Biliary system
advertisement

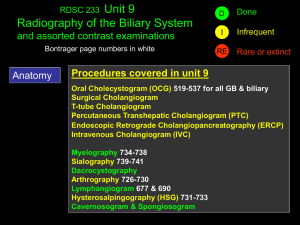
Biliary system Anatomy Plain x ray GB stone in 10 % Gas in biliary tree Gall stone ileus Gas in GB wall Porcilin GB Radiological investigations Oral Cholecystography We comment on Site Size Shape Filling Defect Function Concentration contractility of dye Investigations Imaging techniques Ultrasound this is most useful Most important to show intrahepatic bile ducts dilatation Measure the diameter of CBD (normal up to 7 mm) Comment on the status of the GB and its stones Visualize CBD diameter, stones or areas of narrowing Tumors in the region of the pancreas is seen CT (conventional or helical) competes with the U/S especially as regards the pancreatic tumors. Radiological investigations Ultrasound cholangiogram Preoperative cholangiogram IV cholangiogram PTC ERCP Intra operative T tube ( post operative ) Investigations for a case of obstructive jaundice ERCP ERCP is an outpatient procedure that combines endoscopic and radiologic modalities to visualize both the biliary and pancreatic duct systems. Endoscopically, the ampulla of Vater is identified and cannulated. A contrast agent is injected into these ducts, and x-ray images are taken to evaluate their caliber, length, and course. ERCP is used to get a final diagnosis and do biopsy of ampullary tumors, or brush cytology. Investigations for a case of obstructive jaundice ERCP It can be also therapeutic for stone extraction by Dormia basket or insertion of a stent, both are preceded by sphincterotomy. It has its risks ascending infections, perforations, pancreatitis, an bleeding due to sphincterotomy done routinely before CBD cannulation ERCP Congenital caroli’s syndrome Chledochal cyst (type I) Investigations for a case of obstructive jaundice MRCP a sensitive noninvasive method of detecting biliary and pancreatic duct stones, strictures, or dilatations within the biliary system. It is also sensitive for helping detect cancer. Investigations for a case of obstructive jaundice MRCP (contraindications) Absolute include the presence of a cardiac pacemaker, cerebral aneurysm clips, ocular or cochlear implants ocular foreign bodies. Relative contraindications include the presence of cardiac prosthetic valves, neurostimulators, metal prostheses, penile implants Investigations for a case of obstructive jaundice PTC performed by a radiologist using fluoroscopic guidance. The liver is punctured to enter the peripheral intrahepatic bile duct system. An iodine-based contrast medium is injected into the biliary system and flows through the ducts. Obstruction can be identified on the fluoroscopic monitor. Investigations for a case of obstructive jaundice PTC It is especially useful for lesions proximal to the common hepatic duct. Still, PTC ERCP is generally preferred. is reserved for use if ERCP fails or when altered anatomy precludes accessing the ampulla. Investigations for a case of obstructive jaundice PTC Complications of this procedure include the possibility of allergic reaction to the contrast medium. peritonitis. intraperitoneal hemorrhage, sepsis cholangitis. subphrenic abscess. lung collapse. Severe complications occur in 3% of cases PTC Investigations for a case of obstructive jaundice Endoscopic ultrasound (EUS) combines endoscopy and US to provide remarkably detailed images of the pancreas and biliary tree. It uses higher-frequency ultrasonic waves compared to traditional US (3.5 MHz vs 20 MHz) allows diagnostic tissue sampling via EUSguided fine-needle aspiration (EUS-FNA). Acute Cholecystitis Acute obstructive (Calcular) Acute Acalcaus Acute emphysematous Acute obstructive (Calcular) (Pathology) Calcular obstruction GB become hyperemic, oedematous & distended Chemical inflammation Release of Phosphlipases Act on lecithin which is a mucosal protector transforming it into Lysolecithin (mucosal toxin Arachidonic acid (PG precursor) (inflammation) Sepsis Ecoli, klebsilla & strept which occur later on Acute obstructive (Calcular) (Pathology) Following acute inflammation the condition end by one of the following Resolution Mucocele Empyema Gangrene And perforation Bilo-enteric fistula Acute Acalcular Cholecystitis It form 8 % Risk factors are Sepsis Starvation Prolonged TPN Ileus Morphine use > 6 days Acute Acalcular Cholecystitis Pathology is not knowen Prolonged distention of GB , Bile stasis & inspissations lead to mucosal injury and vessel thrombosis Hypersensitivity to concomitant antibiotics Gangrene occur in 25 % of cases