Methodology
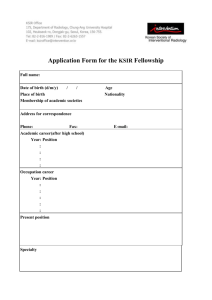
advertisement

Protocol 868 Cordis ARTS Deliverability Research Study: Formative User Preference Study Date: August 26, 2010 Originator: Sean Hägen Overview The following study protocol dictates the process in which BlackHägen Design (BH) will identify, document, and analyze (benchmark) User Preference input for a double-blind, qualitative design research study to understand physicians’ current and ideal definition of stent “deliverability” and it’s associated system solution attributes for percutaneous coronary intervention (PCI) stent delivery systems. This study is intended to benchmark user requirements to support the Cordis Arterial Revascularization Therapies Study (ARTS) from the perspective of the physician in PCI treatment markets – specifically the drug eluting stent (DES) delivery portion. The study methodology will include ethnography (contextual observation) of PCI procedures and brief face-to-face interviews. A comprehensive understanding of the environment, communication between clinicians, procedure protocol, hand biomechanics and user tendencies when delivering DES will be documented in the subsequent Benchmark Report. Objectives ► Map the PCI Usage Characteristics during the DES Delivery Steps Characterize and codify the optimal stent delivery experience from the user’s perspective, key current facilitators and barriers, and identify target design criteria for successful delivery system development from device removal from package to device disposal. Note: emphasis will be placed on actual stent delivery in context. While other aspects of the procedure will be noted e.g. introduction sheath insertion, etc. this will not be described with extensive fidelity ► Characterize User Sample Identify and rank User Personas in order to augment the User Preference Inputs. ► Document User Preference Rationale Capture how physicians define deliverability, what procedural factors influence it, how it is measured, and ultimately, what are the attributes of a PCI-system that enables optimal deliverability (deliver significant design input rationalization for future development of ARTS Device Requirements by Cordis). 533561349.doc 1 Recruitment Criteria The user (Respondent) qualification criteria and recruitments are based on an interventional cardiologist (physician) practicing in two domestic regions (East and West coast), the lead physician’s experience level performing arterial revascularization procedures, the respondent’s volume of cases per year and the diversity of device brands utilized annually. Sample size is also influenced by the project schedule, budget (honoraria) and available access to participating institutions. Respondents: N = 15-20 Inclusive Screening Criteria: Performs at least 120 PCI procedures per year (on average) The sample population should breakdown as follows: Expert (Podium Speaker) 10% Veteran (<155 PCI/yr or 5 yrs tenure) 30% Educator 30% Common Interventionalist (less experienced) 30% Device Usage proportions (objectives) o Uses Cordis Device 30% o Uses Boston Science Devices 30% o Uses Abbott Devices or other 30% 2-4 Transradial approaches Exclusive Screening Criteria: No more than 2 respondents that primarily uses Cordis devices only Methodology The number of attending BH observers will be no more than two (2) in order to minimize intrusion bias and maintain a relaxed, uninhibited environment for the respondents. In order to facilitate minimally invasive contextual observation, the researchers will set-up the video equipment during lab instrument set-up (prior to the patient and primary physician entering the lab). One observer will be in the lab operating the camera equipment the second observer will remain in the control room capturing time metrics. During each site visit, BH will employ a multi-channel video approach which simultaneously captures activity at both the proximal and distal ends of the devices in use. The videos will be synchronized post production. Observations of the user’s focus of attention will also be noted and captured with still images. The site visit will be concluded by interviewing research participants. Interviews will be digitally recorded and the data documented (transcribed) for analysis and archiving. Permission will be obtained ahead of time from the lab manager for filming/photography. Participating physicians/lab managers will be responsible for obtaining patient consent. All data (video, still photography, audio, etc.) will exclude any patient specific (identity) data in order to conform to HIPAA compliance requirements. 