History and Examination in Ophthalmology
advertisement

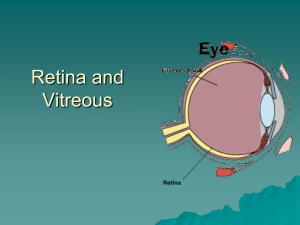
Flashes and Floaters Hong Woon SJUH Flashes and Floaters Flashes AND Floaters occurring together • Virtually pathognomic for Posterior Vitreous Detachment Flashes and Floaters • • • • ΔΔ Flashes or Floaters Posterior Vitreous detachment Migraine Aura Other causes of flashes and floaters • Taking a history of flashes or floaters • When to refer Flashes • • • • • • • • • • • • or PVD Disciform Choroidal melanoma CMV retinitis CRVO Digoxin toxicity Optic nerve compression Optic neuritis AION Pituitary tumour Migraine Aura Charles Bonnet Syndrome Floaters • • • • • • • Vitreous syneresis PVD Vitreous haemorrhage Asteroid hyalosis Posterior uveitis Entopic phenomenon CMV retinitis • Know how to diagnose confidently – PVD – Migraine aura without headache • High index of suspicion not PVD or migraine aura if: – Unusual features to flashes or floaters – Other symptoms Posterior Vitreous Detachment (PVD) • Anatomy of vitreous • Mechanism of PVD • Epidemiology • Symptoms • Signs • Complications Anatomy of vitreous • Mainly water (99%) • Collagen filaments and hyaluronic acid • Strongly attached at vitreous base • Firm attachments at optic disc • Attachments to retina decrease with age Vitreous degeneration and syneresis • Depolymerisation of hyaluronic acid – Release water – Pockets of liquefied vitreous • Collagen filaments aggregate – Fibrils – Collapse of gel (syneresis) – Visible as small floaters Posterior Vitreous Detachment • Posterior vitreous detached from retina – – • Accumulation of lacunae Fluid escapes into retrohyaloid space Large floater – – Weiss’ ring Posterior hyaloid membrane PVD: predisposing factors • • • • • Age Myopia Cataract surgery Trauma Posterior uveitis PVD: natural aging change 60 50 Percent with PVD 40 30 20 10 0 < 50 yrs 50 - 60 60 -70 > 70 Age yrs • If PVD present 73% chance of PVD in fellow eye if greater than 60 years of age Symptoms of PVD • • • • • None Flashes alone Floaters alone Flashes and Floaters Symptoms of complication – Vitreous haemorrhage – Retinal detachment Photopsia from PVD • Peripheral arcs of light (Moore’s lightening streak) • Occurs on eye movement • Dim – seen best in dim lighting • Very brief, but recurrent • Usually precedes onset of floaters • May persist for months or years Floaters from PVD • Sudden onset floater • Much more prominent than small floaters from vitreous syneresis • Due to Weiss’s ring or prominent posterior hyaloid membrane • May be described as curtain or shadow or blurring of vision • Can see through curtain or around shadow Acute complications of PVD Vitreous haemorrhage Retinal tear Retinal detachment Symptoms of Vitreous haemorrhage • Little spots/ Rain drops/ Sand storm – Due to seeing individual red cells • Black streaks – Streaks of blood • Extensive loss of vision – Large vitreous haemorrhage • Increased risk of retinal tear and retinal detachment Symptom of Retinal tear • No symptom from tear alone • ~ 50% risk progression to Retinal detachment • May be associated with small vitreous haemorrhage Retinal detachment? • Retinal tear allows retina to separate from retinal pigment epithelial layer • Retina dependant on RPE and choroid for function • Detachment gives rise to loss of function of detached area. Symptom of Retinal Detachment • Shadow • Progressive • Requires urgent surgery • Visual prognosis best if macula not detached Symptomatic Posterior Vitreous Detachment • Risk of developing retinal tear ( ~ 8%) • Risk of developing RD: 3 – 7% in symptomatic PVD • If RD develops, it usually occurs within 6 weeks Migraine aura without headache • Any age but more common with increase age (~ 1% > 50 years of age) • 77% first occurrence after 50 years of age • 42% no history of migraine • 44% migraine with aura sufferers report aura without headache at times Migraine aura without headache • Wave of depolarisation across cortex including occipital lobe • Slowly evolving nature of visual symptoms Forms of migraine aura • Photopsia – Unformed flashes of light • Fortification spectrum – White or coloured • Scotoma – Often crescent shaped and shimmering • Heat waves/ blurring/ hemianopsia Migraine aura • Dynamic: grows and moves across visual field over minutes • Hononymous but may be difficult for patient to appreciate • Spectrum of patterns but usually more formed than photopsia due to PVD and may be coloured Other Conditions Atypical flashes or atypical floaters or other symptoms • • • • • • • Optic neuritis Photopsia and blunt trauma Toxic, inflammatory or inherited retinal conditions CMV retinitis Vitreous syneresis Asteroid hyalosis Posterior uveitis Optic neuritis • Photopsia present in 70% • Sparks Flickering peripheral vision • May be precipitated by eye movement • Main symptom will be blurring of vision Photopsia following blunt trauma • Indicates VR traction • Can develop retinal tears without full PVD • Must examine retinal periphery Toxic, inflammatory, inherited retinal conditions • Small, shimmering, blinking lights • In affected field of vision • Persistent CMV retintis • Flashes • Floaters • Vision not affected until macular involved • Only in HIV or immunosuppressed patients Vitreous syneresis • Small multiple floaters • Lines / tadpoles • Seen best against bright background • Move with eye • Increased with myopia Asteroid hyalosis • Uncertain pathogenesis • Degeneration – Age > 60 yrs – Calcium laden lipids • Usually unilateral • Remarkably few symptoms Posterior uveitis • Idiopathic / toxoplasmosis • Very large numbers of small spots – individual cells • + larger floaters • Similar symptoms for small vitreous haemorrhage Taking a history of flashes of light • What are the flashes of light like? – Arc of light / jagged / colours / brightness – Where in the vision are they? – How long does it last for? – How does it develop? – Is the vision affected? • When do the flashes occur? – Eye movement – At night • Timing? – How often do they occur? – When did they first start? • Associated features? Taking a history of floaters • What are the floaters like? – Size? – Number? – See through? – Movement? • Are there any flashes of light? • Is the vision affected? • Timing – When did they start? • Associated features? – Retinal detachment – Myopia – Eye surgery Why refer PVD? • To exclude retinal tear / retinal detachment • Retinal tear should be treated before retinal detachment develops • Retinal detachment should be treated before macular involvement • Surgery may be considered for floater in exceptional cases with persistent symptoms When to refer PVD? • Symptoms of vitreous haemorrhage – Rain drops / dark streaks • Symptoms of retinal detachment – Shadow • Recent history – < 6 weeks • High myopia / history of RD in fellow eye What do we do with PVD? • Dilated examination – Confirm diagnosis – Exclude retinal tear / retinal detachment • Discharge – Advised to return if new symptoms (increase in floaters/ shadows) – Surgery for floater only in exceptional cases and only when symptoms persist Summary • Flashes and floaters often due to PVD • Flashes alone may be due to migraine aura without headache • Small risk if retinal tear and retinal detachment • Ask for symptoms or history which may increase risk of retinal tear/ retinal detachment • Risk of retinal detachment considerably reduced if symptoms greater than 6 weeks