VTE / thromboprophylaxis
advertisement

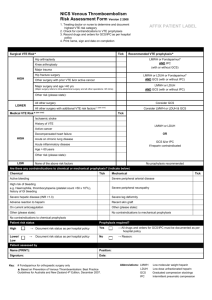
Preventing Venous Thromboembolism in Surgical and Medical Patients Susan Kahn MD MSc Director, JGH Thrombosis Program March 2011 Learning Objectives To understand the importance of thromboprophylaxis in hospitalized patients To be aware of the most recent ACCP consensus guidelines on venous thromboembolism (VTE) prevention 2008 VTE: a very important and costly complication of hospitalization 70% of all VTE in the community is attributable to recent hospitalization!! 2nd most common cause of excess length of stay 3rd most common cause of excess mortality Doubles LOS and costs Autopsy: Fatal Pulmonary Embolism Rationale for VTE prophylaxis 1. 2. 3. High frequency in most hospitalized patients Adverse consequences of unprevented VTE are numerous (PE death, PE, recVTE, PTS, complications of AC) Thromboprophylaxis is effective, safe and cost-effective Risk of DVT in Hospitalized Patients (no thromboprophylaxis, and routine screening for DVT) Patient group DVT prevalence, % Medical patients 10-20 General Surgery 15-40 Major gynecologic surgery 15-40 Major urologic surgery 15-40 Neurosurgery 15-40 Stroke Hip, knee arthoplasty, hip fracture Major trauma 20-40 40-60 Spinal cord injury 60-80 40-80 Moderate risk High risk Fig 1 Relative risk of venous thromboembolism by time since inpatient surgery and since day case surgery Sweetland, S. et al. BMJ 2009;339:b4583 Copyright ©2009 BMJ Publishing Group Ltd. Thromboprophylaxis What is the evidence?… Hundreds of RCTs show that thromboprophylaxis reduces: DVT PE Fatal PE All-cause mortality Costs Thromboprophylaxis Ranked number 1 of >75 strategies to improve patient safety in hospitalized patients More than 25 published evidence-based guidelines since 1986 show clear evidence of benefit and safety ACCP Guidelines: Every hospital should have a formal thromboppx protocol 11 Thromboembolism risk groups addressed by ACCP guidelines General surgery Vascular surgery Gynecologic surgery Urologic surgery Thoracic surgery Laparoscopic surgery CABG Knee arthoplasty Hip arthoplasty Knee arthoscopy Hip fracture surgery Spine surgery Lower extremity injuries Neurosurgery Major trauma Spinal cord injuries Burn patients Medical patients Cancer patients CVCs Critical care patients Long distance travel Geerts-Chest 2008;133:381S Recommendation Grades Grade 1 (strong recommendation) Desirable effects clearly outweigh undesirable effects or vice versa (secondary side effects, costs, patient inconvenience) Can apply to most patients in most to many circumstances Grade 2 (weak recommendation: “suggestion”) Desirable and undesirable effects closely balanced Best action may differ depending on patient circumstances or society values Guyatt GH et al. Grades of recommendation for antithrombotic agents. Chest 2008; 133:123S-131S Quality of Evidence QUALITY METHODOLOGY Strong (A) Moderate (B) Weak (C) One or more well-designed and wellexecuted RCT Well-done observational studies with very large effects (RRR>=80%) RCTs with important limitations Well-done observational studies with large effects (RRR>=50%) RCTS with very serious limitations Observational studies yielding modest effects Guyatt GH et al. Grades of recommendation for antithrombotic agents. Chest 2008; 133:123S-131S Choose best thromboprophylaxis for: • 80 yo F obese post hip # surgery • 35 yo M appendectomy • 72 yo F for ovarian cancer resection, recent GI bleed • 68 yo for colon cancer resection; MVR with prior embolic TIA PREVENTION OF VTE GENERAL RECOMMENDATIONS (I) Mechanical methods of thromboprophylaxis be used primarily in patients at high risk of bleeding (Grade 1A), or possibly as an adjunct to anticoagulant-based thromboprophylaxis (Grade 2A). Graduated compression stockings Intermittent pneumatic compression Venous foot pump Increase venous outflow and/or reduce venous stasis Recommend against use of aspirin alone as thromboprophylaxis for any patient group (Grade 1A) Renal function should be considered when making decisions about the use and/or dose of LMWH, fondaparinux, and other ACs cleared by the kidney, especially in elderly patients, diabetics, or if high risk of bleeding. One of the following is recommended (Grade 1B): Avoid use of AC that bioaccumulates with renal impairment, OR