Does monitoring cardiac output improve outcome?
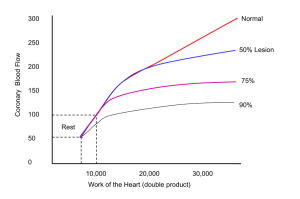
advertisement

Does monitoring cardiac output influence outcome? David Bennett St George’s Hospital London Disclosures • I act as a consultant for Deltex and Lidco Questions to be posed • Can cardiac output (CO) be accurately assessed clinically? • Why are there so many different technologies for measuring CO? • Does monitoring CO, particularly with PAC increase morbidity and/or mortality? • Does monitoring CO or surrogate have prognostic value? • Does targeting CO improve outcome? How Accurate Is Clinical Assessment of Cardiac Output in the Early Postoperative Period Following Cardiac Surgery? Robert A. Linton, MD, FRCA; Nick W. Linton, MEng; Fiona Kelly, MBBChir The Rayne Institute, St Thomas' Hospital, London, United Kingdom • Can cardiac output (CO) be accurately assessed clinically? PhysiciansÕEstimates of Cardiac Index and Intravascular Volume. Ireguri MG Am J Crit Care 2003;12:336. 45 40 35 30 25 % 20 15 10 5 0 60 50 40 % 30 20 10 0 Over Correct Under estimate estimate Cardiac Index Over Correct Under estimate estimate Volume Status Why are there so many different technologies for measuring CO? Fick: Direct, Indirect Dilution tehniques: ICG, Hot and cold, intermittent and semi-continuous ScvO2 and SvO2 ECHO Oesophageal, Supra-sternal Doppler Impedance cardiography Pulse contour analysis C02 rebreathing Does monitoring CO, particularly with PAC increase morbidity and/or mortality? Conners AF,Jr, Speroff T, Dawson NV, Thomas C, et al: The effectiveness of right heart catheterizaion in the initial care of critically ill patients. JAMA 1996; 276: 89997 The incidence of major morbidity in critically ill patients managed with pulmonary artery catheters: A meta-analysis Ivanov, Rada MD; Allen, Jill MSc; Calvin, James E. MD, FACC, FRCPC CC 28(3), March 2000, pp 615-619 M Impact of the Pulmonary Artery Catheter in Critically Ill Patients Meta-analysis of Randomized Clinical Trials Monica R. Shah, MD, MHS, MSJ; Vic Hasselblad, PhD; Lynne W. Stevenson, MD; Cynthia Binanay, RN, BSN; Christopher M. O’Connor, MD MD, MPH; Robert M. Califf, MD JAMA. 2005;294:1664-1670. Impact of the Pulmonary Artery Catheter in Critically Ill Patients Meta-analysis of Randomized Clinical Trials Monica R. Shah, MD, MHS, MSJ; Vic Hasselblad, PhD; Lynne W. Stevenson, MD; Cynthia Binanay, RN, BSN; Christopher M. O’Connor, MD; George Sopko, MD, MPH; Robert M. Califf, MD JAMA. 2005;294:1664-1670. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K; PAC-Man study collaboration. : Lancet. 2005 Aug 6-12;366(9484):472-7. P(survival) 1.00 0.75 0.50 No PAC PAC 0.25 No PAC PAC 508 506 240 232 0 15 205 191 194 179 188 174 186 168 183 166 30 45 60 Time from randomisation (days) 75 90 0.00 Does monitoring CO or a surrogate have prognostic value? Effect of Oxygen Delivery on Mortality Does monitoring CO or a surrogate have prognostic value? and Morbidity in High Risk Surgery. Shoemaker Chest. 1988: 94; 1176 70 60 50 40 % % Mortality 30 20 10 0 301-400 401-500 60 >501 50 % of Patients <300 40 30 % Patients with Morbidity 20 10 0 <400 400-500 500-600 >600 Does monitoring CO or surrogate have prognostic value? Oxygen consumption L/min/m 2 Responders 350 300 250 200 150 Before dobutamine After dobutamine 100 50 Non Responders 0 0 200 400 600 800 1000 1200 1400 Oxygen delivery L/min/m2 Rhodes A. CCM 1999; 11; 2361 250 200 150 100 50 0 0 200 400 600 800 1000 1200 Outcome of Patients cc Responders Non Responders Predicted Mortality % 39 58 Actual mortality % 14 90.9 Rhodes A. CCM 1999; 11; 2361 Impact of LOW Post-Operative Central Venous Oxygen Saturation on Morbidity & Mortality in Surgical Patients V PRIYA*, J V DIVATIA, RASHMI S, R SAREEN 80 Normal (n = 32) Low (n = 51) ScvO2 at 2 hrs 76.8 + 5.7 p = 0.00* 70 63.9 + 8.9 60 80 ScvO2 at 12 hrs p = 0.00* ScvO2 at 12 hours : 95% CI ScvO2 at 2 hours : 95% CI 90 78 76 Normal (n = 32) Low (n = 51) 76.2 + 4.1 74 72 70 68 66 68.7 + 6.1 OUTCOME Normal (n=32) Low (n=51) p Value Days on ventilator (Mean+SD) 0.59 + 1.5 3.5 + 6.1 0.009* Anastomotic leak (no. of pts) 2 (9%) 13 (26%) 0.03* ICU stay (days, Mean+SD) 1.7 + 2.5 5.6 + 6.7 0.009* Hospital stay (days, Mean+SD) 13.5 + 5.0 17.8 + 10.5 0.002* ICU mortality (no. of patients) 0 (0%) 3 (6%) 0.16 Hospital mortality (no. of pts) 0 (0%) 3 (6%) 0.16 DO2 does not always correlate with CO Relationship Between Central Venous Oxygen Saturation and Oxygen Delivery. x e d n I 1200 y r e v i l e D 1100 n e g y x O 600 1000 900 800 DO2 I ml/min/m7002 500 400 300 200 100 0 20 30 40 50 60 70 Central Venous