Bronchiolitis fact sheet
advertisement

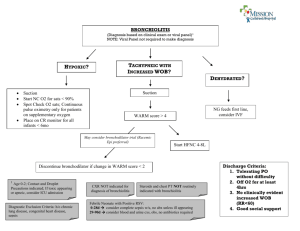
Bronchiolitis Definition Epidemiology Pathophysiology Categories Symptoms Investigations Management DD RSV LRT inflammation Usually <2yrs; winter; most common LRTI in children <2yrs; leading cause hospitalisation in children <1yr; 3-10% SBI in children <1/12 presenting with bronchiolitis so do septic screen; 3-5% SBI in children >2/12 with bronchiolitis, so do urine; 3-4% mortality if co-morbidities, usually <6/12 Cause: RSV (40-70%; 90% children infected by 2yrs), bocavirus (12%), rhinovirus (9%, mild), metapneumovirus (2%), parainfluenza (1%), influenza (0.5%), coronavirus (0.5%), adenovirus (rare but causes more severe disease) Pathophysiology: Infection of bronchiolar resp and ciliated epithelial cells incr mucus secretion, cell death and sloughing, peribronchiolar lymphocytic infiltrate, submucosal oedema, dynamic + fixed narrowing and obstruction of small airways, VQ mismatch, bronchospasm, atelectasis, hyperinflation of LRT Mild: OK Mod: SOB on feeding, feeding >50%, mod WOB, SaO2 <94%, corrects with O2, brief apnoeic episodes, lethargic, dehydrated, exp wheeze Severe: unable to feed (<50% feeds), marked WOB, high O2 requirement, may not fully correct, frequent long apnoeic episodes, fatigue, CO2 retention, insp and exp wheeze Worsens 3-5/7, peak day 2-3, plateaus few days, improves over 2/52; apnoea usually occurs in 1st 3/7 of illness RF for apnoea: <3/12, prem, LBW, co-morbidities, immunodef, chronic lung disease Bloods: if T>38.5 / <1/12; FBC; U+E (if for IVF; SIADH, decr Na); Blood cultures; VBG (if impending resp failure); do septic screen if <1/12 NPA: usually not required if >2/12; do if neonate, apnoea, severe, atypical, uncertain diagnosis, in-hospital infection control; rapid Ag tests 85% sens, 99% spec; PCR higher sens CXR: only if severe/atypical/suspect complication; hyperinflation, minor infiltrates, peribronchial cuffing, segmental atelectasis Urine: do if high fever in neonate (4% may also have UTI) Apnoea monitor: if <1/12, history / PMH of apnoea O2 to SaO2 >92% (if cannot maintain SaO2, need PICU assessment); fluids at 2/3 maintenance (bolus and replacement of deficit over 24hrs if shocked); trial salbutamol if >6-8/12 / history of atopy / previous history of wheeze (no change in LOS or admission rates if younger; if benefit, give as asthma), NP CPAP (in 3-7%), ABx (if complicated by 2Y infection) No benefit: physio, steam, oral decongestants, steroids (no difference in hospitalisation), ipratropium, LT antagonists, Ig, ribavarin ?benefit: saline drops, suctioning, neb saline/hypertonic saline, palivizumab (monoclonal ab to RSV, monthly injection in high risk groups, decr hospitalisation and ICU admits), adrenaline neb (no longer term impact), heliox, caffeine (used in PICU only) Admit if: mod/severe; <3/12, prem, SaO2 <92%, apnoeic episodes or RF for apnoea, significant dehydration, severe WOB, co-morbidities, social, <1/12 and RSV +; 40% are admitted Discharge if: Review within 24hrs, carer education, social circumstances, stable and improving, mild-mod severity, SaO2 >92% off O2 >4hrs; taking at least 2/3 feeds; RR <45 <2/12, RR <40 6-24/12; mild WOB; adequate PO intake; no history of intubation / apnoea GORD, T-O fistula (feeding related), CF, immunodef (recurrent), CCF, myocarditis, epiglottitis, FB (stridor), trachea/largyngomalacia, pneumonia, asthma, ALTE Notes from: Dunn, Cameron (adult and child), TinTin, Starship Guidelines