Clinical Assessment of Pulsatile and Non
advertisement

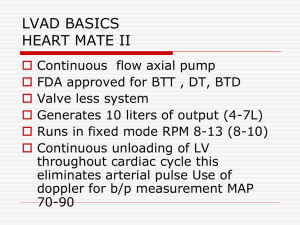
Clinical Assessment of Pulsatile and Non-Pulsaltile VADs Diana Joseph RN, BSN, CCTC VAD/Heart Transplant Coordinator OSF St. Francis Medical Center Peoria, IL Pulsatile Flow Contraction or beating of the heart as felt through the walls of the arteries Normal patients: Pulse is accurate VAD patients: Not truly feeling pts heartbeat. Asynchronous to electrical rhythm Types of VADs Pulsatile VADs Thoratec PVAD Thoratec IVAD HeartMate XVE Non-Pulsatile VADs HeatMate II HeartWare HVAD Pulsatile VADs Fixed or Auto mode Preload sensitive/Volume dependent Radial pulse felt is the actual VAD pumping rate VAD rate/flows increase with activity, volume, sepsis VAD rate/flows decrease with rest, hypovolemia, arrhythmias, RHF Blood Pressure Ideal BP <120/ If pt is hypotensive then ? Volume depleted Bleeding Arrhythmias ? RHF if LVAD Arrhythmias EKG-The only true way to identify pt’s true electrical rhythm VAD rate/pulse is asynchronous to pt’s electrical activity Atrial Fibrillation Ventricular Tachycardia Ventricular Fibrillation Majority of pts will have AICD/Defibrillators Cardioversion/Defibrillation Most VAD pts will tolerate arrhythmias Assess pt if hemodynamically stable Okay to cardiovert/defibrillate No CPR: Could possibly damage or dislodge cannulas/tubings resulting in fatal internal bleeding Hand Pump Non-Pulsatile VADs Axial/Continuous Flow RPMs Difficult to obtain a pulse or BP Use a doppler for BP (narrow pulse pressure) Ideal MAP >70 Most pts will have some residual rhythmic contraction thus create a pulse Arrhythmias EKG – Identify electrical rhythm Okay to cardiovert/defibrillate If RPMs too high could have “suction events” No Hand Pump Caution with CPR Basic Clinical Assessment Neuro-Mental Status Peripheral Circulation-warmth Skin color Respiratory status Labs if available ? VAD alarms Assess VAD Function VAD alarms VAD readings/parameters QUESTIONS ???