Use lower dose OR Monitor drug level or AC level Geerts WH et al. Prevention of venous thromboembolism Chest 2008;133:381S-453S. Mechanical prophylaxis Advantages Can be used in high risk bleeding patients Efficacy demonstrated in a number of patient groups May enhance effectiveness of AC thromboprophylaxis May reduce leg swelling Disadvantages Not as intensively studied as pharmacologic strategies (fewer studies and smaller) No established standards Many devices never tested in RCTs Almost all RCTs unblinded In high risk groups, less effective then AC thromboprophylaxis Greater effect on reducing calf DVT than proximal DVT Effect on PE or death unknown Compliance by patients and staff often poor Cost associated with purchase, storage, dispensing and cleaning, ensuring optimal compliance Anti-embolic (TED) stocking IPC: Sequential Compression Device (SCD) IPC: Foot pump VTE prophylaxis: Risk groups and recommended thromboppx Levels of Risk Low risk - Minor surgery in mobile patients - Medical patients who are fully mobile Moderate risk - Most general, open gynecologic or urologic surgery patients - Medical patients, bed rest or sick - Moderate VTE risk plus high bleeding risk High risk - Hip or knee arthroplasty, HFS - Major trauma, SCI - High VTE risk plus high bleeding risk Approximate DVT Risk Without Thromboprophylaxis <10 % 10–40 % Suggested Thromboprophylaxis Options‡ No specific thromboprophylaxis and “aggressive” ambulation LMWH (at recommended doses), LDUH bid or tid, Fondaparinux Mechanical thromboprophylaxis 40–80 % LMWH (at recommended doses), Fondaparinux, Oral vitamin K antagonist (INR 2–3) Mechanical thromboprophylaxis Geerts WH et al. Prevention of venous thromboembolism Chest 2008;133:381S-453S. UFH BID vs. TID Patient-specific high risk features for VTE Previous VTE Increasing age Obesity Immobility, lower-extremity paresis Cancer (active or occult) Cancer therapy (hormonal, chemotherapy, angiogenesis inhibitors, radiotherapy) Venous compression (tumor, hematoma, arterial abnormality) Central venous catheterization Acute medical illness Pregnancy and the postpartum period Estrogen-containing oral contraceptives or hormone replacement therapy Selective estrogen receptor modulators Erythropoiesis-stimulating agents Inflammatory bowel disease Nephrotic syndrome Myeloproliferative disorders Paroxysmal nocturnal hemoglobinuria Inherited or acquired thrombophilia Trauma (major trauma or lowerextremity injury) Geerts WH et al. Prevention of venous thromboembolism Chest 2008;133:381S-453S. Low risk of VTE Patient group: • • Medical – fully mobile, brief admission Surgical – procedure < 30 min, mobile, and no additional VTE risk factors • • Laparoscopic surgeries (gynecologic, gen Sx) Transurethral procedures Endoscopic procedures Recommendations: No specific prophylaxis mobilization Geerts-Chest 2008;133:381S Moderate Risk: General Surgery Recommendation/Suggestion Major procedure for benign disease Major procedure for cancer related surgery Major and multiple RFs for VTE High risk of bleeding Grade LMWH LDUH bid Fondaparinux 1A LMWH LDUH tid Fondaparinux 1A LMWH + mechanical method LDUH tid + mechanical method Fondaparinux + mechanical method 1C Properly fitted GCS or IPC . When risk of bleeding decreases, AC be substituted or added 1A 1C For most patients, prophylaxis until discharge (and not mobilization) (grade 1A) For selected high risk general surgery patients (cancer surgery, previous VTE), consider LMWH for 28 days (grade 2A) ACCP Antithrombotic and Thrombolytic therapy: CHEST 133, June2008 Moderate Risk: Gynecologic Surgery Recommendation/Suggestion Entirely laparoscopic surgery in whom there are additional VTE risk factors Major open procedure for benign disease Major open procedure for cancer or multiple RFs for VTE Grade LMWH LDUH bid IPC GCS 1C LMWH LDUH bid IPC just before surgery and used continuously while patient not ambulating 1A 1A 1C LMWH LDUH tid IPC just before surgery and used continuously while patient not ambulating Any of above pharmacologic strategies with GCS or IPC 1A 1A 1A 1C For most patients, prophylaxis until discharge (not mobilization) (grade 1A) For selected high risk general surgery patients (cancer surgery, previous VTE), consider LMWH for 28 days (grade 2C) Moderate Risk: Urologic Surgery