Template
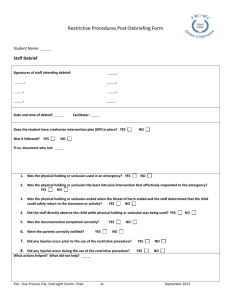
advertisement
FHM TRAINING TOOLS This training presentation is part of FHM’s commitment to creating and keeping safe workplaces. Be sure to check out all the training programs that are specific to your industry. Addressing Combative Patients ►►► These materials have been developed based on applicable federal laws and regulations in place at the time the materials were created. The program is being provided for educational and informational purposes only and does not constitute and is not intended to provide OSHA compliance certification, regulatory compliance, a substitute for any "hands on“ training required by applicable laws and regulations, or other legal or professional advice or services. By accessing the materials, you assume all responsibility and risk arising from the use of the content contained therein. ©2010 Grainger Safety Services, Inc. Learning Objectives At the conclusion of this presentation, you will: ► Recognize potential for encounters with combative patients ► Possess options to evaluate, control, and defuse situations Course Agenda Agenda: ► Epidemiology ► Responding of combative behavior to the threat of violence Section 1 The Epidemiology of Combative Behavior Definition NIOSH defines workplace violence as violent acts directed toward persons at work or on duty: ► Examples: – Threats – Physical assaults – Muggings Frequency Over 5 million in the U.S. work in healthcare: ► Exposed ► High to many safety and health hazards risk for experiencing workplace violence ► Bureau of Labor Statistics (BLS) estimates assaults four times higher than other industries Predicting Violent Behavior Warning signs: ► Pacing or restlessness ► Clenched fist ► Increasingly ► Excessive ► Threats ► Cursing loud speech insistence Delaying Care Major problems of combative patient: ► Potential ► Delay for injury in care Behavior may be result of medical or surgical condition: ► Treat agitations, resolve behavioral problems ► Address behavior then care Establishing a Clear Approach OSHA recommends that employers establish and maintain a written violence prevention plan: ► Creates a policy that violence will not be tolerated ► No reprisals against employees reporting or experience violence ► Encourages ► Establishes incident reporting and recordkeeping a plan for maintaining security Activities Related to Violence Violence often takes place during: ► Meal times ► Visiting hours ► Patient transportation Assaults may occur when: ► Service ► Patient ► Limits is denied is involuntarily admitted set on eating, drinking, tobacco, or alcohol use Who is at Risk? Personnel at high risk: ► Nurses ► Aides Personnel at increased risk: ► Emergency ► Safety response officers ► Healthcare providers Where May Violence Occur? Areas violence frequently occurs: ► Psychiatric ► Emergency ► Waiting wards rooms rooms ► Geriatric units Section 2 Responding to the Threat of Violence Prevention Strategies Five progressive strategies: ► Administrative ► Verbal controls de-escalation ► Seclusion ► Physical restraints ► Medication Least Restrictive Alternative Doctrine Least restrictive alternative doctrine: ► Individuals should be provided with any necessary care, treatment, and support in the least invasive manner, and in the least restrictive manner and environment compatible with the delivery of safe and effective care, taking into account, where appropriate, the safety of others Administrative Controls Administrative controls include: ► Design waiting areas to accommodate for delays ► Minimize bright lights, loud radios, TVs, speaker messages, heavy traffic ► Arrange furniture and other objects to minimize their use as weapons ► Ensure adequate staff at scene Verbal De-Escalation Three main themes to continually convey: ► Express concern for patient well-being ► Emphasize staff in control ► Reassure no harm Also: ► Maintain a means of egress ► Vigilant of body language ► Maintain calm, controlled tone Escalating Behavior Escalating behavior: ►Be consistent ►Patients may attempt to split staff Defining Limits Verbal de-escalation should include: ► Defined limits ► Consequences Signs of Impending Violence Warnings of impending violence: ► Changes ► Loud in patient mood or aggressive speech ► Increasing ► Signs psychomotor activity not always evident Unsuccessful De-Escalation If less restrictive efforts fail: ► Restraints ► Seclusion ► Medication Moving Beyond Verbal De-Escalation To go beyond verbal de-escalation: ► Sufficient ► Treat trained personnel patients with dignity Seclusion Seclusion serves to: ► Decrease ► Permit external stimuli time to regain control Seclusion is not good if patients: ► Have unstable medical conditions ► Need close interaction or monitoring Preparing for Seclusion Pay attention to environment: ► “Sharps” ► Artificial, natural lighting ► Cooling, heating, ventilation ► Toilet ► How facilities, bed and cleanness staff will see and communicate Managing the Secluded Patient The patient should be: ► Reminded of consequences ► Monitored at least every 15 minutes ► Monitored by closed-circuit television, if available Principles of Physical Restraint Principles of patient restraints: ► Individualized ► Humanely ► Protocols ► Usage ► Least and afford dignity administered developed carefully documented restrictive necessary Managing the Restrained Patient Establish parameters of patient monitoring while in restraints: ► Monitor need for continued restraint ► Check distal circulation frequently, adjust as necessary ► Remove one limb at a time Medication Medication: ► In addition to physical restraint ► Control behavior to perform evaluation and treatment ► Effective for violent behavior due to psychiatric, emotional, or medical causes The Risk of Medication Risks of using medications: ► Introduce ► Obscure complications physical exam Documenting Behavioral Control Documentation includes: ► The emergency and explanation for treatment ► Refused or unable to give consent ► Evidence ► Failures ► Explain of incompetence to refuse treatment of less restrictive methods of control techniques used and any injuries incurred ►Section 3 Additional Information Additional Information Violence: Occupational Hazards in Hospitals. National Institute of Occupational Safety and Health (NIOSH) Publication No. 2002-101, (2002, April) Center for Medicare and Medicaid Services website: ww.cms.gov