
1
Williams
1
Alba
Daniel
BS, Ryan
BS, Grace
Laura
PsyD, Tracy
OD, and Felipe De
MD
1
2
3
Departments of Ophthalmology and Psychiatry , Loyola University Chicago Stritch School of Medicine , Maywood, IL 60153
Introduction and Purpose
Background Continued
Introduction
Low vision is defined by the WHO as a visual acuity worse than 20/60 in the
better eye [16]. Many diseases of the eye can cause a low vision state or
blindness. In the developed world, these largely include age-related macular
degeneration (AMD), diabetic retinopathy, and glaucoma. Glaucoma can often
be treated successfully with intraocular pressure lowering drops. AMD and
diabetic retinopathy, however, are chronic diseases with limited treatment
options resulting in most cases of low vision. The prevalence of AMD is 2.8% in
ages 40-59 and 13.4% in those 60 and above [10]. AMD is the cause of
blindness in 18% of blind individuals 65-75 and 30% of blind individuals above
75 making it the leading cause of blindness in the developed world [14]. The
prevalence of diabetic retinopathy is 28.5% with 4.4% of these being people
with vision threatening retinopathy [17]. This makes diabetic retinopathy the most
frequent cause of preventable blindness [12]. Studies have indicated that low
vision states are associated with increased rates of depression similar to and
even higher than other chronic diseases. A low vision state has been associated
with depression rates twice that of the community dwelling elderly [4,5,6,14].
Moreover, the associated depression may be a greater contributor to disability
than the patient's vision loss [4,6]. Complicating things more is the reciprocal
relationship between depression and disability: depression worsens disability
and disability worsens depression.
Study Design
Progression of AMD is followed with regular eye exams, optical coherence tomography
OCT, angiography, and fundus photography. Treatment includes an antioxidant vitamin
regimen with zinc and lutein, anti-VEGF injections (ranibizumab/ Lucentis® , bevacizumab/
Avastin®, and aflibercept/ Eylea®) as well as photodynamic therapy (PDT) with verteporfin
sensitization to eliminate weak blood vessels. The vitamin regimen has been shown to
help prevent the conversion of dry macular degeneration to wet macular degeneration [1,
8, 11]
Diabetic Retinopathy
Chronic hyperglycemia results in damage to microvascular pericytes causing increased
capillary permeability and weakness. Microaneurysms are the first sign of pathology.
Resulting ischemia causes neovascularization, edema and hemorrhage. Retinal
detachment can result secondary to edema or traction from vessel growth into the vitreous
body.
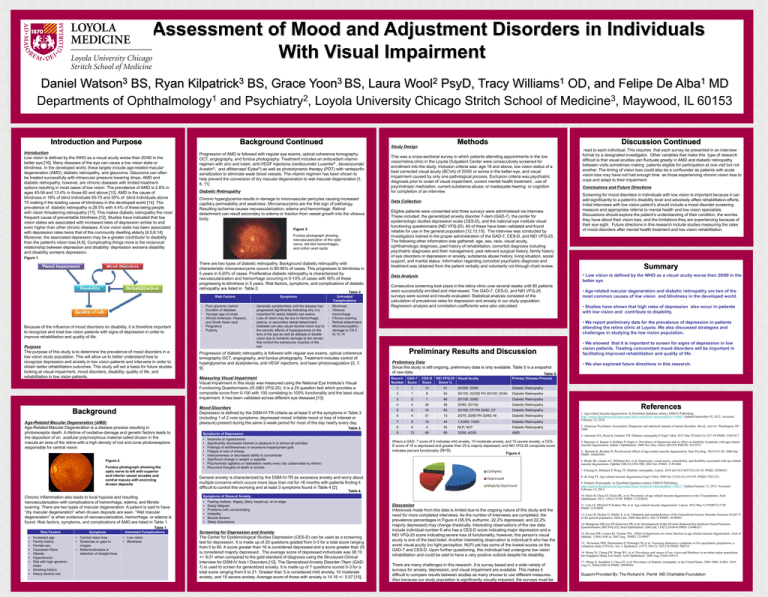
Figure 3.