Major open procedure Major open procedure at high risk of bleeding Recommendation/Suggestion Grade LDUH bid or tid IPC just before surgery and used continuously while patient not ambulating LMWH Fondaparinux Any of above pharmacologic methods with optimal use of GCS or IPC 1B 1B Properly fitted GCS or IPC . When risk of bleeding decreases, pharmacologic thromboprophylaxis be substituted or added 1C 1C 1C 1A 1C For most patients, prophylaxis until discharge (and not mobilization) (grade 1A) For selected high risk general surgery patients (cancer surgery, previous VTE), consider LMWH for 28 days (???) Moderate Risk: Laparoscopic Surgery Recommendation/Suggestion Routine Additional VTE risk factors Grade No prophylaxis Mobilization 1B LMWH LDUH bid Fondaparinux Mechanical methods 1C • Considerable uncertainty •VTE rates appear to be low: 0%-5% screened DVT; 0.03%-0.06% symptomatic VTE •Pneumoperitoneum and reverse Trendelenburg may impact VTE risk • Only 3 RCTs (LMWH vs placebo or mechanical) of thromboprophylaxis (very small studies, heterogenous, venogram endpoints): no difference •Society of American Gastrointestinal Endoscopic Surgeons recommends the use of similar thromboprophylaxis options as for the equivalent open surgical procedures. Moderate Risk: Bariatric Surgery Recommendation/Suggestion Inpatient bariatric surgery LMWH Higher doses LDUH tid than usual Fondaparinux Mechanical methods with any of the above pharmacologic methods Grade 1C •VTE rates vary widely (0.2%-2%); Fatal PE (0.2%) •Optimal dose, timing and duration unknown • Only 1 small RCT of thromboprophylaxis (nadroparin 5700 IU vs 9500 IU; no difference (no events at 3 and 6 months)) For most patients, prophylaxis until discharge (and not mobilization) (grade 1A) For selected high risk general surgery patients (cancer surgery, previous VTE), consider LMWH for 28 days (???) Moderate Risk: Neurosurgery Recommendation/Suggestion Major neurosurgery If high risk of thrombosis (eg. cancer) Grade Optimal use of IPC Post-operative LMWH LDUH 1A 2A 2B Mechanical method be combined with LDUH or post-operative LMWH 2B • Intracranial (vs spinal), malignancy, prolonged procedures, leg weakness are important RFs for VTE in neurosurgery • Glioma patients carry a post-operative VTE risk of 15-25% at 3 months • Mechanical thromboprophylaxis most studied in this population (RRR 68% compared to no thromboprophylaxis) • GCS alone not as effective as IPC • GCS alone is not as effective as combination LDUH and GCS • Concerns of bleeding with preoperative or early postoperative LMWH in craniotomy patients (2-fold higher risk of bleeding at any site vs. mechanical or no thromboprophylaxis) High risk of VTE: Elective hip replacement Situation Recommendation Grade LMWH High risk dose 12 h pre-op or 12-24 h post-op Half dose 4-6 h post-op then high dose following day All THR patients 1A Fondaparinux 2.5 mg 6-24 h post-op VKA INR 2.5 Use of: ASA or Dextran or LDUH • GCS or VFP • Do not use as sole method of thromboprophylaxis 2A VFP or IPC If high risk of bleeding When bleeding risk decreases 1A Add or substitute pharmacological prophylaxis 1C Geerts-Chest 2008;133:381S High risk of VTE: Hip fracture surgery Situation Recommendation Grade HFS: routine prophylaxis Fondaparinux LMWH Adjusted VKA INR 2.5 LDUH Use of ASA Against use of ASA alone 1A If surgery delayed LMWH or LDUH during time between admission and surgery 1C VFP (Venous foot pump) or IPC 1A If high risk of bleeding When bleeding risk decreases Add or substitute pharmacological prophylaxis 1A 1B 1B 1B 1C Geerts-Chest 2008;133:381S High risk of VTE: Elective knee replacement Situation Recommendation Grade Routine prophylaxis Fondaparinux LMWH Adjusted VKA INR 2.5 1A 1A 1A Alternative option Optimal use of IPC 1B Use of: Against use as only method of thromboprophylaxis • ASA or LDUH If high risk of bleeding When bleeding risk decreases IPC VFP Add or substitute pharmacological prophylaxis 1A 1B 1A 1B 1C Geerts-Chest 2008;133:381S Duration of prophylaxis and orthopaedics Situation THR, TKR, HFS THR Recommendation At least 10 days 1A Extend from 10 up to 35 days 1A LMWH • VKA • Fondaparinux 1A •1B •1C • • Extend from 10 to up to 35 days TKR LMWH • VKA • Fondaparinux Fondaparinux • LMWH • VKA • 1B 1C •1C •1C • • Extend from 10 to up to 35 days HFS