Quantitative methods - University of Otago
advertisement

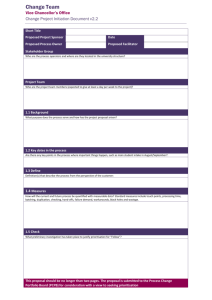
Healthcare Resource Allocation David Hadorn, MD, Ph.D University of Otago Wellington School of Medicine 27 September 2010 Healthcare Resource Allocation • Definitions • Oregon as case study • NZ experience and current activity Definitions • Resource Allocation – implies differential value to be maximised • Rationing – implies fairness, restricted portions, limitations on services • Prioritisation – implies ordering effect with some services falling below threshold Oregon • Legislation passed in 1989 • Designed to set priorities amongst all health services for use in Medicaid • Philosophy was (and remains) to drop services, not people, when funding gets tight • Still going strong today, with waiting list Oregon, cont. • Health Services Commission develops prioritised list • Several hundred ‘line-items’ (condition-treatment pairs) • Legislature sets funding level • Actuaries translate this into a funding threshold on the prioritised list • Service threshold is specified (currently 503 / 680) • Services below funding threshold (nominally) not covered In more detail… Oregon • First list developed 1990 using classical CUA ($ / QALY) • Priority order seemed obviously wrong Result of First CUA History of Prioritisation in NZ • Core Services Committee 1992 • Gave up task of defining ‘the core’ in 1996 (too hard, too controversial, Oregon) • HFA took over prioritisation efforts 19972000 • Since then, little progress on national systematic prioritisation – some DHB work • PHARMAC has kept going strong Current HVDHB Scoring Components Score Maori Health Criteria 1 No targeting for Maori, mainstream service 2 Little targeting to Maori (e.g. targeted to low income), mainstream service Score Effectiveness Criteria 1 No expert evidence 2 Conflicting evidence but recommended by Service Planning Groups Some evidence or expert consensus 3 Mainstream service targeted to Maori 3 4 Maori service 4 5 Fully by Maori for Maori service 15% Weighting Good international evidence or well designed controlled trials 5 Good New Zealand evidence or randomised control trials 25% Weighting Score Equity Criteria 1 Untargeted service Untargeted service but with relatively high proportions of those with the poorest health and highest need 3 Some targeting to those with the poorest health and highest need 4 Generally targeted to those with the poorest health and highest need 5 Targeted specifically to those with the poorest health and highest need 25% Weighting Score Value-for-Money Criteria 2 Scored on 4 separate dimensions below 35% Weighting Value-for-Money dimensions Score Cost per Person Criteria Score Cost Savings Criteria 1 2 >$10,000 per person $1,000-$10,000 per person 1 2 Little or no cost offsets Small cost offsets 3 $100-$999 per person 3 Medium cost offsets 4 $10-$99 per person 4 Large offsets 5 $0-$9 per person 5 Very Large cost offsets 15% Weighting 5% Weighting Score Effectiveness per Person Criteria 1 Little, if any, direct gain 2 Some benefits, small reduction in disability or small increase increase in quality of life 3 Medium benefits, moderate reduction in disability and/or some increase in quality of life or life expectancy 4 Large benefits, good reduction in disability and/or increase in quality of life or life expectancy 5 Huge benefits, adding many years of quality life 10% Weighting Score Timing of Benefits Criteria 1 2 10+ years 6-9 Years 3 3-5 years 4 2 years 5 Within 1 year 5% Weighting Ranked Table of Initiatives Prioritisation Scoring Table - With Weightings Plan Diab/Card Primary Card Child Youth Cancer Chronic Dis Child Health Comm Health Comm Primary Youth Child Health Comm Oral Primary Youth All All Diab Disability Maternity Resp Surgery Youth All Health Comm Child Oral Maternity Youth Child Surgery Health Comm Proposal/Initiative Diabetes Pilot prevention PHO JV Card rehab Prog Kidznet Youth School Health Clinics - targeted Cancer mole removal subsidy Chronic Dis Clinical Pathways in Primary care Immunisation assertive outreach Lifestyle - CHW via targetted PHO Smoking Cessation Primary care teams - Additional Nurses YHS to older youth Ear Caravan Physical Activity - Market Green Scripts Pilot Basic dental service Primary care reduce copayments -Targeted Youth School Health Clinics Service Directory Audits - additional Increase Podiatry Service Disability Advisor Additional post natal support -special needs Flu Vac assert recall Increase Nurse clinics Card & ED Peer support /educators Workforce development fund Ethnicity Collection Workforce development - well child Oral Health enrol adolescents w default prov Maternity coordination mechanism Youth Health Coordinator Mental Health Moderate needs pilot Surgery Diagnostics - Radiology Workforce Study 15% 25% 25% Score 78 68 68 64 65 74 65 72 66 69 62 61 68 62 69 66 53 46 67 66 52 63 65 53 50 62 68 47 60 55 37 44 41 37 Maori 9 9 9 9 6 3 9 9 9 6 6 9 9 3 9 12 6 6 9 9 3 6 3 3 6 9 12 6 9 6 3 6 3 6 Effective ness 20 15 20 10 15 25 15 15 10 20 15 15 15 20 10 10 15 5 20 20 10 15 20 15 10 15 15 10 10 15 5 10 10 5 Equity 25 15 15 20 20 20 20 20 25 20 15 15 20 10 25 20 10 10 15 15 15 20 15 10 10 15 20 10 20 10 5 10 5 5 63 64 45 50 55 41 36 6 6 6 3 9 6 3 20 20 10 15 10 10 5 15 15 10 15 15 10 5 0% 0% 