Heart Failure
advertisement

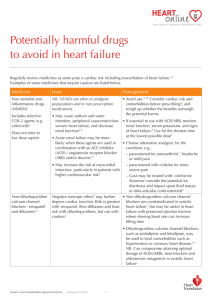
HEART FAILURE: Putting It All Together South Carolina Association Clinical Documentation Specialists Spring Meeting March 23, 2012 Joan M. Lacey, ACNP, ANP, AACC Carolina Cardiology Greenville, SC Heart failure is a common clinical syndrome resulting from any structural or functional cardiac disorder that impairs the ventricles ability to fill and eject blood and the bodies neurohormonal adaptation to this process What Exactly is Heart Failure? A syndrome with many causes and manifestations! Pump failure and altered hemodynamics Altered cell biochemistry (Ca++ cycling) A Perfusion disorder: revascularization and mechanical assistance A rhythm disorder An endocrinopathy, neuropathy, and vasoregulatory dysfunction Abnormal proliferative signaling and gene expression Irreversible premature cell death Less than 50% 5-year survival in symptomatic HF cannot be excluded from the definition of HF Cardiomyopathy “HEART MUSCLE DISEASE” EF <40-45% Primary-in the heart Genetic/mixed/acquired Secondary-occurs from other organ dysfunction Prevalence of Congestive Heart Failure An estimated 5.8 million Americans have congestive heart failure (CHF). (Source: excerpt from NHLBI, Congestive Heart Failure Data Fact Sheet: NHLBI) Survival at 5 yrs. 50% Mortality Estimates of mortality rate per year for patient subgroups Class II = 5-15% Class III = 20-50% Class IV = 30-70% http://www.heartfailure.org/eng_site/faq.asp #longlife Hospitalizations and Mortality Number one reason for admission High readmission rate 27% within one month 50% within six months 17% two or more admissions 1 in 5 people die within one year of diagnosis Systolic dysfunction: poorer prognosis 50% die within five years (median survival) Over 1 million hospitalizations per year Leading cause of Medicare admissions Heart Failure: The Epidemic Prevalence 5.8 million (US) 25 million (worldwide) Incidence 670,000/ year. ETIOLOGY CAD 65% IDIOPATHIC DILATED 50% TOXIN-INDUCED ALCOHOL,COCAINE,CHEMOTHERAPUTIC DRUGS,RADIATION INFECTIOUS /INFLAMMATORY COXSACKIE B, LYME DISEASE, HIV,HCV,CHAES,LUPUS,RA,GIANT CELL MYOCARDITIS, INFLUENZA,MYCOPLASMA PNA FAMILIAL DILATED CARDIOMYOPATHY 20-30% OF “IDIOPATHIC “DCM, ARVD,MUSCULAR DYSTROPHIES,HYPERTROPHIC CM, HEREDITARY HEMOCHROMATOSIS ETIOLOGY PERIPARTUM: IN THE LAST MONTH OR FIRST 5 MONTHS POSTPARTUM ( IMMUNE VS. OCCULT LV DYSFUNCTION) STRESS-INDUCED: “TAKO-TSUBO” ENDOCRINE/NUTRITIONAL:DM,OBESITY,THYROID,ACROMEG ALY AND GH DEFICIENCY,PHEO IRON OVERLOAD: HEREDITARY HEMOCHROMATOSIS TACHYCARDIA INDUCED HYPERTENSIVE INFILTRATIVE: (RESTRICTIVE) AMYLOID,SARCOID New York Heart Association (NYHA) Class Patient Symptoms Class I (Mild) No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath). Class II (Mild) Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. Class III (Moderate) Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. Class IV (Severe) Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased. Types of Heart Failure Acute Chronic Systolic Diastolic Mixed TYPES OF HEART FAILURE FUNCTION Systolic: Decreased EF: ½ the cases HF *Mild 45-50% *Moderate 35-40% *Severe <35% Diastolic: HFnEF (heart failure normal EF) ½ the cases HF DIASTOLIC Older, female, HTN, less CAD LVEDP >16, EF > 50% Echo Impaired relaxation=grade 1 Pseudo normalization=grade 2 Reversible Restrictive=grade 3 Irreversible Restrictive=grade 4 Types Location Left side: ischemic/valvular Right side: CorPulmonale, usually caused by LHF as pressure backs up into lungs. PHTN/PEs/chronic lung disease History CAD/angina HTN OSA/OHV Alcohol/drugs/chemo Viral illness Trips Pregnancy problems Goals of Treatment 1) Prevent functional decline 2) Prevent complications 3) Prevent hospitalizations 4) Prevent progression of HF Medications *BB-selective/nonselective 