Diagnosis of
heart failure
in clinical
practice
Dov Freimark M.D. , F.E.S.C.
Sheiba Medical Centre
Tel HaShomer
Historic Perspectives of Heart
Failure
• Dropsical condition
• Central cardiac pump failure
• Circulatory cardiac pump problem
• Circulatory dysfunction
• Endocrinopathy
• Inflammation
Heart failure is a complicated milieu of pump
dysfunction, remodeling, humoral perturbation and
subsequent circulatory insufficiency.
Definition of heart failure
I.
Symptoms of heart failure (at rest of
during exercise)
and
II. Objective evidence (preferably by
echocardiography) of cardiac dysfunction
(systolic and/or diastolic) (at rest) and (in
cases where the diagnosis is in doubt
and
III. Response to treatment directed towards
heart failure
Criteria I and II should be fulfilled in all cases
European
HeartHeart
Journal
2005;26:1115-1140
European
Journal
2005;26:1115-1140
From Risk to Death
Coronary
Thrombosis
Myocardial
Ischemia
Myocardial
Infarction
Arrhythmia
Loss of
Muscle
Sudden
Death
Neurohormonal
Activation
Remodeling
CAD
Atherosclerosis
LVH
Risk Factors
•Hyperlipidemia
•Hypertension
•Diabetes
•Insulin resistance
•Smoking
•Sex
Ventricular
Dilatation
Heart
Failure
Death
Dzau V. Braunwald E. Am Heart J 1991. 121 1244-1263
Management Outline
Monitor progress
Choose therapy
Evaluate Prognosis
Evaluate co-morbidity
Determine etiology
Assess severity of limitation
Identify major symptoms
Establish diagnosis
A correct diagnosis is the cornerstone
try to make the diagnosis early
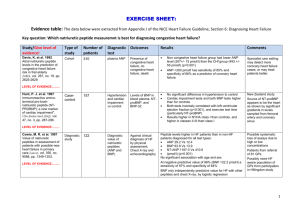
Inspecting the Data
What are we looking for?
Clinical Diagnostic Assessment
routine
•
•
•
•
•
•
•
history
physical examination
EKG
chest x-ray
laboratory
echo
BNP
optional
•
•
•
•
exercise testing
hemodynamics
imaging techniques
angiography
European Journal of Heart Failure
2005;7:291-429
Clinical Trials Lesson?
How do we interpret the information?
History
• cardiovascular events
• cardiovascular surgery or PTCA
• risk profile (family, smoking, hyperlipidemia,
hypertension, diabetes, alcohol)
• other systemic disease/comorbidity (conditions
that mimic heart failure)
• Sleep apnea?
• major surgery
• current therapy
• response to previous therapy
• Compliance0
• Social support
Clinical Status
Symptoms
• angina
• dyspnea
• exercise capacity
Signs
•
•
•
•
•
•
•
•
•
•
appearance
heart rate and rhythm
blood pressure, pulse pressure
pulmonary rales
gallop rhythm
mitral insufficiency
aortic stenosis, insufficiency
jugular venous, hepatic congestion
peripheral edema
pleural/pericardial effusion, ascites
Initial Rapid Clinical Patient
Assessment
Congestion at Rest
No
No
Low
Perfusion
at Rest
Yes
Yes
Warm & Dry
PCW normal
CI normal (compensated)
Warm & Wet
PCW elevated
CI normal
Cold & Dry
PCW low/normal
CI decreased
Cold & Wet
PCW elevated
CI decreased
Normal SVR
High SVR
The Cleveland Clinic
Center for Continuing Education
Rest ECG
•rate
•rhythm
•dysrhythmia
•hypertrophy, strain
•Q-wave infarction
•ischemia
•QT interval, dispersion
•QRS duration
Ambulant Holter Monitoring
•heart rate
•supraventricular tachycardia
•ventricular dysrhythmia
•bradycardia
•silent ischemia
•heart rate variability
Chest X-ray
•
•
•
•
•
heart size and form
pulmonary congestion
signs of COPD
infiltrates/pneumonia
pleural effusion
Hemodynamics
•
•
•
•
•
systemic arterial pressures
pulmonary arterial pressures
filling pressures
cardiac output
systemic vascular resistance
• most useful to assess acute response to an intervention
and for evaluation of a heart transplantation candidate
Laboratory
•
•
•
•
•
•
•
•
•
•
•
hemoglobin
white cells, CRP
renal function
liver function tests
thyroid status
blood sugar
lipid profile
blood gases
drug levels
troponins
BNP
BNP use
• Considerable literature supports the use
of BNP testing in:
•
•
•
•
•
Screening
Triage ( high negative predictive value)
Assessment of prognosis
Titrating pharmacological therapy
Diastolic dysfunction
BNP and final diagnosis
Mean BNP Concentration
(pg/ml)
1400
1200
1000
800
600
400
200
0
No CHF
(n=770)
Dyspnoea,
non-cardiac cause
but history of LVD
(n=72)
Dyspnoea
due to CHF
(n=744)
Maisel A. et al. J Am Coll Cardiol 2001;37(2):379-85
BNP LEVELS DURING HOSPITALISATION
n=105
JACC 2004;43:4:635-641
Echo indices
•chamber dimensions
•hypertrophy
•focal hypokinesis
•ejection fraction
•pulmonary artery pressure
•dyssynchony?
•aortic stenosis/insufficiency
•mitral insufficiency
•diastolic mitral flow pattern
•relaxation indices
•tissue Doppler
Diastolic Heart Failure Definition
• Signs and / or symptoms of CHF
• Normal or mildly reduced left ventricular
systolic function (EF > 45%)
• Evidence of abnormal left ventricular
relaxation, filling, diastolic distensibility and
diastolic stiffness
European Study Group on Diastolic Heart Failure et al. Eur Heart J 1998
The updated ESC guidelines
”Most, if not all, patients with systolic
dysfunction have changes in diastolic
function”.
”Therefore, diastolic and systolic heart
failure should not be considered as
separate pathophysiologic entities”.
European Heart Journal 2005;26:1115-1140
ClinicalDiagnosis
Circulation: 2002;105:1387-1393
Exercise Test
Protocol
•
•
•
•
bicycle
treadmill
floor
gas exchange
• maximal
• submax (6 min walk)
• endurance
Information
limiting symptom
chronotropic response
arrhythmia
blood pressure response
work performed
VO2 max.
ischemia
Coronary disease and heart failure
Mechanisms
• infarction
• ischemia
• stunning
• hibernation
Diagnosis should include detecting
potential reversibility
(hibernating myocardium)
•
•
•
•
•
Thallium scan
Technetium (sestamibi) scan
PET mismatch
Stress Echo
Contrast MRI
• low threshold for angiography
Indications for Coronary Angiography
Evidence suggesting
CAD
•history
•rest ECG
•exercise ECG
•ambulant monitoring
•perfusion studies
Coronary angiography
• extent of coronary disease
• ventricular function
• end diastolic pressure
• valvular disease
•
potential for PCI/CABG
Lower Risk
Higher Risk
Ejection fraction
> .40
< .20
Cardiac index, L/min/m2
> 2.5
< 2.5
PCWP, mm Hg
< 18
> 12
MVO2, ml/kg/min
> 20
< 10
Heart rhythm
Sinus
VT of A . Fib
Heart rate
< 90
> 100
Serum Na+ (mmol/L)
> 135
< 135
LVEF has no Correlation
with Functional Capacity
Am J Cardiol 1984;54:596
StentingThank
has changed
youeverything