Acute emphysematous GB Caused by mixed poly-microbial infection including gas forming bacteria 70% male , diabetics Thrombosis of cystic artery is the cause It lead tom Gangrene in 75 % Perforation in 15 % Patient 5 F General Clinical picture High fever with shivering Nausea, vomiting & biliary dyspepsia Local Biliary colic Tenderness Murphy’s sign Boa’s sign Complication Clinical picture The attack of biliary colic is the start with visceral type of pain (diffuse, colicky, radiating, and associated with vomiting) Later on after 6 to 8 hours, the pain localizes to the right hypochondrium, and become associated with tenderness, rebound T, and rigidity and mild fever (somatic pain) The presence of distended gall bladder is the hallmark of the disease, either discovered clinically or by U/S In 25% of cases the bilirubin rises, due to compression of the CBD (Mirrizi syndrome) or less commonly due to an associated stone CBD Serum amylase should be a routine as well as plain X ray abdomen (pancreatitis, and perforation or gas in biliary system Acute calculous cholecystitis Obstruction of GB outlet leads to chemical inflammation, which persists for 72 h then a fate of the following, will occur Resolution (most common), with relief of obstruction ~>scarring and non-function of GB Resolution of the inflammatory process with persistence of the obstruction (mucocele of the GB) Persistence of infection (empyema of the gall bladder) with obstruction persistence Gangrene and acute perforation leading to localized pericholecystic abscess or generalized frank biliary peritonitis Chronic perforation with development of biliary eneteric fistula Investigation Laboratory Leucocytosis Liver function S. amylase Radiological Plain xray US Doppler US HIDDA scan CT scan & MRI Investigations: the best is ultrasound An ultrasound is the most common screening test. It is 90-95% sensitive for cholecystitis It is 78-80% specific. For simple cholelithiasis, it is 98% sensitive and specific. Investigations: the best is ultrasound Findings include gallstones or sludge and one or more of the following conditions: Gallbladder wall thickening (>2-4 mm) Gallbladder distention (diameter >4 cm, length >10 cm) Pericholecystic fluid from perforation or exudate Air in the gallbladder wall (indicating gangrenous cholecystitis) Sonographic Murphy sign (86-92% sensitive, 35% specific), pain when the probe is pushed directly on the gallbladder (not related to breathing) Treatment (conservative) NPO, nasogastric & IV fluids Analgesic, antipyretic & spasmolytic Antibilotic Broad spectrum ( cephalosporins ) Metronidazole & aminoglycoside Follow up and surgery In the same admission Interval cholecystectomy Urgent if Treatment (surgical) Doubt in diagnosis Failure to improve Complication We perform Chole-cyst-ectomy retrograde Chole-cyst-ectomy Chole-cyst-ostomy Subtotal Chole-cyst-ectomy Mini Chole-cyst-ectomy Laparscopic Chole-cyst-ectomy Treatment (surgical) Established Non-progressive disease Interval Chole-cyst-ectomy Early chole-cyst-ectomy Gall stones Increase bile pigments Decrease phosphlipid &bile salts Increase cholesterol Metabolic Gall stones Infection Stasis 75% Cholesterol stone of stones formed in sterile GB (10% infection) Protein matrix cholesterol (70%) bile pigment Ca carbonate Ca palmitate (Ca salts deposited at periphery, their amount determine the radiolucency) Cholesterol stone Two types Pure cholesterol Oval or rounded mamillated or mullbery-surfaced pale yellow in color solitary big size (100% cholesterol rounded) 60% cholesterol (mixed) Multiple mediums sized (60% cholesterol, faceted) brownish polished surface Gall stones Formation involves 7 processes 1. 2. 3. 4. 5. 6. 7. Super saturation with cholesterol Incomplete transfer of cholesterol from vesicles to micelles Formation of vesicles with high cholesterol Aggregation and fusion of unstable vesicles Cholesterol crystallization (mucin is a nucleating agent) Biliary sludge formation (mucin+ cholesterol+ Ca+pigment ~precursor of stones) Stone growth Black Pigment Stone 25% of stones. It is common in cirrhotics, after terminal ileum resection and in hemolytic diseases. Formed in a sterile GB (20% infection rate) Composed of bilirubin polymer without Ca palmitate and +cholesterol (25%)+matrix of organic material Usually multiple, small, irregular, dark green or black in color Hard in consistency and cut surface is layered Formation Elevated concentration of mono-conjugated bilirubin lower bile salt concentration is the usual