35-65%RRR *ACE 20% mortality reduction/ARB *Diuretic-thiazide/loop/aqua *Nitrates /AA Hydralazine+ Nitrates *Morphine/anxiolytic *Digoxin-0.5-0.8 ng/mL in low EF *Aldosterone inhibitors (class II/III) *CCB avoid non-dihydropyridines/CS Labs CBC/BMP/Na/LFT BNP good neg. predictive value Albumin/Pre-Albumin Renal failure may be reason for or cause by HF Survival over time in patients with severe chronic heart failure (HF) and a left ventricular ejection fraction less than 30 percent who, at study entry, had either a normal plasma sodium concentration (greater than 137 meq/L, solid line) or hyponatremia (plasma sodium less than or equal to 137 meq/L, dashed line). Survival was significantly reduced in the patients with hyponatremia. The survival rate was very low (approximately 15 percent at 12 months) in those with a baseline plasma sodium concentration less than or equal to 130 meq/L. Data from: Lee, WH, Packer, M, Circulation 1986; 73:257. Tests Echo- poor quality, thin/obese EKG Stress test-function, new HF Coronary angiography MRI-CAD,MI,HCM,ARVC,Amyloid CT SPECT (single photon emission computed tomography) IMAGING IN HF Echocardiography Nuclear cardiology Cardiac CT and Cardiac MRI Very high resolution Very good tissue characterization Very good quantitative analysis Viability assessment Functional assessment, including valve function Cardiac MRI Benefits *High quality measurement of LV volume. *Comprehensive evaluation of virtually every aspect of cardiac anatomy and function. *Viability Disadvantage ICD/PPM-relative contraindication Claustrophobia Motion HR <60 Society for Cardiac Magnetic Resonance http://www.scmr.org/ Exercise and Functional Capacity in Heart Failure HF-ACTION trial HF-ACTION Primary Hypothesis Patients with LV systolic dysfunction and NYHA class II-IV symptoms who undergo exercise training in addition to usual care will have a 20% lower rate of all-cause death or hospitalization(primary endpoint) over two years than patients who receive usual care alone Whellan DJ, O’Commor CM, LeeKL et al. Am Heart J 2007; 153:201-2-11 Percent of Patients with Clinical Improvement Exercise training Usual care 3M 54% 28% 12M 53% 33% Conclusion HF-ACTION Based on the main analysis adjusted for HF etiology, exercise training produced a modest, non-significant decrease in the primary endpoint (all-cause mortality or allcause hospitalization) and key secondary clinical endpoints. In protocol-specified analyses adjusted for prognostic factors, the treatment effect was statistically significant for the primary endpoint and for the secondary endpoint of CV mortality or HF hospitalization. Peak VO2 Most objective assessment of functional capacity in HF pt. Only of value in pt. whose exercise capacity is limited by HF. Influenced by age, gender, BMI. The percent predicted value may be a more reliable indicator of prognosis. VO2 max has been defined as: "the highest rate of oxygen consumption attainable during maximal or exhaustive exercise" Cumulative survival in patients with heart failure according to maximal oxygen consumption (VO2) in mL/kg per min. Survival is markedly reduced in patients with a peak VO2 below 10 mL/kg per min. Data from: Mancini, DM, Eisen, H, Kussmaul, W, et al, Circulation 1991; 83:778. Six-min. walk test correlates with VO2 max. Measures the distance ambulated on a level hallway surface during six minutes. In a retrospective analysis of 440 patients from a randomized controlled trial with NYHA class III-IV HF baseline distance significantly predicted mortality and hospitalization; for each 100 m (328 ft) increase in distance walked. Similarly, in a series of 476 patients form a single referral center, the distance walked at baseline was an independent predictor of two-year survival. See 2002 Thoracic Society statement. Hemofilteration UNLOAD (UltrafiltratioN