533561349.doc 2 Methodology continued… A Discussion Guide and the supporting Datasheet are intended to provide the BH researcher with guidelines and a checklist of metrics to capture, measure and characterize during site visits. The following is an example of an introductory discussion with a Respondent. It should not be read verbatim, rather as a reference if Respondents want more information on why or how we are conducting the study: We are a design consultant for a medical manufacturer that is developing a PCI stent delivery system that optimizes usability. Our client must remain undisclosed in order to maintain a double-blind study requirement. We are here today to observe you, specifically the usability aspects of delivering a stent. Your experience and opinions will help us learn what criteria can insure future devices are meeting you needs, so it is very important that you give us your honest opinions— good or bad. In general, we are interested in: Any particular challenges, bottle-necks you experience during the procedure. If the performance of any device involved is less than optimal, and why? Your ideas for improving the experience for yourself, your team, and the patient. After the completion of the procedure, we’d like to spend no more than 15 minutes with you to clarify some of our observations and also take you through an exercise where you will have the opportunity to share some of your experiences with us in more detail. This is certainly not a test of your abilities! We are interested in knowing how and why you personally do things a certain way. At this time, we’d like to know if it is ok for us to ask you questions during the procedure. If there are any specific parts of the procedure that you feel are difficult to understand, from our point of view, feel free to describe what you are doing. If at any time you need us to leave the room, we are prepared to shut-down the cameras and leave the room immediately. Thank you for the opportunity to learn from you and your team! 533561349.doc 3 Methodology continued… At the convenience of the cardiologist, BH will conduct a brief interview. A methodology for obtaining the step by step breakdown of the procedure and the associated emotive connections used is called projective mapping. The projective mapping exercise utilizes metaphoric images to enable the respondent to better articulate their experiences and aspirations through storytelling and projective association. The researcher will ask the respondent to describe his or her experience during the procedure. Using this type of exercise, it will become apparent the number of steps and emotions involved for each task. Once collected a procedure map will be created using the steps and emotional metrics shown with this exercise, time metrics and devices used, and data collected through video. Interview Guide 1. Please describe the steps in delivering stent. Probe for: a. Major milestones within the procedure b. Specific techniques to advance (stent) catheter over guide wire, around tortuous anatomy c. Key feedback throughout the procedure, what lubricity is appropriate? (this may need physical aids to really dive into e.g. set of tubes with predetermined friction for comparison) d. What attributes are associated with pulling the stent back into guidecath, balloon inflation/over-inflation, stent deployment e. As the stent opens (is deployed) what feedback is most important? f. What do they use a reference guide to confirm that delivery is on target? 2. What are the most difficult challenges regarding the delivering a stent? Why? 3. Can you define any “rules of usage” or tips that you usually give to novice users? 4. What constitutes easier stent delivery? 5. How do you define tracking? How important is tracking? 6. How do you define pushability? 7. How important is pushability? 8. Why do you choose to use one stent brand over another? 9. Do they choose to use a different stent for radial access vs. femoral access? Why? 10. Which stent has the best deliverability? Why? 11. What might improve deliverability? 533561349.doc 4 Observation Guide Overall room layout Personnel identification and work flow path Set-up of instrumentation: where possible provide a list of all catheters used, including brand names Observed procedure steps including challenges and mitigations o Challenges to be defined as any portion of the procedure which takes excessive amounts of time, obvious mood changing events, trials/re-trials on device performance, and any device interchanges e.g. disposal of one catheter for another Metric Objectives of Study 1. Establish User Requirements for preparation of Stent Delivery Systems (opening package and prepare additional equipment, i.e. syringes/stopcock, flush etc.) 2. Determine the unique behavior steps (technique) during delivery 3. Correlate device characteristics with behavior modalities (user inputs to device outputs) a. Describe opinions, thoughts, and perceptions regarding actions e.g. what works, what doesn’t and why. 4. Characterize device response from navigation, lesion access to deployment a. Describe challenge and ease of use areas b. Describe stent visibility issues 5. Capture relative perception/emotion/opinion that correlate with use characteristics during delivery scenarios. 6. Evaluate current device deliverability through distal and tortuous vessels 7. Specific product interaction attributes to be assessed include the following: a. Lubricity of the outer body b. Perception of system behavior with regards to feedback and response e.g. tracking and pushability c. Attributes of use interaction at critical points in the procedure including reaching lesion site, deployment and device removal. d. Stent visibility e. The usefulness of catheter marker bands (indicating location/spacing of stent on balloon), understand the design constraints around marker placement and the appropriate degree of radiopacity 533561349.doc 5 Equipment The following equipment will be utilized for this study: 1. Digital Still Camera 2. Digital Video Camera (2) 3. Audio Recorder 4. Tripod (2) 5. Protocol 6. Data Collection Sheets 7. Projective Mapping exercise 8. Discussion Guide 9. Note pad 533561349.doc 6