Initiation of DT LVAD Programs at Non
advertisement

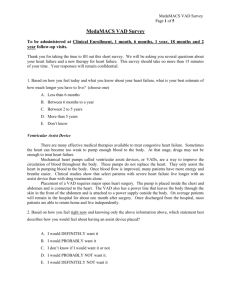
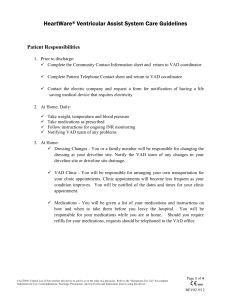
Rohinton J. Morris, MD Abington Health Systems Reasons Logistics Process Results Abington Hospital Reasons 600 bed capacity Cardiac surgery since 1996 – 3400 cases/year Two cardiac surgeons All cases done, except for transplant 17 & 8 member Cardiology groups 6 cardiac cath labs Heart Failure Service Community of the Elderly COMPETING FORCES 4 surrounding transplant centers 22 cardiac surgery centers in 20 mile radius Population of 8 million in surrounding Phila area Local population of 800K in primary service area LOCOREGIONAL NEEDS 15 miles from Philadelphia Why a VAD program? Primary Belief: Service of community – elderly, inadequacy of HF support Complementary HF services – to cath lab, EP service High-risk cardiac surgery Satellite to a transplant program HEART FAILURE Primary cause of death in the U.S. #1 DRG for admissions Advanced HF is its own specialty – board certification by ACC Demographics of US population leading to…greater prevalence of HF SURGICAL/CARDIOLOGY COLLABORATION Team approach to chronic disease Clinicians at front line-but everybody in hospital involved – administration, social work, ER, primary care, subspecialties. 1. Better appreciation of the natural history of heart failure will improve outcomes clinically Treatment options offered to local patients Utilization of resources efficiently Earlier recognition of advanced heart failure 134HTx centers • Heart failure, as a specialty, has lagged significantly behind other areas of cardiology in diffusing to the community – CABG – PCI – ICD -> Biventricular pacing -> afib ablations • Heart failure outcomes in the community are poor – 30 day readmission rates up to 25% – Average LOS nearly 7 days • • Heart failure, as a specialty, has lagged Hypothesis: significantly behind other areas of cardiology in diffusing to the community Poor penetration of advanced HF care – CABG Poor clinical outcomes – PCI – ICD are -> Biventricular pacing -> afibtoablations driven (largely) by failure identify Heart failure outcomes stage DinHFthe community are poor – 30 day readmission rates up to 25% – Average LOS nearly 7 days Logistics INFRASTRUCTURE Surgical, cardiologic focus Special people – VAD coordinator, HF social worker Involvement of multiple departments- Nutrition, Phys Ther, echo, ID, Psych, Administrative belief EMOTIONAL COMPONENTS Mission buy-in Culture of a village Nursing specialization Begin w End –goal : Implantation Work backwards – from Patient identification Identify team components Start with basic elements of team Pt identification #1 Committee formation Basic team members Simulation – FMEA process Identify personnel needed Identify equipment/space/peripherals What departments are involved? Who needs education? What are weak links? What are likely failure modes? FAILURE MODE CHANCE OF OCCURRENCE/EFFECT – SOLUTIONS?? VAD coordinator sick Device malfunction Slow timing of lab results Lack of blood products Multiple pt requirements Operative misadventure Caregiver stress Likely/ Moderate Unlikely/ Drastic Very likely / Serious Possible/ Serious Likely / Mild (Abstain)/ Serious Likely/ Moderate •Mock VAD Implant •Interdisciplinary team involvement •Debriefing after 1st LVAD implant – 1/24/2012 •Guided by Center for Patient Safety and Healthcare Quality •Maria Wilson & Nancy McMann VAD Surgeon(2010) VAD Coordinator(2011) Heart Failure Clinic Identify Candidates Joint Commission Destination Therapy Certification Continued Program Growth FMEA Establish Administrative & Clinical Committee 1st VAD Implant Heart Failure specialist to start Jan 2013 Process PRIMARY ESSENTIAL Cardiac Surgeon Heart Failure Cardiologist VAD coordinator Social Worker Heart Failure Nurses Financial manager Administrative support Echocardiographers Nutritionist Physical Therapist Rehab Outpatient Nursing Mechanical Cardiac Assist Program –Organizational Structure Laurence Merlis President & CEO Margaret McGoldrick Executive Vice President & COO Marni Guba Director, Cardiovascular Service Line Dr. John J. Kelly Chief of Staff Terry O’Reilly Senior Vice President, Patient Safety & CNO Theresa Reilly Director, Critical care Services Dr. Richard Eisenstaedt Chairman, Department of Medicine Dr. Robert Watson Chief of Cardiology Director, Comprehensive Heart Failure Program