Chargemaster-It`s Importance in Healthcare!
advertisement

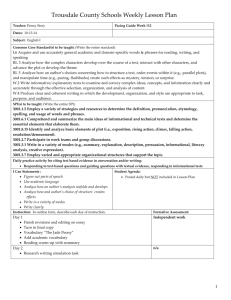
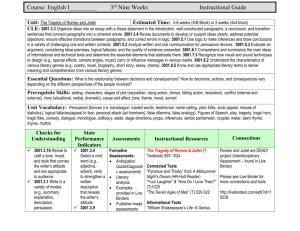
* Lisa Poworoznek Director, Budget & Reimbursement Finger Lakes Health May 22, 2014 Charge Code Description Department # Facility assigned mnemonic, unique to one service “Patient Friendly” description General ledger department service performed within Relative Value Unit RVU Revenue Code CPT/HCPCS Multipliers 3 digit code categorizing the service: National Uniform Billing Committee Procedural Coding Systems: CPT – AMA Pharmacy option – matches order to code Adds additional procedure explanation Modifiers Charge Amount Exploding Rules HCPCS – CMS CPT = Current Procedural Terminology HCPCS = Healthcare Common procedure Coding System Financial fee assigned to line item One charge code for two procedures always performed together * * Exhibit 51 - ICR PROVIDER NO. XX-XXXX NEW YORK STATE DEPARTMENT OF HEALTH VERSION: 2013.01 PERIOD FROM 01/01/2012 TO 12/31/2012 INSTITUTIONAL COST REPORT 05/31/2013 08:17:05 RATIO OF COST TO CHARGES - OUTPATIENT CHARGE MAPPING (REVENUE CODES) - PART III EXHIBIT 51 COST CENTER GROUP 45020 39 72 56 72 30 39 20 47 36 76 20 72 78 62 17 47 11 30 17 33 33 41 17 43 76 REVENUE CODE 987 976 960 921 841 762 731 700 618 559 482 460 440 421 402 369 352 335 320 309 301 272 255 171 120 COST CENTER GROUP 45020 19 17 55 56 30 47 20 61 36 56 20 21 45 62 17 47 11 30 33 33 33 41 61 39 70 REVENUE CODE 986 972 943 920 804 761 730 637 615 510 481 450 434 420 401 362 351 331 319 307 300 270 252 141 118 * COST CENTER GROUP 45020 20 33 85 21 30 47 15 61 36 56 20 78 45 72 09 17 11 17 33 33 41 61 61 70 39 REVENUE CODE 985 971 942 900 803 750 729 636 612 509 480 444 431 419 391 361 350 324 312 306 278 264 251 128 116 COST CENTER GROUP 45020 89 47 47 30 30 89 15 41 36 47 78 78 45 72 09 47 44 17 33 33 41 47 61 39 39 REVENUE CODE 982 964 941 851 801 740 720 622 611 490 471 443 430 410 390 360 343 323 311 305 276 260 250 122 111 COST CENTER GROUP 45020 21 21 47 30 61 20 47 41 36 20 43 78 62 17 47 11 44 17 33 33 41 61 40 39 76 REVENUE CODE 981 961 940 845 771 732 710 621 610 483 470 441 424 403 370 359 341 322 310 302 275 259 200 121 110 Department Ownership Not Charged – Didn’t Happen Percent of Charge Payments Reduces AR Future Rates RCC * * MAC – Medicare Administrative Contractors * CERT – Comprehensive Error Rate Testing Contractors * ZPIC – Zone Program Integrity Contractors * SMRC – Supplemental Medical Review Contractors * Commercial Payors * OIG – Office of Inspector General * DOJ – Department of Justice * OMIG – Office of Medicaid Inspector General * MIP – Medicaid Integrity Plan * Self Pay Patients * Media * Watch Groups * “The second reason the compilation and release of this data is a big deal is that it demonstrates the point I tried to make in spotlighting the seven sample medical bills in Time’s “Bitter Pill” report: most hospitals’ chargemaster prices are wildly inconsistent and seem to have no rationale. Thus the release of this fire hose of data— which prints out at 17,511 pages—should become a tip sheet for reporters in every American city and town, who can now ask hospitals to explain their pricing.” The U.S. Department of Health and Human Services is releasing the "chargemaster" price list of the 100 most common inpatient procedures for all U.S. hospitals, inspired by Time's March 4 expose on hidden medical billing. * May 1, 2014 Medicare IPPS Proposed Rule Includes Significant Payment Changes for FFY 2015 * The Affordable Care Act (ACA) requires that hospitals "for each year establish (and update) and make public (in accordance with guidelines developed by the [Health and Human Services] Secretary) a list of the hospital's standard charges for items and services provided by the hospital, including for diagnosis-related groups established under Section 1886(d)(4) of the Social Security Act.