Saturation 80 90 100 • Does targeting CO improve outcome? Meta-analysis of hemodynamic optimization: relationship to methodological quality Martijn Poeze, Jan Willem M Greve and Graham Ramsay Critical Care 2005, 9:10.1186/cc3902) This article is online at: http://ccforum.com/content/9/6/R771 R771-R779 (DOI Peri-operative Cont Treatm ro ent l % Mortalit 10.4 y 4.7 Wilson et al:- BMJ :1999 318 1099 * Days Meta-analysis of hemodynamic optimization: relationship to methodological quality Martijn Poeze, Jan Willem M Greve and Graham Ramsay Critical Care 2005, 9:10.1186/cc3902) This article is online at: http://ccforum.com/content/9/6/R771 R771-R779 (DOI Sepsis % Mortalit y Cont Treatm ro ent l 54 53 Hayes, M A. Timmins, A C. Yau, E H. Palazzo, M. Hinds, C J. Watson, D. Title Elevation of systemic oxygen delivery in the treatment of critically ill patients Source New England Journal of Medicine. 330(24):1717-22, 1994 Jun 16. % Mortality Early goal-directed therapy in the treatment of sepsis and septic shock: An outcome evaluation of early intervention Rivers et al N Eng J Med 2001 345 19 * * * ScvO2% Hours * * Early goal-directed therapy in the treatment of sepsis and septic shock: An outcome evaluation of early intervention Rivers et al N Eng J Med 2001 345 19 Control n (%) Treatment n (%) p 59 (46.5) 38 (30.5) 0.009 Severe sepsis 19 (30) 9 (14.9) 0.06 Septic shock 40 (56.8) 29 (42.3) 0.04 44 (45.4) 35 (35.1) 0.01 Mortality In-hospital: All patients Septic syndrome DO2I ml/min/m 2 Early goal -directed therapy after major surgery reduces complications and duration of hospital stay Pearse et al Critical Care 2005 9 R687 -693 * * * Hours * * * * Number of infections * * * Control n=60 EGDT n=62 14 11 Median (6-188) (0.4-110) % Difference Reduction 3 21 Mean 29.5 17.5 12.0 41 Total 1770 1085 685 39 Chittock DR. Dhingra VK. Ronco JJ. Russell JA. Forrest DM. Tweeddale M. Fenwick JC. Severity of illness and risk of death associated with pulmonary artery catheter use.[see comment]. Critical Care Medicine. 32(4):911-5, 2004 Apr. Does goal directed therapy using the oesophageal Doppler reduce surgical mortality and morbidity? Hamilton M. A.1, Grocott M. P. W.1, Mythen M1, Bennett D2 Mean reduction in LOS of 4 days (25%) Conclusions •Cardiac output is a frequently measured variable •There are several technologies allowing it’s measurement •Despite earlier claims it is unlikely that measuring CO particularly with the PAC is harmful •Low CO and it’s failure to respond to treatment has prognostic significance •There is now reasonable evidence suggesting that targeting CO very early in the course of critical illness is of real benefit •This is particularly so in patients undergoing major surgery META-ANAYSIS OF HEMDYNAMIC OPTIMIZATION IN HIGH RISK PATIENTS Jack W. Kern1,2,3, Pharm D, William C Shoemaker2,3, MD CCM 2001 Patient identification. Written informed consent. Lines inserted. Surgery. Randomisation Admit to ICU. Monitor cardiac output in all patients using Lidco. Data concealed from clinical staff In all patients maintain SaO2 ≥94%, Hb≥ 8g.dl-1 , Temp.at 37oC. HR≤100 or <20% above baseline. MAP 60-100 mmHg CONTROL GROUP EGDT GROUP Fluid challenge with 250 ml bolus IV colloid until sustained 2mm Hg rise in CVP is achieved for ≥20 min. Repeat if CVP falls Fluid challenge with 250 ml bolus IV colloid until sustained 10% rise in SV for ≥20 min. Repeat if SV falls kg -1 If urine output <0.5ml hr-1 for 2 hours or consecutive hourly lactate rises to >2 mmol l -1 then CI revealed to clinical staff If DO2 <600ml min -1 m2 start dopexamine at 0.25µg kg -1 min -1 and increase to maximum of 0.25µg kg -1 min -1 until DO2 reaches target value. Dose reduced if tachycardia or myocardial ischemia develops If CI <2.5l min-1m2 commence epinephrine, if > 2.5l min-1m2 continue current treatment After 8 hours study period ends all decisions taken by clinical staff. Patient followed for hospital morbidity and 60 day mortality Pinsky MR, Vincent JL. Crit Care Med. 2005 May;33(5):1119-22. META-ANAYSIS OF HEMDYNAMIC OPTIMIZATION IN HIGH RISK PATIENTS Jack W. Kern1,2,3, Pharm D, William C Shoemaker2,3, MD CCM 2001 1: Crit Care Med. 2006 Apr 4; [Epub ahead of print] Related Articles, Links Pulmonary artery catheter use is associated with reduced mortality in severely injured patients: A National Trauma Data Bank analysis of 53,312 patients* Friese RS, Shafi S, Gentilello LM. •Audit of >53,000 trauma patients in USA •Older patients with severe injury and shock had a survival benefit when managed with PAC • Odds ratio, 0.33; 95% confidence interval, (ratio 0.17-0.62) •