Vitreoretinal / Ocular Trauma - Sight Loss and Vision Priority Setting
advertisement
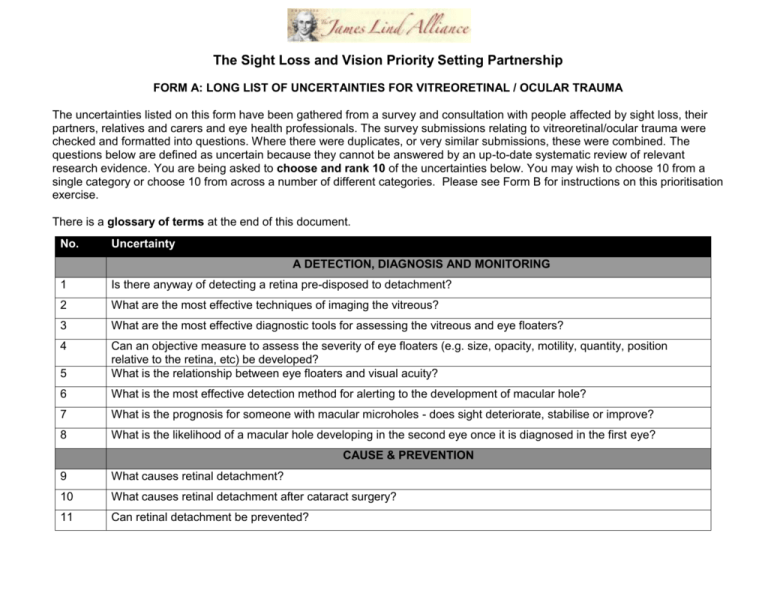
The Sight Loss and Vision Priority Setting Partnership FORM A: LONG LIST OF UNCERTAINTIES FOR VITREORETINAL / OCULAR TRAUMA The uncertainties listed on this form have been gathered from a survey and consultation with people affected by sight loss, their partners, relatives and carers and eye health professionals. The survey submissions relating to vitreoretinal/ocular trauma were checked and formatted into questions. Where there were duplicates, or very similar submissions, these were combined. The questions below are defined as uncertain because they cannot be answered by an up-to-date systematic review of relevant research evidence. You are being asked to choose and rank 10 of the uncertainties below. You may wish to choose 10 from a single category or choose 10 from across a number of different categories. Please see Form B for instructions on this prioritisation exercise. There is a glossary of terms at the end of this document. No. Uncertainty A DETECTION, DIAGNOSIS AND MONITORING 1 Is there anyway of detecting a retina pre-disposed to detachment? 2 What are the most effective techniques of imaging the vitreous? 3 What are the most effective diagnostic tools for assessing the vitreous and eye floaters? 4 5 Can an objective measure to assess the severity of eye floaters (e.g. size, opacity, motility, quantity, position relative to the retina, etc) be developed? What is the relationship between eye floaters and visual acuity? 6 What is the most effective detection method for alerting to the development of macular hole? 7 What is the prognosis for someone with macular microholes - does sight deteriorate, stabilise or improve? 8 What is the likelihood of a macular hole developing in the second eye once it is diagnosed in the first eye? CAUSE & PREVENTION 9 What causes retinal detachment? 10 What causes retinal detachment after cataract surgery? 11 Can retinal detachment be prevented? No. Uncertainty 12 Are there any dietary choices or supplements that could help stop retinal detachments? 13 Are there any exercises that could help stop retinal detachments? 14 What causes vitreous syneresis/degenerative vitreous? 15 How can vitreous syneresis/degenerative vitreous be prevented? 16 What causes vitreous opacities/eye floaters? 17 Can other health problems contribute to vitreous opacities/floaters? 18 How can vitreous opacities/eye floaters be prevented? 19 Can dietary and lifestyle choices prevent vitreous opacities/eye floaters? 20 Why are some people better able to cope with the distress caused by vitreous opacities/eye floaters? 21 Why can vitreous opacities/eye floaters be different across the two eyes, or only perceived in one eye? 22 How does aging affect vitreous opacities/eye floaters? 23 How does exposure to light (e.g. natural vs artificial spectrum) affect vitreous opacities/eye floater symptoms? 24 Why are the symptoms of vitreous opacities/eye floaters less noticeable when you are engaged in another activity (such as reading or watching TV)? Why do vitreous opacity/eye floater characteristics - opacity, motility, quantity, position, size, shape, colour vary so much from person to person? What causes posterior vitreous detachment? 25 26 28 What is the relationship (e.g. prevalence, time-frame, causal factors) between vitreous syneresis, posterior vitreous detachment and retinal detachment? Why does the likelihood of cataract formation increase after vitreous removal? 29 Can epiretinal membrane/fibrosis be prevented from happening? 