CerebPharm-1 - Anesthetist Student Blog
advertisement

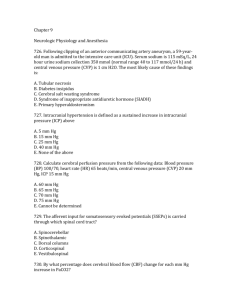
Cerebral Pharmacology and Anesthesia for Supratentorial Craniotomy Mani K.C Vindhya M.D Asst Prof of Anesthesiology Nova Southeastern University Introduction to Cerebral Pharmacology. In addition to anesthetic agents and neuromuscular junction blockers, don’t forget: Drugs to decrease brain interstitial fluid Dexamethasone (edema around solid brain tumors) Mannitol and hypertonic saline (osmotic diuretics) Furosemide (loop diuretic) Antibiotics – usually two for intracranial neuroanesthesia Nafcillin or oxacillin (or vancomycin, if penicillin allergic) Gentamicin Qualities of an Ideal Neuroanesthetic Maintenance of mean arterial pressure and cerebral perfusion pressure Decrease in intracranial pressure (ICP) Decrease in cerebral metabolic rate coupled with decrease in cerebral blood flow Decrease in CSF volume (production < reabsorption) No inhibition of cerebral autoregulation No expansion of closed air spaces Rapid emergence Anticonvulsant Lack of toxicity to major organ systems Cerebroprotective (or at least not harmful) Compatibility with neuromonitoring (such as SSEP’s) Maintenance of Mean Arterial Pressure and Cerebral Perfusion Pressure CPP = MAP - ICP (or CVP, whichever is greater) Change in MAP Inhaled Anesthetics Increase N2O Little change Intravenous Anesthetics Etomidate Opioids Decrease Halothane Isoflurane Desflurane Sevoflurane Large Decrease Enflurane Thiopental Propofol Decrease in ICP and Cerebral Blood Flow All inhaled anesthetics (in high concentrations) increase CBF. All IV anesthetics (except ketamine) decrease CBF. The volatile agents have a biphasic effect on CBF in normal subjects Effects of volatile agents on CBF and CMR in normal subjects (coupling intact): CMR CBF Effects of volatile agents on CBF if coupling is impaired or if CMR is already suppressed: CBF CMR Decrease in Cerebral Metabolic Rate (CMRO2) coupled with decrease in Cerebral Blood Flow (CBF) Decrease in Cerebral Metabolic Rate (CMRO2) IV anesthetics – coupled with decreased CBF (metabolic effect) Volatile inhaled anesthetics - “uncoupling” of CBF from CMRO2 in high concentrations Only 2 anesthetics increase CMRO2 (coupled with an increase in CBF): Ketamine Nitrous oxide (N2O) Effects of Dexmedetomidine on CBF and CMR Dexmedetomidine decreases CBF and CBF velocity in humans. Dexmedetomidine did not reduce CMR in an animal model. A 2008 study showed that dexmedetomidine decreases both CBF velocity and CMR in humans • Decrease in CSF Production Relative to Reabsorption. – A decrease in CSF volume would tend to decrease intracranial volume and ICP. – Effects of anesthetics on CSF secretion and absorption ANESTHETIC SECRETION ABSORPTION Halothane Decrease Decrease Enflurane Increase Decrease Isoflurane --- Increase Desflurane Increase (hypocapnia only) --- Fentanyl --- Increase Etomidate Decrease Increase No Inhibition of Cerebral Autoregulation Autoregulation is intact with IV agents (i.e. thiopental, propofol, fentanyl) In high concentrations, all volatile inhaled anesthetics impair autoregulation No Expansion of Closed Air Spaces N2O = the only anesthetic that expands closed air spaces Intracranial air pockets Pneumocephalus Air emboli (venous or arterial) Teaching Points: Don’t turn on N2O at the end of case (but perhaps O.K. to leave it on during case). Don’t use in patients after recent craniotomy (i.e., air pockets on CT scan). . Rapid Emergence from Anesthesia (Lower Blood:Gas Solubility) Inhaled Agent B:G Solubility Halothane 2.4 Enflurane 1.9 (cf. MAC = 1.7) Isoflurane 1.4 (cf. MAC = 1.2) Sevoflurane 0.68 Nitrous oxide 0.47 Desflurane 0.42 Anticonvulsant