Slides
advertisement
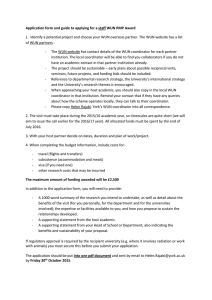
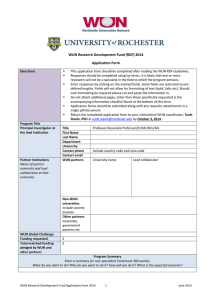
Yttrium-90 Radioembolization for Hepatocellular Carcinoma: Comprehensive Analysis of Long-term Outcomes in 291 Patients Robert J. Lewandowski, Ahsun Riaz, Robert K. Ryu, Ramona Gupta, Vanessa L. Gates, Kent T. Sato, Reed Omary, Riad Salem Northwestern Memorial Hospital Chicago, IL Disclosures Consultant, Advisory Boards, Research Support • MDS Nordion, Sirtex Medical Y90 Radioisotope • • • • • • 100% pure beta emitter, 0.9367 MeV Physical half-life of 64.2 h Irradiates tissue with average range of 2.5 mm Maximum penetration of approx. 1.0 cm A constituent of an insoluble glass matrix Microsphere diameter 25µ - 35µ Methodical Approach to Y90: 10 year experience • Investigated each concept – Safety – Angiographic Technique – Dosimetry – Niche Applications • Portal vein thrombosis • Radiation Lobectomy • Radiation Segmentectomy – Lung dose, Distribution – Liver Metastases • CRC • NET • Cholangiocarcinoma – – – – – Imaging criteria Pathologic analyses comparison with TACE Biomarkers Long term Survival Combination with Systemic Agents • Capecitabine • Sorafenib Northwestern 5-yr Experience 291-Patient Cohort • December 2003 December 2008 – Open label protocol: Y90 glass microspheres • All baseline CT/MR – 1250 CT/MRI scans, total 4.3 scans per patient – Strict imaging definition of metastases at baseline – Comprehensive review at each stage in time for development of metastases (CT chest, bone scans) – Prospectively followed all patients RECIST (Uni-dimensional) Guideline System Response Evaluation Criteria in Solid Tumors (RECIST) Classification Definition CR 100% decrease in maximum diameter of target lesion PR ≥30% decrease in maximum diameter of target lesion SD <30% decrease to ≤20% increase in maximum diameter of target lesion PD >20% increase from maximum response of target lesion Clinical Outcomes • TTP: Progression defined as any of the following: progression by WHO, EASL, UNOS stage or appearance of new lesions • Survival: from first treatment • Univariate (Kaplan-Meier with Logrank) and Multivariate (Cox Regression Model) were used Baseline Demographics N (%) Age (years) Gender Ethnicity < 65 138 (47) ≥ 65 153 (53) ≥ 75 63 (22) Male 223 (77) Female 68 (23) Caucasian 208 (71) African American 37 (13) Asian 29 (10) Hispanic 17 (6) Etiology N (%) Etiology HCV 100 (34) Alcohol 56 (19) Cryptogenic 54 (19) HBV 26 (9) HCV + Alcohol 23 (8) NASH 6 (2) Autoimmune 4 (1.3) Hemochromatosis 4 (1.3) HCV + HBV 3 (1) PBC 1 (0.6) Unknown 14 (5) Imaging Characteristics N (%) Distribution Tumor location Morphology Tumor Burden Solitary 78 (27) Multifocal 213 (73) Bilobar 139 (48) Unilobar 152 (52) Uninodular & <50% 73 (25) Multinodular & <50% 180 (62) Massive or >50% 38 (13) 0-25% 223 (76.6) 26-50% 48 (16) 51-75% 19 (7) 