Nervous System Part 5
advertisement

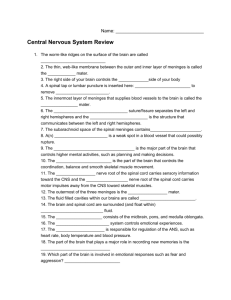
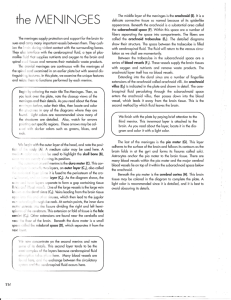
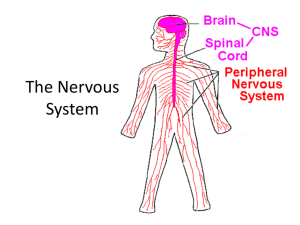
Chapter 7 – Part 5 The Nervous System Protection of the Central Nervous System 1. 2. 3. 4. Scalp and skin Skull and vertebral column Meninges Cerebrospinal fluid 5. Blood brain barrier Meninges The three connective tissue membranes covering and protecting the CNS structures are meninges. Three Layers: 1. Dura Mater 2. Arachnoid Mater 3. Pia Mater Meninges 1. Dura Mater – Outer most layer Feels tough & leathery Folds inward in several areas Double-layered external covering 1. Periosteum – Attached to the inner surface of the skull 2. Meningeal Layer – Outer covering of the brain Meninges 2. Arachnoid Layer – Middle meningeal layer Web-like 3. Pia Mater – Innermost membrane of the meninges Clings tightly to the surface of the brain and spinal cord, following every fold Delicate layer Cerebrospinal Fluid Similar to blood plasma composition Formed by the choroid plexus Forms a watery cushion to protect the brain Continually circulated in arachnoid space, ventricles, and central canal of the spinal cord Ventricles and Location of the Cerebrospinal Fluid Meningitis Meningitis - Inflammation of the meninges Serious threat to the brain because bacterial or viral meningitis may spread into the nervous system of the CNS. Usually diagnosed by taking a sample of cerebrospinal fluid Procedure is called a lumbar (spinal) tap Blood Brain Barrier No other body organ is so absolutely dependent on a constant internal environment as is the brain. Other body tissues can withstand the rather small fluctuations in the concentrations of hormones, ions, and nutrients that continually occur, particularly after eating or exercise. If the brain were exposed to such chemical changes, uncontrolled neural activity might result! Remember that certain ions are involved in initiating nerve impulses and some amino acids serve as neurotransmitters. Blood Brain Barrier Neurons are kept separated from bloodborne substances by a blood-brain barrier. Composed of the least permeable capillaries of the body. Only water, glucose and essential amino acids can easily pass through the walls of these capillaries. Metabolic wastes (urea, toxins, proteins, and most drugs) are prevented from entering the brain. Blood Brain Barrier The following contribute to the barrier: 1. Astrocytes 2. Relative impermeability of the capillaries Most responsible for providing this protection Useless against some substances Fats and fat soluble molecules Respiratory gases Alcohol Nicotine Anesthesia Traumatic Brain Injuries Concussion Slight brain injury May be dizzy, “see stars”, or lose consciousness briefly No permanent brain damage Contusion Nervous tissue destruction occurs Nervous tissue does not regenerate Shows an area of subarachnoid hemorrhage with bleeding and an area of brain contusion where the white ischemic brain has died Traumatic Brain Injuries Cerebral Edema – Swelling of the brain due to inflammatory response to injury Hemorrhaging – Bleeding from ruptured vessels Traumatic Brain Injuries After head blows, death may result from intracranial hemorrhage or from cerebral edema. Both may compress and kill brain tissue Individuals who are initially alert and lucid following head trauma and then begin to deteriorate neurologically later are most likely hemorrhaging or suffering the consequences of edema. Cerebrovascular Accident (CVA) Commonly called a stroke Third leading cause of death in the US Occur when blood circulation to a brain area is blocked (blood clot or a ruptured blood vessel) Brain tissue supplied with oxygen from that blood source dies Loss of some functions or death may result Cerebrovascular Accident (CVA) • Fewer than 1/3 of those surviving a CVA are alive 3 years later. • Some patients recover at least partly, because undamaged neurons spread into areas where neurons have died and take over some lost functions. • Most of the recovery seen after brain injury is due to this phenomenon. Alzheimer’s Disease Progressive degenerative brain disease that ultimately results in dementia (mental deterioration) Structural changes in the brain include abnormal protein deposits and twisted fibers within neurons Alzheimer’s Disease Mostly seen in the elderly, but may begin in middle age Victims experience memory loss, irritability, confusion and ultimately, hallucinations and death 5-15% of people over 65 develop this condition. Parkinson’s Disease Cause: Results from a degeneration of the dopamine-releasing neurons, and as those neurons degenerate, the dopamine-deprived basal nuclei they target become overactive Typically strikes people in their 50s and 60s (Michael J. Fox is an exception) Cause of Parkinson’s is still unknown Parkinson’s Disease Symptoms include: 1. Persistent tremor at rest exhibited by head nodding and “pill-rolling” movement of the fingers 2. Forward-bent walking posture and shuffling gait 3. Stiff facial expression 4. Trouble initiating movement or getting their muscles going Huntington’s Disease Genetic disease that leads to massive degeneration of the basal nuclei and later of the cerebral cortex Strikes during the middle age Symptoms: Initial - wild, jerky, and almost continuous flapping movements Later - marked mental deterioration Progressive and usually fatal within 15 years of onset of symptoms Treatment of Parkinson’s and Huntington’s Disease Parkinson’s Disease Signs and Symptoms – Inhibition of the motor drive Treatment – Usually treated with drugs that enhance dopamine’s effects Huntington’s Disease Signs and Symptoms - Overstimulation of the motor drive (opposite of Parkinson’s disease) Treatment – Usually treated with drugs that block dopamine’s effects