Activity = desirable property Anesthetic Type Only proconvulsant activity Both pro- and anticonvulsant activity Only anticonvulsant activity Intravenous Methohexital Narcotics Etomidate* Diazepam Ketamine Propofol* Methohexital Thiopental Midazolam Inhalational Nitrous oxide Enflurane* Halothane Sevoflurane* Isoflurane (?) Desflurane (?) Isoflurane (?) Desflurane (?) Numerous case reports of convulsion-like muscle activity during induction and emergence from anesthesia with: Sevoflurane Enflurane Etomidate Propofol To prevent peri-operative drug-induced seizures in epileptic patients Continue anticonvulsant therapy. Consult with the patient’s neurologist to discuss management. Avoid etomidate. Do not use sevoflurane routinely in epileptic patients. Limit maximum concentration to < 1.5 MAC. Lack of toxicity to major organ systems 1. All of the volatile inhaled anesthetics can form toxic metabolites in CO2 absorbents (baralime > soda lime). A = compound A (vinyl compound produced by sevoflurane) B = BCDFE (vinyl compound produced by halothane) C = carbon monoxide (formed by pungent volatile anesthetics in the following rank order) D = desflurane > E = enflurane >F = Forane R (isoflurane) Many anesthetics are associated with potential organ toxicity: Sevoflurane – renal toxicity might be caused by: compound A from CO2 absorbents fluoride ion from hepatic metabolism Halothane > enflurane > isoflurane > desflurane Hepatotoxicity in proportion to hepatic metabolism Nitrous oxide – bone marrow toxicity Etomidate Adrenocortical suppression Propylene glycol toxicity caused by diluent Cerebroprotective (or at least not harmful) Thiopental = the “gold standard” for cerebral protection at the present time (i.e., during clipping of an intracranial aneurysm) Three agents may be harmful so far as cerebral protection is concerned: Ketamine Nitrous oxide Etomidate Compatibility with Neuromonitoring (such as somatosensory evoked potentials) Three kinds of evoked potentials: Evoked Potential Latency Anesthetic Interaction Brainstem auditory evoked response (BAER) 2 msec Barely affected Somatosensory evoked potentials, SSEPs (median nerve) 20 msec Somewhat affected Somatosensory evoked potentials, SSEPs (posterior tibial nerve) 40 msec Somewhat affected Visual evoked response (VER) 70-100 msec Very variable under anesthesia Effect of isoflurane on upper extremity SSEPs Summary of effects of anesthetics on SSEPs: Inhaled anesthetics – dose-related decrease in amplitude and increase in latency Less than 1 MAC volatile agent Nitrous oxide – profound depressant effect on SSEPs, especially when used in combination with volatile agent Intravenous agents: Propofol and thiopental – small decrease in amplitude and increase in latency. Propofol is commonly used for TIVA (total IV anesthetic) technique. Opioids – negligible effect on SSEP’s Ketamine and etomidate – increase SSEP amplitude. (Etomidate is exceptional. It increases SSEP amplitude but decreases BAEP amplitude). Summary. Six I’s that inhibit SSEP’s: Inhaled anesthetics (isoflurane and nitrous oxide) IV anesthetics (to a lesser extent than inhaled anesthetics). Ketamine and etomidate are the exceptions; they increase amplitude. Ischemia or hypoxia – anywhere from limb to cortex Injury – anywhere from limb to cortex Ice cold temperatures – < 34.5 oC “Incompetence” I.V. Induction of Anesthesia for Intracranial Neurosurgery Typical induction agents Thiopental, propofol, or etomidate =suitable I.V. induction agents Fentanyl or sufentanil – as narcotic analgesics to supplement Lidocaine IV – to blunt hypertensive and ICP response to intubation Neuromuscular junction blockers – rocuronium, vecuronium, or