Dr. John Kukora Chairman, Department of Surgery To Be Named Co-Director, CHFP Medical Director, MCAP Dr. Rohinton Morris Chief, Cardiothoracic Surgery Medical Director, Cardiovascular Service Line MCA Program Kevin Hagan, VAD Coordinator Education VAD Inpatient VAD Outpatient VAD Committee •Cardiology •Cardiac Surgery •Anesthesia •Perfusion •OR Staff •Nursing •Social Work/Case Management •Physical/Occupational/Speech Therapy •Nutrition •Finance •Palliative Care Performance Improvement Research INTERMACS Chief, Cardiothoracic Surgery • Home care Chief of Cardiology • Rehab VAD Coordinator • Anesthesia HF Nurse Practitioner • CT Surgery Team – OR RNs, RNFAs, CT CT Surgeon NPs HF Cardiology Social Work –HF dedicated • Perfusion Financial Coordinator • Pharmacy Nutrition Physical/Occup/Speech Therapy • Echocardiography • Cardiovascular Service Line Director Palliative Care • Nursing Administration HFU, CICU Nursing Staff CNS (Clin Nurse Spec) Heart Failure• Hospital Senior Leadership Unit Critical Care Educator “We asked each segment to send at least one designated person to the FMEA process” Interdisciplinary team meetings Operations group meeting – includes administration Outpatient VAD Clinic Combined with Comprehensive Heart Failure Program Overlap with Aquapheresis Program Collaboration with multiple transplant centers Participate in INTERMACS Registry Majority of patients present via Comprehensive Heart Failure Program Major focus on PCP education & referral Self-referred Hospital units impacted: OR CSU HFU ETC - Cath Lab - Acute Rehab Unit Nursing competency Specialized nursing units: CSU, HFU Annual unit competencies New user training class Sim Lab – in development Physical & Occupational Therapy competency Specialized for VAD pt care Annual requirement Rehab unit competency Thoratec online training Transplant Center “SHARED CARE” New Paradigm of care Greater access of care for patients Multiple practice involvement Relief on implanting site for followup care Revenue sharing Volume issues / flows Minor perc site infection Gout Fracture in drive line casing local help from Thoratec engineer Acute pulmonary edema local ER Routine alarms Mild anemia Blood pressure Profound anemia GIB Drive line infection with sepsis VT + MV endocarditis ICD generator change Cataract surgery Hyperkalemia Results Program growth --Yearly growth --Total referrals : 131 --Following 43 patients --One-year mortality: 9.7% --Two VAD changeouts 2012 2013 2014 2015 2016 4 12 16 9… ??? IM-1 IM-2 IM-3 IM-4 IM-5 1 17 11 12 0 “Besides payment” The Mechanical Cardiac Assist Program created a Performance Improvement (PI) Plan to: Monitor the process and outcome of patient care Promote safe, quality and timely provision of care Improve the knowledge and skills of the MCAP team Provide the structure that supports performance improvement The MCAP PI plan is integrated with AMH’s organizationwide PI activities Patient selection –biggest driver of outcomes LOS –everybody contributes Readmission blues Medical issues Psychosocial issues Administration pitfalls Coding/Billing/Collecting Staffing Advanced Heart Failure specialist joined team Jan 2013 Community outreach Chairman’s Forum Primary Care Update Physician outreach / in-reach Internet promotion Large DT population in service area – Culture of the Elderly September 2011 – Present (Apr 2015): VAD/Tx Evals: 129 Recommended VAD/Tx: 47 VAD Implants: 46 (41 @ AMH) TxListed/Potentially Listed (But not VADed): 5 JACC (Jun 2011) – Showed outcomes were no different in 55 pts that were BTT or DT (split by age 70) at a 386 bed community hospital Lead author Robert Adamson –Medical director of cardiac transplantation program at Sharp Memorial Hosp, S.D. Ann Thor Surg – (John, Oct 2011)- PMA study. Compared outcomes of 486 pts @ 36 centers during clinical trial, to 1496 pts @ 83 centers posttrial. KaplanMeier survival increased (76 to 85%) in 2nd group. Presented at AATS-First discussant: “That new VAD technology that utilizes continuous flow. . .can be taught along with appropriate patient selection and disseminated to a broad range of clinical centers.” M. Acker –Chief of Cardiac Surgery -UPenn DT is no longer the “future”—It’s here. More DT/advHF programs are needed for the community. A team approach—including hospital administration & staff– is necessary. Careful construction, continuous monitoring and PASSION give great outcomes. Questions?