Macular Surgery - Back to Medical School
advertisement
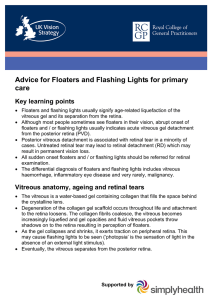
Ophthalmic Emergencies How to avoid missing a serious and treatable condition Hong Woon SJUH, Leeds Ophthalmic Emergencies • Ophthalmic emergencies with obvious clinical signs • Ophthalmic emergencies without obvious clinical signs Alkali burns • Fertilizers and cleaning products/ drain and oven cleaners/ cement • Must treat immediately with irrigation before referring on. • Irrigate with copious amounts of water/ buffer solution until pH normal • Untreated can become blind due to stromal damage and ischaemia Beware infection in CL wearer of if recent operation • Painful red eye: - may indicate infective keratitis/ endophthalmitis • Urgent treatment required Dendritic ulcers • Self limiting • Problem occurs if treated with topical steroids Ophthalmic emergencies without obvious clinical signs Choices: 1. Make diagnosis from examination – Become competent at slit lamp and fundus examination 2. Make diagnosis from symptoms – Learn to take a good history What to ask for when taking a history of visual loss? • Character of visual loss may help identify location of disease: – – – – Extent of visual loss: sharpness / darkness / field loss Blurred vision: Out of focus / Distorted vision Floater Glare / Halos • Timing: onset / progressive / transient • Associated factors: pain / headache Extent of visual loss • Very important clue about severity of problem • Ask about vision of each eye • Vision of less than CF is indicative of serious disease • But remember serious disease can also be present if vision is good Quantify extent of visual loss with vision test • Sit patient at correct distance from chart • Test each eye individually • Ask patients to use distance glasses • Use pinhole if no glasses • If unable to see any letters – ? CF, ?HM, ?PL • Compare with previous vision Blurred vision • Out of focus / not sharp • No distortion • Refractive problem – Cornea – Lens – Shape of eye • Macular problem Distortion of vision (Metamorphopsia) • Things look wavy, jumbled up. Lines not straight. Kink in lines • Condition affecting retina – Wet macular degeneration – Macular hole – Macular pucker – Retinal detachment Field defect • Curtain, bit missing, bump into things • Always a sign of serious problem • If homonymous: -same visual field both eyes – Defect of visual pathways • Not hononymous – Retinal – Optic nerve Shadow in the eye • Retinal detachment • Glaucoma • Vitreous haemorrhage • Vascular lesion • Optic nerve disorder • Visual pathway problem Floater • Due to opacity in vitreous • Fly/spider, blob, haze • Movement Floaters • PVD – May notice Weiss’ ring • Syneresis • Vitreous haemorrhage – Rain drops – Black streaks • Posterior uveitis Flashes • PVD – Moores lightening streak – Peripheral scintillation with eye movement • Migraine – Scintillating scotoma – Fortification spectrum • Mass lesion • Retinal ischaemia Glare • Difficulty seeing in bright light – Low sun – Driving at night – Fluorescent light in supermarkets • Corneal or lens problem – Often due to cataract • Vision may be good otherwise “Halos” in acute glaucoma • Not strictly a halo – diffraction of light by ice crystals • Coloured rings around lights due to refraction by water droplets • Not to be confused with glare due to scatter by corneal or lens opacities Reduced colour sensitivity • Things look darker / less colour • Optic nerve disease – Optic neuritis – Compressive optic nerve disease • Condition affecting retina – Wet macular degeneration – Central serous retinopathy Timing of visual loss • Recent or chronic • Static or progressive • Transient or persistent • Very important in determining urgency of situation Conditions causing sudden visual loss • Vascular occlusion – Central retinal artery occlusion – Central retinal vein occclusion – Anterior ischaemic optic neuropathy • Vitreous haemorrhage • Acute glaucoma Conditions causing rapid progressive visual loss • Retinal detachment • Wet macular degeneration Causes of transient visual loss • Amaurosis fugax • Subacute angle closure glaucoma • Visual obscuration due to papilloedema • Giant cell arteritis • Floaters • Ocular surface problem Symptoms suggestive of urgent condition • • • • • Marked visual loss Field