Sux Apnoea - A Case Study
advertisement

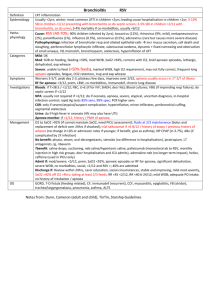
Sux Apnoea - A Case Study Karenne Nielsen Clinical Nurse Specialist West Gippsland Healthcare Group Suxamethonium Chloride “Sux” “Scoline” Short acting muscle relaxant Allows rapid intubation of trachea & provides short periods of neuromuscular blockade Main uses - difficult intubation - emergency conditions - brief procedures Suxamethonium “Sux” Dose = 1-2 mgs/kg IVI or IMI Rapid onset of muscle relaxation - fasciculation 30-60 seconds Short duration of 5-10 minutes - apnoea lasts ≈ 5 mins - paralysis recovery another 5 mins Suxamethonium – “Sux” Metabolised by plasma cholinesterase - an enzyme produced in the liver & present in the blood Plasma cholinesterase is usually present in sufficient concentration to give a half-life of approx. 4 mins No reversal agent Side effects Cardiovascular – bradycardia Hyperkalaemia Raised intraocular/pressure Allergic reaction → Anaphylaxis Malignant hyperthermia Muscle pains- calf & chest Prolonged muscle paralysis “Sux apnoea” Rare condition in 4-6% population Patients with abnormal plasma cholinesterase are incapable of metabolising suxamethonium resulting in prolonged muscle paralysis and apnoea. Inherited - often normal levels but abnormal plasma cholinesterase (up to 8hrs or more) Acquired – lower levels of normal plasma cholinesterase Case study 55 year old Female No significant medical/family history Nil current medications Non smoker Surgical & Anaesthetic history - Varicose Vein Ligation 2002 - GA no muscle relaxants Pre-Anaesthetic Assessment Weight: 77.5 kgs / Height: 156cm Reflux lying flat in bed “High risk of gastric reflux” Undershot jaw – Airway Grade III “? Difficult intubation” ASA score 2 Anxious patient ++ Anaesthetic drugs Midazolam 2mgs IVI Fentanyl 100µgs IVI Propofol 200mgs IVI Suxamethonium 100mgs IVI @ 1355 Nitrous/Oxygen 2:2 Sevoflurane 2% Cephazolin 1gm IVI Anaesthetic/Operation Ventral Hernia Repair with Mesh - surgery straightforward = 1hr No muscle movement noted throughout the operation – end time 1hr & 10 mins after “sux”given Sux apnoea or another diagnosis ? Assumption of Sux apnoea confirmed by nerve stimulation Management Anaesthesia maintained - important to be patient - keep asleep and unaware Continuous monitoring Entropy monitoring Fluid and electrolyte balance Temperature BSL Management Urinary catheter Pressure area care Calf stimulation Eye care Wound/drain care Nerve stimulator Plan for emergency surgery Management Relatives kept informed & to visit - truthful explanation of condition - reassure safe & waiting to wake - ? Fresh Frozen Plasma Started to swallow @ 6½hrs Extubated 30 mins later Total time = 7 hours Recovery Drowsy Co-operative and talking No recollection Required narcotic analgesia Very dry mouth Puffy eyes Husband to visit Post-op period Hypokalaemia post op day 1& 2 - Potassium replaced IVI & orally Febrile post op day 2 - CXR ? pneumonia - oral antibiotics Erythema of wound day 3 Discharged post op day 5 Follow up for Sux Apnoea Review 1 month post-op Debriefing with family present - Sux Apnoea episode - Importance of alerting staff with future anaesthetics Pseudocholinesterase typing & Phenotype differentiation Patient and family tested Follow up testing Normal Dibucaine = over 70% Homozygous normal = (6.0-15.6) “K” – Dibucaine Inhibition = 15% confirming susceptibility to “Sux” Genotype testing unavailable but length of apnoea suggests rare clinical variant Children 4/6 tested – all normal levels The end!! Thankyou very much for your attention.