Grade 1A 1A • 1C • 1C • Geerts-Chest 2008;133:381S Knee arthoscopy Situation Suggestion Grade No additional VTE risk factors No prophylaxis Early mobilization 2B Additional risk factors LMWH 1B Geerts-Chest 2008;133:381S RECORD3: TKR patients, 10 days Rx Rivaroxaban: oral direct Factor Xa inhibitor 20 Total VTE RRR 49% Enoxaparin 40 mg od Rivaroxaban 10 mg od Incidence (%) 15 10 Major VTE 5 Symptomatic VTE RRR 62% 18.9% 0 9.6% 2.6% 1.0% RRR 65% 2.0% 0.7% Major bleeding NS 0.5% 0.6% RECORD1: THR patients, 35 days Rx 5 Rivaroxaban 10 mg once daily Enoxaparin 40 mg once daily Total VTE Incidence (%) 4 RRR 70% 3 Major VTE RRR 88% 2 Symptomatic VTE Major bleeding 1 3.7% 0 1.1% 2.0% 0.2% 0.5% 0.3% 0.1% 0.3% Patients with Renal impairment No dose adjustment required in patients with mild (CrCl >50 mL/min) or moderate (CLCR: 30-49 mL/min) renal impairment Subjects with CLCR <30ml/min excluded from clinical trial program. Limited clinical data: rivaroxaban levels sig increased in such patients Moderate risk: Patients hospitalized for a medical condition Recommendation/suggestion 1. 2. 3. Congestive heart failure Severe respiratory disease Confined bed rest with one or more of: • • • • Active cancer Previous VTE Acute neurologic disease Inflammatory bowel disease For some patients if contraindication to anticoagulation prophylaxis LMWH or LDUH bid or Fondaparinux Grade Mechanical thromboprophylaxis with GCS or IPC 1A 1A 50-70% of symptomatic VTE and 70-80% of fatal PE occur in hospitalized medical patients Geerts-Chest 2008;133:381S Moderate risk: Patients hospitalized for a medical condition Optimal duration remains unclear (EXCLAIM study) 4000 ill medical patients Enoxaparin 6-14 days vs. 28 days VTE at 1 month (enox 4.9% vs. extended enox 2.8%) (p<0.05) Major bleeding (1.1% extended enox vs. 0.3% enox) (p<0.05) No impact on all-cause mortality Geerts-Chest 2008;133:381S Moderate risk: Critical Care patients VTE risk varies considerably Most ICU patients have multiple risk factors Some acquired RFs include: pharmacologic paralysis, CVC lines, surgical procedures sepsis, mechanical ventilation vasopressor use, renal dialysis Also, have risk factors for bleeding Trauma Surgery Low platelets Liver disease Geerts-Chest 2008;133:381S Moderate risk: Critical Care patients Recommendation/Suggestion Grade Any admitted patient Assessment for VTE risk Routine prophylaxis in most 1A Moderate risk of VTE (medically ill or postoperative general surgery) LMWH or LDUH bid 1A High risk of VTE (major trauma or orthopedic surgery) LMWH (extrapolate from major trauma and orthopedics population) 1A GCS and / or IPC 1A If high risk of bleeding When bleeding risk decreases Add or substitute LMWH / LDUH 1C Geerts-Chest 2008;133:381S High risk: Hospitalized cancer patients Recommendation/Suggestion Surgery Appropriate for the type of surgery LWMH=LDUH tid Grade 1A Bedridden with an acute Thromboprophylaxis as for other high risk medical patients medical illness 1A Chemotherapy or hormonal therapy 1C Indwelling CVCs Ambulating, nonhospitalized No role for prophylaxis No role for prophylactic doses of LMWH or mini-dose warfarin 1B No role for prophylaxis to improve survival 1B Geerts-Chest 2008;133:381S Basic principles • • • • • • • • Think about VTE prophylaxis in each and every patient Assess risk of VTE Determine if contraindications present Assess if patient is in a higher than usual risk group that might require more aggressive approach (stepped up dose, dual modality, longer duration): e.g. previous VTE, cancer, prolonged immobilization REMEMBER to prescribe thromboprophylaxis Assess ongoing need for thromboprophylaxis (or resolution of contraindications) regularly Low threshold to investigate if symptoms/signs VTE occur Think HIT if VTE (MI, stroke) occurs in patient who received heparin or LMWH Choose best thromboprophylaxis for: • 80 yo F obese post hip # surgery • 35 yo M appendectomy • 72 yo F for ovarian cancer resection, recent GI bleed • 68 yo for colon cancer resection; MVR with prior embolic TIA Gaps in knowledge • Chronically immobilized nursing home or rehab patients • Value of extended thromboprophylaxis after hospitalization for medical illness • Post C section thromboprophylaxis • Thromboprophylaxis after non- hip lower extremity fracture (e.g. ankle, tibfib)