“ * Until now, CMS has not issued the required guidelines. In the rule, CMS is "reminding hospitals of their obligation to comply" with this requirement. CMS states that its guidelines are "that hospitals either make public a list of their standard charges (whether that be the chargemaster itself or in another form of their choice), or their policies for allowing the public to view a list of those charges in response to an inquiry." CMS does not provide a deadline for compliance, but expects that hospitals will update the information at least annually, or more often as appropriate, to reflect current charges. * HIM Registration Billing Chargemaster Department Managers Compliance * Clinical Order Entry System • Which is in tandem with: Medical Record HIM/Coding * • Which then ties to the: Chargemaster • Which maps with: Billing * Keeping Abreast of New Coding Regulations * Assess Contractual Issues for Impacts * Education Opportunities * Evaluate Current Charge with Active Listening * Charge Forms/Tickets – Process Review * Partner with Billing to Assist and Ensure “Clean Claims” * * Recommends Action to Avoid Compliance Concerns * Directs Chargemaster Review Team in Ongoing Refinements * Liaison between Finance and Clinical * Develop Policies and Procedures * Maintance – Qtrly CMS, Monthly Bulletins * Evaluate Additional Charge Capture Possibilities Incorrect Multipliers Missing CCodes Edits/Denials Injectable Drugs with no Injection Charge Setting Implications Revenue Center Mismatches * Outdated Codes * * * *Medicare Guidelines state routine supply charges will be bundled into the procedure, room rate or leveling system. - Routine Items: Gowns, Gloves masks, Blood Pressure Cuffs, Ice Bags, IV Tubing, Pillows, Towels, Thermometers, Wash Clothes, Soaps, Bed Linen, Diapers, Tourniquet, Gauze, Band Aids, Oxygen Masks, Syringes, Wall Suction, Drapes, Cotton Balls, Marking Pens, Pads, Urinals, Wipes, Toothbrushes, Shaving Kits, Chucks, Shampoo, Etc…… * Is this for a specific patient? Non, Billable, Item is Routine No Is the item reusable? Yes Is there a Physician order: Written, Verbal or Implied? No Is medical necessity properly documented? No Non Billable, Bundled into room/procedure Non Billable, Personal Non billable Without What category does this fall into? Take Home If needed to facilitate discharge * Implant Low Cost Set Up Tray/Kit Procedure Tray/Kit Unique Item or ordered off shifts Track Independently for ICR Decide threshold – Bundle Preparation kits are not chargeable Review each item in kit: Ccodes Communication Emergency Department Charges December 2013 YTD Stats DEPT. MNEM. PROCEDURE **3001 30010014 CUTDOWN >1YR VENIPUNCT **3001 30010015 ARTERIAL PUNCTURE **3001 30010016 INTRAOSSEOUS NEEDLE IN **3001 30010034 REMOVE FB EAR **3001 30010035 REMOVE CERUMEN **3001 30100001 SUTURE REMOVAL **3001 30010001 ED VISIT LEVEL 1 **3001 30010094 HAND STRAPPING **3001 30010091 APPLY FINGER SPLINT **3001 30010085 EVAL SUBUNGAL **3001 30010039 REMOVE CORNEAL FB W SL **3001 30010036 REMOVE FB EYE-SUPERFIC **3001 30010038 REMOVE CORNEAL FB * TECHNICAL CHARGES 2013 2013 2013 QTY CHARGE TTL CHRGS CPT REV SI 1 $40 $40 36425 450 X 6 $50 $300 36600 450 Q3 9 $450 $4,050 36680 450 X 5 $140 $700 69200 450 X 8 $14 $112 69210 450 X 89 $180 $16,020 99281 450 V 82 $180 $14,760 99281 450 V 1 $190 $190 29280 450 S 29 $169 $4,901 29130 450 S 1 $84 $84 11740 450 T 2 $271 $542 65222 450 S 2 $271 $542 65205 450 S 1 $271 $271 65220 450 S RVU 0.3042 0.3042 0.7353 0.7353 0.7353 0.7658 0.7658 0.7685 0.7685 0.8370 1.0663 1.0663 1.0663 MU 1.00 1.22 1.00 1.00 1.04 1.00 1.00 1.00 1.09 1.27 1.00 1.00 UNIT EXTENDED MCR BLUES Mark Up RECOMMEND COST COST REIMB REIMB to MCR CHARGE $14.00 $14 $20.47 $24.00 3.4 $70.00 $14.00 $84 $20.47 $30.00 3.4 $70.00 $33.84 $305 $49.48 $270.00 3.4 $169.20 $33.84 $169 $49.48 $84.00 3.4 $169.20 $33.84 $271 $49.48 $8.40 3.4 $169.20 $35.24 $3,137 $51.53 $108.00 3.4 $176.22 $35.24 $2,890 $51.53 $108.00 3.6 $183.00 $35.37 $35 $51.71 $114.00 3.4 $176.84 $35.37 $1,026 $51.71 $101.40 3.4 $176.84 $38.52 $39 $56.32 $50.40 3.4 $192.60 $49.07 $98 $71.75 $162.60 3.4 $245.37 $49.07 $98 $71.75 $162.60 3.4 $245.37 $49.07 $49 $71.75 $162.60 3.4 $245.37 * Hard Coding: For procedures performed the exact same way on every patient. Applied by clinical personal performing the procedure. 70,000 – 90,000 codes Assumes documentation is present to support code * Soft Coding: Medical record reviewed by coder and a procedure code is applied from documentation – Mainly used with surgical codes 10,000 – 60,000 * Collision Coding- Clinical applies hard code while HIM also soft codes, results in duplicate charges. Watch for these situations. * * - Encourages staff to perform and/or “check off” services that are not required in order to validate productivity - Additional maintenance as line items grow - Charge for services without medical necessity - No substantiating documentation - Stat definition varies from revenue definition * HIM Registration Billing Chargemaster Compliance * Department Managers * Lisa Poworoznek Director, Budget & Reimbursement Finger Lakes Health lisa.poworoznek@flhealth.org *