constitution in forming patients yet the exact pathogenesis is not known Brown Pigment Stone Rare ductal stones caused by infection by gram -ve bacteria releasing B glucuronidase releasing free bilirubin Composed mainly of Ca bilirubinate, Ca palmitate + small amounts of cholesterol matrix of organic material Amorphous soft stones Gall stone disease Symptom less no interference interference in Diabetics Acromegalic Calcified Patient under go surgical intervention Symptomatic Chronic cholecystitis Acute biliary colic, acute cholecystitis Jaundice Clinical presentations Acute cholecystitis Empyema of the gallbladder Mucocele of the gallbladder Biliary colic 'Flatulent dyspepsia' Mirrizi's syndrome Obstructive jaundice Pancreatitis Acute cholangitis Chronic calcular cholecystitis Clinical picture Recurrent attacks of epigastric or right hypochondrial pain (persistent pain) May be attacks of severe biliary colic Nausea &vomiting Flatulent dyspepsia with intolerance to fatty meals Tenderness in right hypochondrium (Murphy’s Treatment : Cholecystectomy either conventional or laparoscopic is the ideal treatment for symptomatic patients. Patients with asymptomatic gall stones can be left without surgery specially if cirrhotics. However patients with a calcified or porcelain gallbladder should consider elective cholecystectomy due to the increased risk of carcinoma (25%). Laparoscopic cholecystectomy (LC) Shown to be equally as effective as open cholecystectomy in controlled trials Pre-operative ERCP is indicated if: Recent jaundice Abnormal liver function tests Significantly dilated common bile duct Ultrasonic suspicion of bile duct stones cholecystectomy Indication Trauma Inflammation Acute & chronic Mucocele empyema Tumor Torsion As a part of other operations cholecystectomy Incisions Subcostal (Kocher’s) Upper right paramedian Right upper transverse Upper midline cholecystectomy Technique Preliminary exploration Signs of cholecystitis Associated pathology Saint’s triade Welkie’s triade Pancrease Stone in CBD Saint’s triade Welkie’s triade Technique Packing of the field & retractors GB is grasped Separation of GB Artery Duct Identification of Calot’s Operative complications Injury to important structure Common bile duct injury: observed more frequently in the laparoscopic approach. Iatrogenic common bile duct injury often results from a combination of inexperience of the surgeon, the presence of anomalous biliary anatomy, and acute inflammation. Duodenum injury Pancreatic and liver injury Ligation of Rt hepatic artery Primary hge Injury of cystic artery Injury of Rt hepatic Injury portal vein GB bed Post operative complications General Chest & abdomen DVT Infection: Spillage of stones into the peritoneal cavity during cholecystectomy increases the risk of infection and abscess formation. Wound infections also are possible but are less common in the laparoscopic approach.. Post operative complications Local Bleeding: Ligation of Reactionary slipped ligature 2 ry hge if infection which may lead to collection above IVC ( Waltman- Walter syndrome) CBD or CHD Hepatic artery Biliary peritonitis Biliary fistula Subphrenic collection Postcholecystectomy syndrome Post cholecystectomy syndrome Organic causes Long stump of cystic duct Missed stone Stricture Stenos is of sphincter of Oddi Non organic causes Psycho-somatic Biliary dyskinesia Long stump of cystic duct If stone is formed Stump must be excised with Stone extraction If no stones symptomatic treatment Missed stone after cholecystectomy Confirm diagnosis by US & ERCP Minimal invasive ERCP sphincterectomy & stone extraction by Dormia Basket PTC then choledochoscpic extrction Surgical Supradoudenal choledochotomy Transdoudenal sphincteroplasty Stricture Minimal invasive by stent insertion Surgical Roux en Y choledocho jujunostomy Roux en Y hepatico jujunostomy Post cholecystectomy syndrome Organic causes Long stump of cystic duct Missed stone Stricture Stenos is of sphincter of Oddi Non organic causes Psycho-somatic Biliary dyskinesia Post cholecystectomy syndrome Stenos is of sphincter of Oddi Endoscopic papillotomy and sphincterotomy Sphincteroplasty Choledocho doudenotomy Biliary dyskinesia Endoscopic papillotomy and sphincterotomy Stone in CBD Aetiology GB stone (commonest) Primary stones of CBD usually (Brown) Parasites Stasis FB cholangitis Clinical picture Symptom less 20 % Symptoms Charcot’s triade Jaundice Pain Fever Raynaud’s Charcot’s pentale triade Hypotension Altered mental status Investigations