Fundus photograph showing
neovascularization of the optic
nerve, dot-blot hemorrhages,
and cotton wool spots
Figure 1.
There are two types of diabetic retinopathy. Background diabetic retinopathy with
characteristic microaneurysms occurs in 80-95% of cases. This progresses to blindness in
5 years in 5-20% of cases. Proliferative diabetic retinopathy is characterized by
neovascularization and hemorrhage occurring in 5-10% of cases with 50% of these
progressing to blindness in 5 years. Risk factors, symptoms, and complications of diabetic
retinopathy are listed in Table 2.
Table 2.
Risk Factors
-
Because of the influence of mood disorders on disability, it is therefore important
to recognize and treat low vision patients with signs of depression in order to
improve rehabilitation and quality of life.
Purpose
The purpose of this study is to determine the prevalence of mood disorders in a
low vision study population. This will allow us to better understand how to
recognize depression and anxiety in low vision patients and intervene in order to
obtain better rehabilitation outcomes. This study will set a basis for future studies
looking at visual impairment, mood disorders, disability, quality of life, and
rehabilitation in low vision patients.
Background
Age-Related Macular Degeneration (AMD)
Age-Related Macular Degeneration is a disease process resulting in
photoreceptor death. A lifetime of oxidative damage and genetic factors leads to
the deposition of an acellular polymorphous material called drusen in the
macula an area of the retina with a high density of rod and cone photoreceptors
responsible for central vision.
Figure 2.
Fundus photograph showing the
optic nerve to left with superior
and inferior vessel arcades and
central macula with encircling
drusen deposits
Poor glycemic control
Duration of diabetes
Younger age of onset
African American, Hispanic,
and South Asian race
- Pregnancy
- Puberty
Symptoms
Untreated
Complications
- Generally symptomless until the disease has
progressed significantly indicating why it is
important for yearly diabetic eye exams
- Loss of vision may be due to hemorrhage,
edema, or secondary retinal detachment
- Diabetes can also cause blurred vision due to
the osmotic effects of hyperglycemia on the
lens of the eye as well as diplopia or double
vision due to ischemic damage to the nerves
that control the extraocular muscles of the
eye
- Blindness
- Vitreous
hemorrhage
- Fibrous scarring
- Retinal detachment
- Microneuropathic
damage to CN II,
III, IV, VI
Progression of diabetic retinopathy is followed with regular eye exams, optical coherence
tomography OCT, angiography, and fundus photography. Treatment includes control of
hyperglycemia and dyslipidemia, anti-VEGF injections, and laser photocoagulation [3, 7,
9].
Measuring Visual Impairment
Visual impairment in this study was measured using the National Eye Institute’s Visual
Functioning Questionnaire–25 (NEI VFQ-25). It is a 25 question test which provides a
composite score from 0-100 with 100 correlating to 100% functionality and the least visual
impairment. It has been validated across different eye diseases [13].
Mood Disorders
Depression is defined by the DSM-IV-TR criteria as at least 5 of the symptoms in Table 3
(including 1 of 2 core symptoms: depressed mood/ irritable mood or loss of interest or
pleasure) present during the same 2-week period for most of the day nearly every day.
Table 3.
Symptoms of Depression
•
•
•
•
•
•
•
•
Methods
Insomnia or hypersomnia
Significantly decreased interest or pleasure in in almost all activities
Feelings of worthlessness or excessive inappropriate guilt
Fatigue or loss of energy
Indecisiveness or decreased ability to concentrate
Significant change in weight or appetite
Psychomotor agitation or retardation nearly every day (observable by others)
Recurrent thoughts of death or suicide
Discussion Continued
This was a cross-sectional survey in which patients attending appointments in the low
vision/retina clinic in the Loyola Outpatient Center were consecutively screened for
enrollment into the study. Inclusion criteria was: age 18 and above, low vision status of a
best corrected visual acuity (BCVA) of 20/60 or worse in the better eye, and visual
impairment caused by only one pathological process. Exclusion criteria was psychiatric
diagnosis prior to onset of visual impairment, current mental health treatment , use of
psychotropic medication, current substance abuse; or inadequate hearing or cognition
for completion of an interview.
