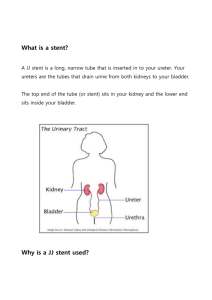
Procedure
advertisement

Colonic stenting: Single institution experience from a UK district general hospital Background • 8-29 % of patients with colon cancer present with partial or total obstruction (1) • Emergency surgery is associated with up to 25% mortality (2) • Self expandable metal stent (SEMS) provides a low-risk and successful option. 1. Fregonese et al, GASTROINTESTINAL ENDOSCOPY Volume 67, No. 1 : 2008 2. Small et al, GASTROINTESTINAL ENDOSCOPY Volume 71, No. 3 : 2010 Colon Cancer Palliation Malignant Colonic Obstruction “Bridge to Surgery” For patients that are nonsurgical candidates with metastatic disease or comorbid illness For decompression of the colon prior to surgery Alternatives Metal Stent Two Stage Surgery (Temporary Colostomy) Table Lavage Surgery Metal Stent Procedure Catheter and contrast injected carefully proximal to lesion. Guidewire is advanced across the lesion The stent delivery system is positioned across the lesion The stent is deployed Stent placement is confirmed via fluoroscopic and endoscopic images Aim •We set out to evaluate the outcome of the use of SEMS in malignant colonic obstruction (MCO) in a district general hospital (DGH) Method •Retrospective study between 1st Jan 2007 to 28th Feb 2014 •Patients identified from prospectively maintained endoscopy and stent database •The endoscopy reporting software (Unisoft), stent logbook, patient document portal, and patient administration system (Sunquest) were reviewed for data collection. •Information regarding indication and treatment intent, site of the lesion, stent type, procedure outcome, adverse events, and patient demographics were reviewed. 9. Calvert et al, Gastroenterology 2004 Results • 75 patients underwent 78 SEMS insertion • Majority were males (n=50, 66.7%) • Median age was 77 years (47-96 yrs) • Technical success 98.7% (n=77) • Clinical success 89.6% (n=69) Results •Majority (91%) of the SEMS were inserted in the left colon - sigmoid colon 40 (51.3%) descending colon 15 (19.2%), rectum 14 (17.9%), transverse colon 7 (9.0%) and anastomotic recurrence post left hemicolectomy in 2 (2.6%) • 53 (67.9%) underwent semi-elective colonic SEMS insertion and 25 (32.1%) had emergency stent inserted •10 (12.8 %) SEMS were inserted as a bridge to surgery while 68 (87.2%) were inserted for palliation. Complications • 1 perforation (1.3%) - Hartmann`s procedure • Wire guided extravasation of contrast (managed conservatively after stent insertion) in 1 (1.3%) –no harm to patient • Migration in 3 (3.8%) resulting in stent removal[1 self extrusion of rectal stent] • Stent blockage in 3 (3.8%) [1unblocked with enema, 2 tumour ingrowth] • Stent non-function in 2 (2.6%) [failed expansion secondary to very tight ca] • 30 day mortality 10.3% (n=8) - none procedure related Conclusion • High quality colonic stent service with high technical and clinical success rate can be delivered in a DGH • Experienced operators has ensured low complication rate • Low 30 day mortality (10.3%) - none procedure related • The service has responded to the presentation of the acutely obstructed patients • All acute surgical units should have access to an colonic stenting service 13 Tips • Work as a team with surgeons – joint decision making through MDT • Procedure to be carried out by experienced therapeutic endoscopist • Be confident in the use of fluoroscopy, twin channel therapeutic gastroscope, colonic irrigator, swing tip catheter and wires • Be able to do urgently – within hours of admission • Allow yourself plenty of time for the procedure – 60 min • Prescribe laxatives post stenting