loss Floaters/Photopsia Distortion of vision Transient marked loss of vision • Recent change • Rapidly progressive change Ophthalmic emergencies without obvious clinical signs • • • • • • • Subacute angle closure glaucoma CRAO AION Wet macular degeneration PVD with retinal tear/detachment Retinal detachment Trauma • CRVO • Neurological conditions presenting with eye signs/symptoms Subacute angle closure glaucoma • Acute angle closure glaucoma – ophthalmic emergency with obvious clinical signs – Red eye – Painful eye – Severe visual loss in affected eye • Often premonitory episodes of subacute angle closure glaucoma Subacute angle closure glaucoma • Angle closure develops in evenings when pupil dilates – Pressure increases to give pain and corneal oedema – Patient sees blurred vision and haloes around lights • Patient goes to bed – Sleep induced miosis aborts attack of glaucoma – Normal eye next day • Should be referred urgently before established AACG develops Treatment of to prevent angle closure glaucoma • YAG PI • Laser treatment • PI prevents build up of aqueous behind pupil Central retinal artery occlusion • Sudden severe visual loss • Visual loss may not be total due to cilioretinal artery • Usually embolic, rarely due to GCA • Attempt to reperfuse artery if within 24 hours of onset • Should be seen urgently to exclude GCA and identify cause • No recovery of vision • Often premonitory symptoms Amaurosis fugax • Transient visual loss due to passage of emboli through central retinal artery • Recovery to normal vision unless permanent central retinal artery occlusion develops • Often no emboli visible on clinical examination • Total or altitudinal visual loss in one eye for a few minutes • Visual recovery often described like a curtain lifting • Aspirin very effective in preventing CRAO Cause of CRAO is usually carotid disease • Risk factors: – Hypertension, Smoking, Diabetes, High Cholesterol • • • • Risk of further emboli to eye or brain Reduce risk factors Antiplatelet agents Carotid endarectomy if greater than 70% stenosis Anterior ischaemic optic neuropathy • Infarction of optic nerve head - pale swollen disc with visual loss. • Sudden severe visual loss if entire disc affected, altitudinal defect if only one short posterior ciliary artery occluded Anterior ischaemic optic neuropathy • No treatment for affected eye • 75% due to atherosclerosis in middle aged smokers • 25% due to Giant cell arteritis headache, tenderness of temporal arteries, malaise, raised ESR . • AION due to GCA is emergency high risk of developing AION in fellow eye Wet macular degeneration 1. Serous elevation of retina or PED 2. Blurred vision and distorted vision 3. Usually progressive over weeks 4. Difficult to see with ophthalmoscope 5. Initial vision may be very good Wet ARMD • Highly likely to progress to severe visual loss if untreated • Recovery of vision best if treated before chronic changes have developed • Treatment not recommended for late cases Treatment of CNM with intravitreal injection of antiVEGF • VEGF (vascular endothelial growth factor) stimuates growth of choroidal neovascular membrane • antiVEGF binds to VEGF and prevents it acting on CNM • Visual loss can be reversed if caught early Incidence of PVD Diagnosis of posterior vitreous detachment • Flashes and floaters • Weiss’ ring • Age, myopia, cataract operation • Examination – Weiss’s ring – Posterior hyaloid membrane 80 60 40 20 0 10-45 yrs 46-65 yrs 66-86 yrs Symptomatic Posterior Vitreous Detachment • Risk of developing retinal tear (8-22%) • Risk of developing RD: 3 – 7% in symptomatic PVD • If RD develops, it usually occurs within 6 weeks Symptomatic Posterior Vitreous Detachment Indications for urgent referral • Recent history (? Within 6weeks) • Symptoms suggestive of vitreous haemorrhage • Symptom of retinal detachment Reason for urgent referral • To pick up retinal tear before retinal detachment • Early treatment of retinal detachment Penetrating ocular injury • Suspect if history of high velocity fragment – ie metal on metal fragment • May be minimal external eye signs. Symptoms suggestive of urgent condition • • • • • Marked visual loss Field loss Floaters/Photopsia Distortion of vision Transient marked loss of vision • Recent change • Rapidly progressive change