76-100% 1 (0.4) Imaging Characteristics N (%) PVT Metastases None 166 (57) Branch 58 (20) Main 67 (23) None 245 (84) LN 29 (10) Other 17 (6) Tumor Size N Mean (Range) Overall 291 7 (1.2-22) < 5 cm 116 (40) 3.4 (1.2-4.9) 5-10 cm 123 (42) 7.1 (5-10) > 10 cm 52 (18) 14.9 (10.1-22) Size Baseline Stage N (%) Child Pugh A 131 (45) B 152 (52) C 8 (3) A (n=39) BCLC A1 3 (1) A2 22 (8) A3 8 (2) A4 6 (2) B 66 (23) C 178 (61) D 8 (3) Treatment Characteristics Location Number of Treatments (N) Median dose (Gy) Mean dose (Gy) [Range] Liver 526 103 112 (18-1693) Lung (per treatment) 526 5.4 8.8 (0.09-89.9) Lung (cumulative) 291 9.3 15.7 (0.09-110) Clinical Toxicities Adverse Event No. of Patients % Fatigue 167 57 Abdominal Pain 67 23 Nausea/Vomiting 57 20 Anorexia 45 15 Fever/Chills 10 3 Diarrhea 7 2 Weight Loss 4 1 Liver-only disease Child’s Class PVT N EASL PR N (%) WHO PR N (%) TTP Median (95% CI) Overall Survival Median (95% CI) 116 (113) 78 (69) 59 (52) 10.8 (7.4-14) 17.2 (14.9-24) Overall 81 (79) 61 (77) 42 (53) 15.5 (10.7-25.9) 22.1 (17.2-32.5) T1/T2 27 (25) 22 (88) 13 (52) 27.1 (8, -) 20.5 (14.9-27.4) T3 27 (27) 24 (89) 17 (63) 21.9 (10.9-25.8) 35.7 (18.3-44.4) T4a 27 (27) 15 (56) 12 (44) 8.6 (6, -) 14.9 (7.3-22.2) T4b 35 (34) 17 (50) 17 (50) 5.6 (2.3-7.6) 10.4 (7.2-16.6) 122 (114) 59 (52) 44 (39) 8.4 (5.9-12.3) 7.7 (6.5-11.2) Overall 65 (64) 43 (67) 30 (47) 13.0 (8.4-18.1) 14.8 (11.8-29.1) T1/T2 22 (22) 15 (68) 8 (36) 13.0 (6.3-25) 29.1 (17.1, -) T3 21 (21) 18 (86) 12 (57) 17.4 (8.4-33.9) 38.3 (6.9-41.7) T4a 22 (21) 10 (48) 10 (48) 8.8 (3.6-18.1) 11.8 (6.2-19) T4b 57 (50) 16 (32) 14 (28) 5.9 (4.2-7.9) 5.6 (4.5-6.7) UNOS Overall CP A A PVT Absent PVT Present Overall CP B B PVT Absent PVT Present Northwestern 5-yr Experience 291-Patient Cohort • Significant findings: – 273/291 (94%) of patients had FU imaging – All as outpatients – 58% downstaged T3 T2 – 32 transplanted – No GI ulcers AFP 8.0 AFP 800 Pre treatment AFP 2200 6 months post treatment AFP 4.5 After 2 treatments Pre treatment 22 months Pre Tx: AFP 1368 36 months post Tx: AFP 9.5 Northwestern 5-yr Experience 291-Patient Cohort • Continues to be evolving role of Y90 in HCC • Cohort data permits – Exploratory subgroup analyses • • • • • Who benefits Who doesn’t Where should research be focused? Downstaged to potential cures (transplant/resection) Treatment in portal vein thrombosis patients • Next considerations – Y90 vs chemoembolization – Y90 +/- Sorafenib (various combinations) Acknowledgements Radiology: Robert Lewandowski Reed Omary Bob Ryu Kent Sato Paul Nikolaidis Frank Miller MR Physicists: Andrew Larson Post-Doc Fellows: Saad Ibrahim Ahsun Riaz Nurses: Karen Marshall Sharon Coffey Krystina Salzig Peggy Gilbertsen Jennifer Karp Elizabeth Gonda Hepatology/Oncology: Laura Kulik Mary Mulcahy William Small Al Benson Michael Abecassis Daniel Ganger Steve Flamm