15% Consist w Acceptabi Cost per NZHS lity person 0 0 9 0 0 15 0 0 9 0 0 15 0 0 12 0 0 9 0 0 9 0 0 12 0 0 9 0 0 6 0 0 15 0 0 12 0 0 12 0 0 15 0 0 12 0 0 12 0 0 12 0 0 15 0 0 15 0 0 9 0 0 15 0 0 9 0 0 12 0 0 12 0 0 12 0 0 15 0 0 15 0 0 15 0 0 12 0 0 15 0 0 15 0 0 9 0 0 12 0 0 15 5% Cost offsets 4 3 4 3 2 4 3 4 3 5 2 2 3 3 2 2 2 1 1 3 1 2 4 3 2 1 1 1 1 1 1 1 2 1 10% 5% Time to effectiven Outcomes ess 8 3 6 5 6 5 4 3 6 4 8 5 6 3 8 4 8 2 10 2 6 3 4 4 6 3 8 3 6 5 6 4 4 4 4 5 4 3 6 4 4 4 6 5 6 5 6 4 6 4 4 3 2 3 2 3 4 4 4 4 4 4 4 4 4 5 2 3 Mental Health Mental Health Mental Health Mental Health Mental Health Mental Health Mental Health Mental Health Psychological therapies MH Quality & Outcomes program devel Youth crisis respite services MH Aged Care Workforce development - MH Scholarships Primary Mental Health long term stable Outsource MH link Newsletter 0 0 0 0 0 0 0 0 0 0 0 0 0 0 9 15 6 6 15 6 15 3 1 2 1 1 1 1 6 4 6 6 2 4 2 4 3 5 4 3 4 5 National Prioritisation Back on Agenda Renewed government interest in prioritisation signaled through series of Wellington Health Economist Group seminars: Gerald Minnee, Ruth Isaac, NZ Treasury. Health system sustainability in the long term: Why we need to act today. 22 May 2008 Judy Kavanaugh, MOH. Prioritisation: why is it so hard? 21 August 2008 Janet McDonald. Prioritisation: Change and Adaptation in Families with Young Carers. 11 September 2008 David Hadorn and Martin Hefford. Saying ‘no’ in three countries: alternative methods of healthcare prioritisation. 16 October 2008 (repeated at VUW and Treasury) Creation of Centre for Assessment and Prioritisation July 2009 “Meeting the Challenge” • Ministerial Review Group (MRG) – Horn Report • Released 16 August 2009 • Changed dynamic for health reform • Several recommendations support CAP’s mission MRG on prioritisation From MRG report: [We recommend] revamping and strengthening the National Health Committee, so that it is better able to perform its original role of assessing the appropriateness and cost-effectiveness of new services, and progressively reassessing existing services. p 5 [A] single national agency removed from both DHBs and the Ministry [is needed]. The best approach would be to strengthen the NHC. p29 sec72 Cabinet Paper • “[MRG] identified improved prioritisation as way to manage costs and improve safety and effectiveness of health services, as has been achieved by PHARMAC with respect to community pharmaceuticals. This requires smarter control of the introduction of new technology and interventions . . . while decreasing the utilisation of less effective and outdated services.” Cabinet Social Policy Committee, Improving the Health System: Further Elements: Paper One: Prioritisation of New Technologies and Interventions, 19 March 2010 Decisions Yet To Be Taken • Cabinet has embraced MRG’s main recommendation but still has to decide • (1) how NHC should select and assess interventions • (2) whether and how NHC decisions should affect or constrain District Health Boards’ funding decisions, and • (3) whether and how groups of similar products and services (e.g., new technologies, devices, diagnostics) might be ring-fenced and subjected to a fixed budget, PHARMAC-style. Minister at Arms’ Length from Process • “risk” of becoming “directly [involved] in detailed and potentially sensitive decisions . . . [including] establishing the work programme, which may also be contentious.” • “can create PHARMAC-like budget arrangements to place Minister at arms length from the decisions” • OTOH Minister must retain ability to veto output in capacity as elected representative • But make it difficult to veto, like PHARMAC Treasury is Cautious • Treasury cited these issues as reasons to ‘defer’ development of a prioritisation infrastructure (despite Minister’s expressed wish to begin “as soon as possible” with consultation to run alongside): “Deferral would enable the decisions to be taken further in terms of how prioritisation will in fact work and how any prioritisation recommendations will be implemented (crucially, how it will or will not constrain DHBs). These design details matter, as there is a risk of fuelling, rather than dampening, health cost pressures if the model is wrong.” How Should NHC Advice Bind DHBs? • Don’t want to force DHBs to purchase services deemed high priority (like NICE in UK) or to invest or disinvest in same services (accept some disparities as price for local control) • Give DHBs options for new investments and disinvestments – balance costs Proposed Prioritisation Method: • National Health Committee would use “Traffic Light” approach • Combines central assessment and prioritisation with local choice • Using Cabinet-approved methods, including consultation, National Health Committee would develop three lists: green, orange, red • Green = good new investments (new technology or expand existing) • Orange = good candidates for disinvestment, i.e., marginal value for money • Red = indications for which services should not be performed or funded (zero or negative net benefit) Proposed method, continued • Cost of green list = cost of orange + red lists – compatible with fixed budget • DHBs permitted to choose amongst designated services based on local considerations • Could go ‘off list’ but would be asked to explain why to Minister