Data Collection
Eligible patients were consented and three surveys were administered via interview.
These included: the generalized anxiety disorder 7-item (GAD-7), the center for
epidemiologic studies depression scale (CES-D), and the national eye institute visual
functioning questionnaire (NEI VFQ-25). All of these have been validated and found
reliable for use in the general population [12,13,15]. The interview was conducted by
investigators trained in the proper administration of the GAD-7, CES-D, and NEI VFQ-25.
The following other information was gathered: age, sex, race, visual acuity,
ophthalmologic diagnosis, past history of rehabilitation, comorbid diagnosis including
psychiatric diagnoses and their management, past relevant surgical history, family history
of eye disorders or depression or anxiety, substance abuse history, living situation, social
support, and marital status. Information regarding comorbid psychiatric diagnosis and
treatment was obtained from the patient verbally and voluntarily not through chart review.
Consecutive screening took place in the retina clinic over several weeks until 80 patients
were successfully enrolled and interviewed. The GAD-7, CES-D, and NEI VFQ-25
surveys were scored and results evaluated. Statistical analysis consisted of the
calculation of prevalence rates for depression and anxiety in our study population.
Regression analysis and correlation coefficients were also calculated.
•
•
•
•
•
•
•
Increased age
Family history
Female sex
Caucasian Race
Obesity
Hypertension
Diet with high glycemic
index
• Smoking history
• Heavy alcohol use
Symptoms
• Central vision loss
• Scotomas or gaps in
images
• Metamorphopsia or
distortion of straight lines
Untreated Complications
• Low vision
• Blindness
Summary
• Age-related macular degeneration and diabetic retinopathy are two of the
most common causes of low vision and blindness in the developed world.
• Studies have shown that high rates of depression also occur in patients
with low vision and contribute to disability.
• We report preliminary data for the prevalence of depression in patients
attending the retina clinic at Loyola. We also discussed strategies and
challenges in studying the low vision population.
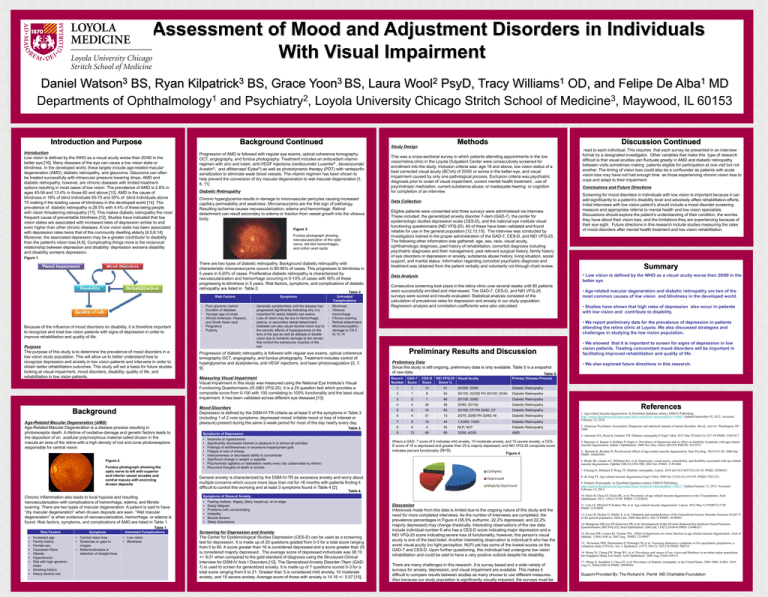
Preliminary Results and Discussion
Preliminary Data
Since this study is still ongoing, preliminary data is only available. Table 5 is a snapshot
of raw data.
Table 5.
Record GAD-7
Number Score
CES-D
Score
NEI VFQ-25 Visual Acuity
Score %
• We showed that it is important to screen for signs of depression in low
vision patients. Treating concomitant mood disorders will be important in
facilitating improved rehabilitation and quality of life.