30 What causes eye floaters and flashes of light? 31 What is the relationship between eye floaters and hyperesthesia? 32 What is the relationship between people experiencing troublesome eye floater symptoms and obsessive personality traits/psychological disorders? 27 No. Uncertainty 33 What is the effectiveness of diet or vitamin supplements in preventing posterior vitreous detachment? 34 How can vitreous detachment be prevented? 35 Are there environmental or genetic factors that predispose to macular holes? 36 Are there lifestyle, environmental or genetic factors that predispose to macular micro holes? TREATMENT 37 How can the risk of losing sight for people with retinal detachment be reduced? 38 How can the success rate of surgery for retinal detachment be improved? 39 Can vision be restored for people whose retina was detached many years ago? 40 How can epiretinal membrane/fibrosis be treated? 41 Can a cure be developed for vitreous syneresis/degenerative vitreous/eye floaters? 42 Can better interventions be developed that are effective in treating vitreous opacities/eye floaters? 43 45 Can lifestyle changes, supplements, herbal remedies or complementary therapies improve the quality of life for people with vitreous opacities/eye floaters? What is the effectiveness of different management strategies to help people cope with vitreous opacities/eye floaters? What can influence whether vitreous opacities/eye floaters worsen or not over time? 46 How can the vitreous be repaired or regenerated? 47 Is there an alternative treatment to surgery for symptoms of vitreous syneresis/degenerative vitreous? 48 49 What is the effectiveness of inducing a posterior vitreous detachment compared to leaving the vitreous attached to the retina and removing as much vitreous from the inner part of the eye as possible for people with degenerative vitreous? What is the most effective treatment for epiretinal membrane/fibrosis? 50 What is the most sensitive and valid measure of an eye-floater patient's benefit from treatment? 51 What factors are important in deciding whether to surgically treat patients with eye floaters? 44 No. Uncertainty 52 Can a functioning prosthetic eye be developed to replace an eye damaged by injury? 53 Can stem cells be used to regrow an eye or part of an eye damaged by injury? 54 Can surgical techniques be improved to save sight for eyes damaged by injury? 55 Can an optic nerve damaged by injury be regenerated? 56 What is the most effective and safe treatment for macular holes? 57 How effective are treatments for macular hole for symptoms of distortion? 58 Can effective anti-scarring agents be developed for macular hole surgery? 59 How can macular hole be prevented from developing again after surgery? Glossary of terms: Complementary therapies: Forms of treatment that do not eradicate the cause of a condition but can help relieve symptoms. Environmental factors: Outside influences on health such as social circumstances, drugs, diet etc. Genetic factors: Influences on health caused by genes for a particular trait. Hyperesthesia: A condition that is characterised by a heightened sensitivity to stimuli of the sense. Imaging: Techniques to gain visual images of the eye. Opacity: The measure of an object’s impenetrability to light. Optic nerve: The nerve that attaches the eye to the brain. Prosthetic: An artificial device that replaces a missing body part. Stem cells: Cells that have the potential to become any type of cell in the body. Visual acuity: The clearness or acuteness of an individual’s vision. Vitreous: A thick gelatinous, transparent substance that fills the space between the lens and the retina.