succinylcholine (with prior defasciculating dose of a competitive NMJB) Succinylcholine for intracranial neurosurgery 1. Increased CBF and ICP in dogs 2. Succinylcholine has been postulated to increase ICP by causing muscle afferent activity and stimulation of muscle spindle fibers (innervated by A-gamma fibers). A more recent study in patients with neurologic injury showed that succinylcholine did not change ICP, CBF velocity, or EEG activity. The increase in ICP induced by succinylcholine can be blocked with a defasciculating dose of NMJ blocker Teaching points: Don’t use succinylcholine if it’s contraindicated (i.e., hemiplegia). If OK, use succinylcholine if you’re at all worried about the airway. Use a defasciculating dose of a competitive neuromuscular junction blocker if you plan to use succinylcholine Maintenance of Anesthesia: How do the anesthetics stack up? Some agents we just don’t use: Ketamine Only cerebrovasodilating IV agent Increases CSF volume May cause neuronal damage due to its action on glutamate (N-methyl-D-aspartate, NMDA) receptors Halothane Most cerebrovasodilating inhaled agent (cortical CBF) Hepatotoxicity limits use in adults Enflurane – no longer in our O.R. Second most cerebrovasodilating inhaled agent, after halothane Increases CSF volume Epileptogenic (esp. with hypocarbia) Isoflurane, Sevoflurane, & Desflurane Bad Points: Decrease MAP (high concentrations) Increase CBF and ICP (high conc’s) Decrease CPP (high concentrations) Inhibit autoregulation (> 1% isoflurane) Good Points: Decrease CMRO2 No expansion of closed air spaces Easily titratable Desflurane Bad Points: Decreases MAP (so former PDR’s prohibited its use in intracranial neurosurgery) Maximum of 0.8 MAC recommended in current PDR Increased lumbar CSF pressure in one study but not in another more recent study in the setting of hyperventilation. ! Carbon monoxide (CO) production in CO2 absorbent is a concern. Coughing and bucking on emergence Very Good Point: Rapid emergence (allows for rapid wake-up at end of case) Sevoflurane Bad Points: EEG seizure activity has led to recommendation that sevoflurane not be used routinely in epileptics Possible nephrotoxicity is a concern: Fluoride ion production from hepatic metabolism Compound A production from CO2 absorbent Should not use for > 10 MAC hours (i.e., long neuro cases) Good Points: Rapid emergence (perhaps use at end of case) Pleasant odor (less coughing and bucking?) Favorable regarding CBF and autoregulation Nitrous Oxide Bad points: Increases CBF more than isoflurane on a MAC to MAC basis Increases CMRO2 (only I.A. that does) Expands closed air spaces (only I.A. that does) Tends to cause nausea and vomiting May cause neuronal damage due to its action on glutamate (N-methyl-D-aspartate, NMDA) receptors Good Points: MAP is maintained. Rapid emergence Easily titratable Many neuroanesthesiologists routinely used it in the past ! No difference in outcome of elective supratentorial craniotomy Propofol Good Points: Decreases CBF Decreases CMRO2 Autoregulation is preserved. Apparent antiemetic action Bad Points: Decreases MAP May have delayed emergence relative to inhalational techniques Anesthetic Opioids (Fentanyl, sufentanil, alfentanyl, remifentanyl) Good Points: Little change in CBF Less decrease in MAP Little change in CBF Autoregulation is preserved. Bad Points: Nausea and vomiting = a frequent S.E. Fentanyl was thought to be better than sufentanil or alfentanyl, based on their effects on MAP and CPP Sufentanil does not increase ICP in patients with brain injury so long as MAP is maintained Remifentanyl Good Point: A logical choice for rapid emergence Bad Points: Severe hypertension on emergence (recommended to give MSO4 prior to DC’ing remifentanyl) ? High incidence of post-op nausea and vomiting Anesthetic Management of Intracranial Neurosurgical Cases Reasonable Maintenance Regimens for Intracranial Neuroanesthesia (going from routine to desperate). N2O + isoflurane (½%) + fentanyl N2O = the first agent to go if there’s brain swelling or venous air emboli or ischemia danger (i.e. aneurysm or head trauma) MAC equivalents of sevoflurane or desflurane might also be substituted for isoflurane. Sufentanil could be substituted for fentanyl. Isoflurane (1%) + fentanyl Isoflurane (½%) + propofol + fentanyl Volatile agents are next to go if intractable ICP or brain swelling Total IV anesthetic: Propofol + fentanyl Barbiturate coma -- for intractible brain swelling or cerebral protection during aneurysm clipping (titrated to EEG burst suppression): Thiopental Pentobarbital Reasonable Muscle Relaxants for Maintenance of NM Blockade Vecuronium Rocuronium Pancuronium – increases HR Cis-atracurium: No histamine release (different from atracurium) An epileptogenic metabolite, laudanosine Special Cases in Neuroanesthesia • The ways to decrease intracranial volume and pressure apply in typical intracranial neuroanesthetic cases (i.e., supratentorial craniotomies). Three components inside the skull Brain (80% of ICV) ! Neurons, glia, extravasated cells ! Interstitial fluid CSF (8% of ICV) Blood volume (12% of ICV) ! Arterial side ! Venous side “Bad” Things that Increase ICV and ICP Ways to Decrease ICV and ICP Tumor Hemorrhage Head injury Surgical excision Evacuation of hematoma Temporal lobe decompression Edema Mannitol Hypertonic saline Furosemide Dexamethasone Obstructive hydrocephalus Spinal drain Ventriculostomy Increase CBF: Hypoventilation/ hypercarbia Hypoxia Heavy pre-medication Hyperthermia Inhibit cerebral venous drainage Decrease CBF: Hyperventilation/ mild hypocarbia Avoid hypoxia Anesthetic choice Avoid hyperthermia Improve cerebral venous drainage Transphenoidal Hypophysectomy = an exception. For resection of tumor confined to pituitary: No furosemide or mannitol Dexamethasone (solid brain tumor) Spinal drain (to put air or NSS in, not to take CSF out) No hyperventilation Quirk of Anesthesia after Recent Craniotomy Avoid N2O if air is inside skull on CT scan Quirks of Head Trauma (ABC’s of TBI) Airway. Safely get control. Blood pressure. Avoid hypotension (SBP < 90 mm Hg) if possible, or correct it immediately. CO2. Don’t routinely hyperventilate, only if necessary for “swollen” brain. Diuretics or Dexamethasone? Usually do give diuretics, particularly mannitol Usually don’t give dexamethasone or steroids Early decompressive craniectomy or temporal lobe decompression might be necessary in dire circumstances. Fluids. Avoid hypovolemia. Glucose. Treat hyperglycemia. Hypothermia was “hot,” but now it’s not. Avoid hyperthermia. IV and Inhaled Anesthetics Ruptured intracranial aneurysm or arteriovenous malformation (AVM) Prevent sudden increases or decreases in MAP that predispose the aneurysm to rupture Hyperventilation may depend on Hunt-Hess Grade: Grade 0 – hyperventilation O.K. Grades 1-2 – normocarbia or modest hypocarbia (paCO2 = 35) to prevent vasospasm Grades 3-5 – hyperventilation may be necessary anyway EEG monitoring if barbiturate coma is needed during temporary clipping. Moderate induced hypothermia? The results of the completed IHAST trial indicate no better outcome with hypothermia (33.5 oC) than normothermia (36.5 oC) Induced hypotension might be requested if aneurysm ruptures. Infratentorial (posterior fossa) surgery is unique in that it can be done in different positions – sitting, lateral decubitus, or prone. Thank you