• We also explored future directions in this research.
Primary Disease Process
1
1
13
51
20/200; 20/60
Diabetic Retinopathy
2
1
8
54
20/100; 20/200 PH 20/100; 20/40
Diabetic Retinopathy
3
0
1
66
20/100; 20/60
Diabetic Retinopathy
4
4
28
48
20/80; 20/100
Diabetic Retinopathy
5
0
10
65
20/100; CF PH 20/80, CF
Diabetic Retinopathy
6
4
31
13
20/70; 20/60 PH 20/60; NI
Diabetic Retinopathy
7
9
19
44
1.5/200; 1/200
Diabetic Retinopathy
8
0
4
54
NLP; NLP
Diabetic Retinopathy
9
12
49
68
3/200; 4/200
AMD
Where a GAD- 7 score of 5 indicates mild anxiety, 10 moderate anxiety, and 15 severe anxiety; a CESD score of 16 is depressed and greater than 25 is majorly depressed; and NEI VFQ-25 composite score
indicates percent functionality (N=9).
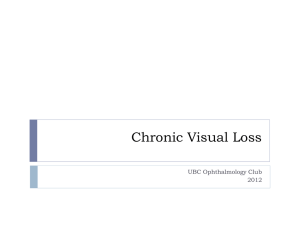
Figure 4.
References
1. Age-related macular degeneration. In DynaMed [database online]. EBSCO Publishing.
http://search.ebscohost.com/login.aspx?direct=true&site=dynamed&id=114486. Updated September 05, 2012. Accessed
February 12, 2010.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC:
2000.
3. Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy.N Engl J Med. 2012 Mar 29;366(13):1227-39 PMID: 22455417
4. Banerjee A, Kumar S, Kulhara P, Gupta A. Prevalence of depression and its effect on disability in patients with age-related
macular degeneration. Indian J Ophthalmol. 2008 Nov-Dec; 46(6): 469-474 PMCID: 2612975
5. Berman K, Brodaty H. Psychosocial effects of age-related macular degeneration. Inter Psychog. 18(3):415-28, 2006 Sep.
PMID. 164665924
6. Brody BL, Gamst AC, Williams RA, et al. Depression, visual acuity, comorbidity, and disability associated with age related
macular degeneration. Ophthal 108(10):1893-900, 2001 Oct. PMID: 11581068
7. Cheung N, Mitcheel P, Wong TY. Diabetic retinopathy. Lancet. 2010 Jul 10;376(9735):124-36. PMID: 20580421
8. de Jong PT. Age-related macular degeneration Engl J Med. 2006 Oct 5;355(14):1474-85. PMID:17021323
9. Diabetic Retinopathy. In DynaMed [database online]. EBSCO Publishing.
http://search.ebscohost.com/login.aspx?direct=true&site=dynamed&id=116611. Updated January 12, 2013. Accessed
February 12, 2013.
10. Klein R, Chou CF, Klein BE, et al. Prevalence of age-related macular degeneration in the US population. Arch
Ophthalmol. 2011; 129(1):75-80 PMID: 212230632
Symptoms of General Anxiety
Feeling restless, fidgety, jittery, keyed-up, or on edge
Easily fatigued
Problems with concentrating
Irritability
Muscle tension
Sleep disturbance
Table 1.
Risk Factors
Screening for mood disorders in individuals with low vision is important because it can
add significantly to a patient’s disability level and adversely affect rehabilitation efforts.
Initial interviews with low vision patient’s should include a mood disorder screening
measure and appropriate referral to mental health and low vision specialists.
Discussions should explore the patient’s understanding of their condition, the worries
they have about their vision loss, and the limitations they are experiencing because of
their eye sight. Future directions in this research include studies measuring the rates
of mood disorders after mental health treatment and low vision rehabilitation.
better eye.
General anxiety is characterized by the DSM-IV-TR as excessive anxiety and worry about
multiple concerns which occurs more days than not for >6 months with patients finding it
difficult to control this worrying and at least 3 symptoms found in Table 4 [2].
