Central neuromodulation
advertisement

Neuromodulation for
chronic intractable
primary headache
Laurence Watkins
Victor Horsley Department of Neurosurgery
National Hospital for Neurology & Neurosurgery
BASH Hull January 2011
Neuromodulation in primary
headache disorders
Peripheral neuromodulation
Occipital nerve stimulation
Central neuromodulation
Deep Brain Stimulation
Why?
Results
Procedure
Future
Occipital headaches
Weiner 1995: ONS in patients who
had responded to repeated GON
injection
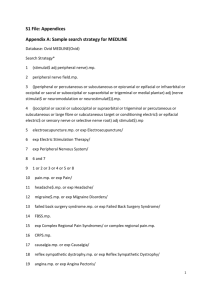
Statistical parametric map (SPM{F}) showing brain regions in which rCBF correlates (positively
or negatively) with pain scores, in particular the dorsal rostral pons, ACC and cuneus (voxels
significant at P
Matharu, M. S. et al. Brain 2004 127:220-230; doi:10.1093/brain/awh022
Copyright restrictions may apply.
Graphs showing (A) mean pain scores and (B) mean scores of stimulator-induced paraesthesia
by scanning states
Matharu, M. S. et al. Brain 2004 127:220-230; doi:10.1093/brain/awh022
Copyright restrictions may apply.
Cervico-trigeminalhypothalamic system
Results of ONS in
cluster headache
Burns B; Watkins L; Goadsby P.
Lancet 2007 369:1099-1106
Treatment of medically intractable
cluster headache by occipital nerve
stimulation: long term follow up of
eight patients
8 patients with chronic
cluster headache
Median 12 years since onset
Median 6 years since became
chronic
Median age 46 years (32-58)
Median follow up 20 months
n=8
2 patients substantial improvement
3 patients moderate improvement
40-80% reduction
1 patient mild improvement
90-95% reduction
25% reduction
6 said they would “recommend it to other
CCH patients”
1 stopped triptan use and 2 reduced
2 patients no improvement
First Meeting
Check have been fully assessed in
Headache Neurology Clinic (chronic,
disabling, intractable)
General fitness & airway satisfactory;
reflux?
MRI ? (because can’t have MRI once
ONS is implanted)
Any major surgery planned ? (because
restriction of monopolar diathermy once
ONS implanted)
Explaining procedure
Discussion with patient
Describing the procedure
Relatively novel operation – NICE
assessment “in progress”
200+ patients so far in our unit since
2002. Now about 1 per week.
Known risks: next slide
Clearance from PCT
Discussion with patient
Known risks:
may not help
infection requiring removal of implant
electrode migration
neck stiffness
breakage or failure of components
tethering to skin or muscle
skin erosion
early depletion of battery
Clearance from PCT
Follow up clinics
Typically 4 in first year
Joint assessment with Headache
Neurologist and Specialist Nurse
(usually on day care unit)
Gradually refine the settings to get
best response (headache diary),
without patient discomfort
Checking for any problems
Stages of the operation
Insertion of electrodes
LA
+ Sedation
Test stimulation of electrodes
Awake
Insertion of battery and tunnelling
of leads
Asleep
(GA with LMA)
Alternatively GA throughout if
difficult airway or reflux
USA: 2 stage procedure
Skin marking
Awake, sitting upright on stool
Midline
Intermastoid line
Spinous process of C1
3cm from midline
Chosen position of battery
Positioning
Lateral position
Access to all operative areas
Strict aseptic technique to
establish field
Anaesthetist access to patient for
communication and airway
Test stimulation
Radiating occipital paraesthesiae
bilaterally
300 microseconds pulse width
60-80 Hz
At low amplitude – typically 1-2V
If no paraesthesiae or if amplitude
>4V then reposition electrode
2-3 days later
Activate implant
Set initial parameters
Pleasant radiating occipital
paraesthesiae bilaterally
Patient education to use handset for
continuous comfortable stimulation
Patient given implant ID card
Advised to restrict strenuous activity in
first 8 weeks
Drive when comfortable, but switch
implant off while driving
Restrictions after 2 months: no MRI,
scuba diving below 10m
Real Life
Some dramatic results but have to
give realistic expectation to
patients. Approximately 70% will
be pleased with result and 30%
disappointed.
Relatively low risk; so may be
justifiable in cases where chronic
headache is disrupting quality of
life and intractable to medical
treatment
Main technical
challenges
Placing electrodes to get paraesthesiae
Anchoring/looping the electrodes
Minimising infection risk
Not “instant” result so can’t really do “trial
electrodes”
Experience with bion
Single electrode on 3cm
rechargeable “capsule”
Unilateral
Need to map position of nerve with
subcutaneous needle electrode
Then place bion at optimal point
Experience with bion
Implanted 10
All unilateral syndromes
6 hemicrania continua
5/6 benefit
Faster onset of benefit (approx 2
weeks) cf cluster (months)
Limitations of bion
Unilateral
Thus not ideal for chronic migraine
and cluster
Single electrode
Thus need nerve mapping and
precise placement
Frequent recharging (daily or in
some patients several times per
day)
Advantages of bion
No wires to tunnel
Thus can be done with local
anaesthetic only
Shorter operation
No migration because no wires
causing tension
Next Steps
RESPONSE trial of ONS in chronic
migraine (large, multicentre,
randomised controlled trial)
CE marking & NICE assessment
Rechargeable stimulators
Smaller stimulators
More experience
Interplay between medication and
neuromodulation
Other inputs into CTH system
Cervico-trigeminalhypothalamic system
Neuromodulation in primary
headache disorders
Peripheral neuromodulation
Occipital nerve stimulation
Central neuromodulation
Deep Brain Stimulation
Conclusions
Consider in patients with
chronic, disabling, intractable
primary headache
ONS and DBS are both “low
risk” when practiced in a
multidisciplinary team and in
experienced hands (but the rare
complications in DBS can be
severe)
Conclusions
May be logical to see ONS as
primary surgery and reserve
DBS for those who don’t
respond or can’t have ONS
Thank you
laurence.watkins@uclh.nhs.uk