Emergency Preparedness and Management for
advertisement

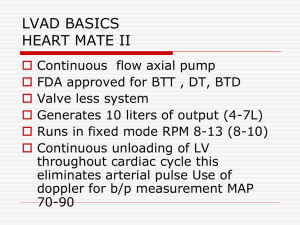
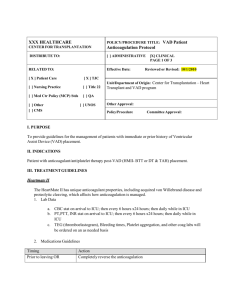
Emergency Preparedness and Management for Patients with Ventricular Assist Devices Emergency preparedness applies to everyone and even more so to patients with a ventricular assist device (VAD) that requires constant power. Your community can be impacted by several types of hazards and you may also travel to a location with different hazards other than those at home. Knowing what to do can make all the difference. It is recommended that you prepare a plan for you and your family. Hospitals, fire stations and police stations have back-up generators for times of loss in power. Contact your local emergency facilities to discuss their commitment to allowing you to seek shelter with them. Include the contact and location in your preparedness plan. In an event of prolonged power outage, your VAD team may give you specific instructions on where to go. Your options may vary depending on how widespread the power outage: 1) Relocate to family or friends home that has power 2) Relocate to your local emergency facility or community shelter that has a back-up generator 3) Go to the hospital If you have access to a portable generator, you may use it to power your battery charger. You may not use it to power your pump directly with your AC adapter. In case of a medical emergency, it is safe for you to be transported by ground or air to your VAD hospital or nearest hospital. If evacuation is necessary, or if you are leaving your home for an extended period of time, take your VAD equipment and supplies with you: Batteries (always charge batteries after use so you have spare, fully charged batteries) AC & DC adapter Spare controller Battery charger Driveline exit site dressing supplies VAD binder (patient manual, and other instructions provided by your VAD team) Emergency contact numbers Prescribed medications Store and operate all equipment within the recommended temperature conditions. Keep an emergency kit available at all times. In the event of a disaster, it is recommended you have enough food and water to last 72 hours. Other items to include in an emergency kit are: Flashlight Cell phone and charger Emergency contact numbers Water Page 1 of 2 GL1110 Rev01 11/14 Emergency Preparedness and Management for Patients with Ventricular Assist Devices Keep emergency contact numbers at different locations in your home (e.g. by the phone, in your binder/bag, on your refrigerator, at your bedside). You may want to program contact person(s) in your phone as “in case of emergency” for easy location. It is also a good idea to keep your medical history and medication list in your VAD binder or bag. Make a plan for how you will communicate with your family and VAD team. You may want to subscribe to an alert system. In addition, you may find many resources in emergency planning at your local community services. EMERGENCY Contact Information If a situation arises that you are experiencing an urgent alarm or are in an emergency situation call 911. There is a VAD coordinator on-call 24 hours a day/7 days a week if an emergency situation arises. You can contact a VAD coordinator by calling _________________________ In the event of an extended power outage and/or no clean water supply, the closest community facilities with back-up resources are (fill in location and contact person): Hospital/Emergency Room: ________________________________________ Fire Station: ____________________________________________________ Police Station: ____________________________________________________ NON-EMERGENCY Contact Information If a non-emergency situation arises and you need to speak to the VAD Coordinator, call _________________ during business hours. Page 2 of 2 GL1110 Rev01 11/14