•
•
•
•
•
•
Conclusions and Future Directions
• Low vision is defined by the WHO as a visual acuity worse than 20/60 in the
Data Analysis
Table 4.
Chronic inflammation also leads to local hypoxia and resulting
neovascularization with complications of hemorrhage, edema, and fibrotic
scarring. There are two types of macular degeneration: A patient is said to have
“dry macular degeneration” when drusen deposits are seen. “Wet macular
degeneration” is when evidence of neovascularization, hemorrhage, or edema is
found. Risk factors, symptoms, and complications of AMD are listed in Table 1.
read to each individual. This requires that each survey be presented in an interview
format by a designated investigator. Other variables that make this type of research
difficult is that visual acuities can fluctuate greatly in AMD and diabetic retinopathy
between visits sometimes making patients eligible for participation at one visit but not
another. The timing of vision loss could also be a confounder as patients with acute
vision loss may have not had enough time as those experiencing chronic vision loss to
cope and adapt to their impairment.
Screening for Depression and Anxiety
The Center for Epidemiological Studies Depression (CES-D) can be used as a screening
test for depression. It is made up of 20 questions graded from 0-3 for a total score ranging
from 0 to 60. A score greater than 16 is considered depressed and a score greater than 25
is considered majorly depressed . The average score of depressed individuals was 38.10
+/- 9.01 when compared to the gold standard of diagnosis using the Structured Clinical
Interview for DSM-IV Axis I Disorders [12]. The Generalized Anxiety Disorder-7item (GAD7) is used to screen for generalized anxiety. It is made up of 7 questions scored 0-3 for a
total score ranging from 0 to 21. Greater than 5 is considered mild anxiety, 10 moderate
anxiety, and 15 severe anxiety. Average score of those with anxiety is 14.18 +/- 5.57 [15].
Discussion
Inferences made from this data is limited due to the ongoing nature of this study and the
need for more completed interviews. As the number of interviews are completed, the
prevalence percentages in Figure 4 (55.5% euthymic, 22.2% depressed, and 22.2%
majorly depressed) may change drastically. Interesting observations of the raw data
include individual number 6 who has a CES-D score indicating major depression and a
NEI VFQ-25 score indicating severe loss of functionality; however, this person’s visual
acuity is one of the best listed. Another interesting observation is individual 8 who has the
worst visual acuity (no light perception, NLP) yet has some of the lowest scores on the
GAD-7 and CES-D. Upon further questioning, this individual had undergone low vision
rehabilitation and could be said to have a very positive outlook despite his disability.
There are many challenges in this research. It is survey based and a wide variety of
surveys for anxiety, depression, and visual impairment are available. This makes it
difficult to compare results between studies as many choose to use different measures.
Also because our study population is significantly visually impaired, the surveys must be
11. Lim LS, Mitchell P, Seddon JM, et al. Age-related macular degeneration. Lancet. 2012 May 5;379(9827):1728
PMID: 22559899
12. Lowe B, Decker O, Muller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7)
in the general population. Med Care. 2008 Mar;46(3): 266-74 PMID: 18388841
13. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute Visual Function
Questionnaire (NEI VFQ-25). Arch Ophthalmol. 2001 Jul; 119(7):1050-8 PMID: 11448327
14. Rovner BW. Casten RJ. Tasman WS. Effect of depression on vision function in age-related macular degeneration. Arch of
Ophthal. 120(8):1041-4, 2002 Aug. PMID: 12149057
15. Weissman MM, Sholomskas D, Pottenger M, et al. Assessing depressive symptoms in five psychiatric populations: a
validation study (CES-D). Am. J. Epidemiol. (1977) 106 (3): 203-214 PMID: 900119
16. Wong Ty, Chong EW, Wong WL, et al. Prevalence and causes of low vision and blindness in an urban malay population:
the Singapore Malay Eye Study. Arch Ophthalmol. 2008 Aug;126(8):1091-9
17. Zhang X, Saaddine J, Chou CF, et al. Prevelance of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010
Aug 11; 304(6):649-56 PMID: 20699456
Support Provided By: The Richard A. Perritt MD Charitable Foundation