Laboratory CBC Liver function urine Radiological US ERCP MRCP PTC Management of stone CBD Support liver by correction of the general condition by I.V. fluids for hydration Support kidney by Mannitol (hypotension and hyperbilirubinemia together causes renal shut down) Prevent infection by antibiotics, Prevent bleeding by correction of the avitaminosis K by parentral vitamin administration Concurrent common bile duct and gallbladder stones Preoperative ERCP, with clearance of the common bile duct, followed by LC Open cholecystectomy and common bile duct exploration Combined laparoscopic-endoscopic management: Endoscopic sphincterotomy and stone extraction are performed on the operation table after the surgeon has passed a guidewire through the cystic duct into the duodenum to help the endoscopist because the procedure is performed with the patient in the supine position. Management of a case of stone CBD Minimal invasive Endoscopic extraction of calculi followed by cholecystectomy whether surgical or most commonly laparoscopic PTC which provide drainage and subsequent choledochoscopy & stone extraction Management of a case of stone CBD Conventional choledochtomy Chole cystectomy and supra doudenal choledochtomy choledocholithotomy (exploration of the common bile duct) Trans doudenal sphincterotomy Choledocho douden ostomy Indications of common bile duct exploration (supra doudenal Preoperative confirmation of the presence of CBD stones (U/S, ERCP, or operative cholangiography) Jaundice or history of jaundice History of pancreatitis (although it is usually due to a passing stone) Operative choledochtomy) Stone palpable in CBD Dilated CBD with thick lusterless fibrous wall, with mud inside Dilated cystic duct specially if there is multiple small stones in the gall bladde Postoperative Surgical Jaundice Management of a case of stone CBD T tube insertion which should be Widest possible diameter Latex or red rubber (never plastic) Exist from one side of the choledochotomy wound Horizontal limb is cut to lie below the carina and above the common channel Vertical limb comes out straight from the abdomen T tube cholangiography is done on the 4 th days and tube is extracted at the 10-12 days after 24hour occlusion without problems (fever, leakage, or pain) Management of stone CBD Sphincterotomy or sphincteroplasty done In the presence of stenosed termination of CBD or an impacted stone in its lower end that cannot be extracted from the choledochotomy wound the ampulla is attacked through a duodenal incision and the ampulla should undergo either sphincterotomy or sphincteroplasty at 10 or 11-oclock positions to avoid pancreatic duct injury Management of a stone CBD Chole docho duodenostomy is done (in the following situations) In dilated CBD (more than one cm) In case there is multiple stones (> 4 stones in CBD) because of the high possibility of missing a stone inside Presence of intrahepatic biliary stones Stricture of the lower end of CBD Missed stone after CBD exploration Confirm diagnosis bt US & ERCP Wait for 6 weeks Hydrostatic pressure Minimal invasive ERCP sphincterectomy & stone extraction by Dormia Basket PTC then choledochoscpic extrction Surgical Supradoudenal choledochotomy Transdoudenal sphincteroplasty Jaundice Jaundice Pre-hepatic (Hemolytic) Hepatic Post hepatic (Obstructive) Pre-hepatic (Hemolytic) Congenital abnormal Shape spherocytosis, eleptocytosis Hb thalssemia, sickle cell Enzymes G6 PD, pyruvate kinase Pre-hepatic (Hemolytic) Acquired Immune hemolytic Collagenic SLE, Rheumatoid Tumor lekemia, lymphoma Infections malaria, syphilis Drugs penicillin tetracycline, quinidine, aSPIRIN Non immune Septicemia Burn Metal poisoning Mismatch blood transfusion Haematoma Snake venum Hepatic Acute Viral Amoebic or bacterial Alcoholic Liver cell necrosiis Drugs Direct hepatotoxic A antibiotics (Tetracycline), Analgesic (salycilate, paracetamol) Antihelminthic carbon tetra chloride Anaesthestics fluthane Arsenic Hepatic Drugs Direct hepatotoxic B benzidine dervative TNT C cytotoxic 5FU Intra hepatic cholestasis Non sensitivity methyl testosterone Sensitivity neomercazole, thiuracil, chloropromazine Hypersensitivity PASA Chronic Chronic active Cirrhosis Primary hepatic cirrhosis Space occuping lesions Obstructive jaundice (Etiology) Common Common bile duct stones Carcinoma of the head of pancreas Malignant porta hepatis lymph nodes Infrequent Ampullary carcinoma Pancreatitis Liver secondaries Obstructive jaundice (Etiology) Rare Benign strictures - iatrogenic, trauma Recurrent cholangitis Mirrizi's syndrome Sclerosing cholangitis Cholangiocarcinoma Biliary atresia Choledochal cysts Calcular obstruction Intermittent (can be progressive if stone is impacted) Usually no reaching high levels Pain is colicky in nature, and typical for biliary colic G.B not palpable except very rarely if its neck is obstructed too (double stone) Malignant obstruction Progressive except very rarely in ampullary tumors where sloughing can give temporary decrease Usually reaching high levels Pain is constant and referred to the back in pancreatic tumor, while it is absent in CBD tumors G.B is palpable except in Klatskin tumors Obstructive jaundice Calcular Complications of obstructive jaundice Ascending cholangitis Charcot's triad is classical clinical picture which is formed of intermittent pain, jaundice and fever Cholangitis can lead to hepatic abscesses Need parenteral antibiotics and biliary decompression Operative mortality in elderly of up to 20% Complications of obstructive jaundice Clotting disorders Vitamin K required for gamma-carboxylation of Factors II, VII, IX, XI Vitamin K is fat-soluble. No absorbed. So it needs to be given parenterally Urgent correction will need Fresh Frozen Plasma Also endotoxin activation of complement system Complications of obstructive jaundice Hepato-renal syndrome Poorly understood Renal failure post intervention Most probably due to gram negative endotoxinaemia from gut Preoperative lactulose may improve outcome by improving altered systemic and renal haemodynamics Drug Metabolism Half-life of some drugs prolonged. (E.g. morphine) Impaired wound healing. Investigations for a case of obstructive jaundice Laboratory Raised Direct bilirubin (in most of the cases the indirect bilirubin also rises due to hepatic cellular malfunction). Alkaline phosphatase Gamma glutamyl transferase 5 nucleotidase Investigations for a case of obstructive jaundice Laboratory Mild elevation or normal SGOT & SGPT (these are shooting in viral hepatitis) Slightly depressed or normal Prothrombin time (due to avitaminosis K) Urine urobilinogen Investigations for a case of obstructive jaundice Imaging techniques Ultrasound this is most useful CT (conventional or helical) competes with the U/S especially as regards the pancreatic tumors. ERCP MRCP PTC EUS malignant Treatment for cholangiocarcinoma of CBD Palliative Plastic stent insertion through ERCP Stent insertion through percutanous transhepatic route Self-expanding stainless steel wire biliary endoprosthesis is new modality with high patency rate, and less infection rate Treatment for cholangiocarcinoma of CBD Palliative Bypass surgery Round ligament approach for Klatiskin tumors (on condition that the carina is permitting right to left communication) Hepatico jujenostomy for middle and low tumors Cholecystojujenostomy for low tumors. usually we add gastrojujenostomy and enteroanastomosis (triple anastomosis) for pancreatic head tumors Treatment for cholangiocarcinoma of CBD For operable cancers For Klastiskin tumor, segment IV excision provides good access to the confluence allows good proximal clearance and facilitates hepaticojujenostomy For middle tumors excision of the tumor from just below the carina to the duodenum is done with hepaticojujenostomy For distal tumors. Whipple operation is done Biliary stricture Etiology Congenital (biliary atresia) Traumatic (most important, and usually follow cholecystectomy) Complete ligation of CBD Narrowing of the duct by partial inclusion in a ligature Ischemia of the duct, or diathermy injury Inflammatory Sclerosing cholangitis (multiple strictures separated by normal or dilated segments). Cholangiocarcinoma Sclerosing cholangitis PSC (primary sclerosing choangitis ) is a chronic cholestatic biliary disease characterized by non suppurative inflammation and fibrosis of the biliary ductal system. The cause is unknown but is associated with autoimmune inflammatory diseases such as chronic ulcerative colitis. Sclerosing cholangitis Most patients present with fatigue and pruritus and, occasionally, jaundice. The natural history is variable but involves progressive destruction of the bile ducts, leading to cirrhosis and liver failure. Biliary stricture Investigations used are similar to those used in any case of obstructive jaundice (U/S then CT, ERCP, MRCP or PTC Treatment is centered on creating a biliary enteric anastomosis with mucosa-tomucosa sutures without compromising the blood supply of any of the ends.