versus IV Diuretics for Patients Hospitalized for Acute Decompensated Congestive Heart Failure; J Am Coll Cardiol, 2007; 49:675) 200 patients, 28 medical sites, randomization to UF or diuretics At 48 hours into treatment, the UF group: 38 percent greater weight loss 28 percent greater net fluid loss At 90 days following hospital discharge, the UF group: 43 percent reduction in rehospitalizations for HF 52 percent reduction in ED or clinic visits 63 percent total reduction in days rehospitalized The benefits seen in all subgroups analyzed Today's Devices Impella GHS – first to use in SC 2.5 or 5.0L/min Directly unload the left ventricle in the heart Reduce myocardial workload and oxygen consumption Increase cardiac output and coronary and end-organ perfusion ICD Indications EF<35% Nonischemic vs. Ischemic Asymptomatic NSVT SCA,VF or unstable VT NYHA class I-III Optimum OPT BiV-ICD Indications *EF < 35% *NYHA Class I ischemic or *NYHA Class II ischemic or nonischemic HF *Stable OPT *LBBB/QRS > 120ms Indications for Transplant *Refractory cardiogenic shock *Dependence on inotropes *Peak VO2 <10ml/kg/min *Severe ischemia and poor function not amendable to CABG/PCI *Recurrent symptomatic vent. *Arrhythmias refractory to Rx. Jarvik HeartMate HeartWare international HVAD pump Today’s surgical options Revascularization RF Ablation for Arrhythmia Aneurysm Resection Dor Batista VAD Valve surgery Transplant Cor Pulmonale What the heck is this COR=CORONARY PULMONALE=PULMONARY Right ventricular hypertrophy and or dilatation from pulmonary hypertension which results from any disease of the lung parenchyma, thorax or pulmonary vasculature unrelated to the left side of the heart. RIGHT VENTRICLE SIZE: RVEDD/RVESD (RV end diastolic/systolic diameter) Normal: 0.9-2.0cm;1.5-2-2cm RIGHT ATRIAL SIZE: Normal: 2.8-4.0cm RV HYPERTROPHY RV FAILURE = LATE COR PULMONALE PREDISPOSING FACTORS COPD-80% CHRONIC BRONCHITIS/BRONCHIECTASIS OSA CHRONIC PE/ACUTE PE CYSTIC FIBROSIS DIFFUSE INTERSTITIAL LUNG DISEASE PNEUMONITIS PRIMARY PHTN MARKED OBESITY ALTITUDE SICKNESS ANY THING THAT CAUSES PHTN SYMPTOMS CHEST DISCOMFORT/ANGINA EXERCISE INTOL./FATIGUE DOE EDEMA ASCITES WHEEZE/COUGH SYNCOPE SOMNOULENCE TREATMENT TREAT UNDERLYING CAUSE OF THE PULMONARY HYPERTENSION GOAL TO DECREASE PULMONARY VASCULAR RESISTANCE OXYGEN IMPROVES SURVIVAL OF HYPOXIC PATIENTS WITH COPD CAREFUL DIURETICS COULD DROP CARDIAC OUTPUT (WATCH BUN/CR) EXAM-RIGHT HEART/ PERIPHERAL SPLIT S2 TR SYSTOLIC MURMER JVD HEPATOMEGALY/HJR PERISTERNAL HEAVE AT 2ND LICS PERIPHERAL EDEMA TESTS: CXR: TEAR DROP HEART/PULM ART. ENLARGED ECHO PFT/VQ RHCATH BNP CT EKG: RAD/RVH/RAH- “P” PULMONALE II,III,AVF,V1-V2 S1,Q3,T3,TALL R IN V1-V2, PROMINENT S IN V5-V6 INVERTED TWAVES AND ST DEPRESSION IN V1-3=RVSTRAIN Cardiomyopathy Disease of the heart muscle best suited to refer to genetic diseases. *HCM *DCM *Restrictive CM *Arrhythmogenic RV Cardiomyopathy *Left vent non compaction *Unclassified Critical thinking is the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action. http://www.criticalthinking.org/aboutCT/define_critical_thinking.cfm Exam- Objective JVD/HJR Edema-pulm/crackles/peripheral/scrotal Ascites, effusions Gallop S3, S4 Murmur (http://www.blaufuss.org) Arrhythmias Displaced apical pulse Diaphoresis Pulse press <25mmHG Pulses Alternans Peripheral constriction Inc. sympathetic tone, tachy Daily thoughts at Bedside Perform routinely!! Medication-right the first time Read progress notes Telemetry V-scan (visual) Exam-objective/subjective I &O/Wt. Lifestyle/eating/activity/family Heart Sounds S1-TV/MV closed=TV/MV regurg.----PV/AV stenosis S2-PV/AV closed=PV/AV regurg.----TV/MV stenosis A stenosed valve is open and a regurgitant valve is closed Exam-Subjective Dyspnea/SOB/DOE PND/Orthopnea Fatigue/exercise intolerance Weight/abdominal girth