PSA
advertisement
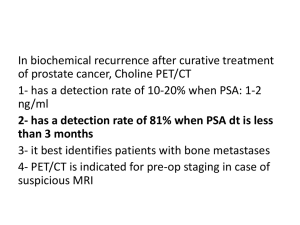
BENIGN PROSTATIC HYPERPLASIA DR .MOHAMMAD H DUMIRIEH 2014 DEFINTION Hyperplasia of stroma and epithelium in periurthral area of prostate (transition zone) Tone of prostatic smooth muscle plays role in addition to hyperplasia ETIOLOGY Etiology unknown Androgen dihydrotestosterone(DHT)required (converted from testosteron by 5-alpha reductase) Possiple role of impaired apoptosis, estrogen. other growth factors Epidemiology Age related,extremly common(50% of 50 year olds,80% of 80 year olds) 25 % of men will require treatment Clinical Feature Reslut from outlet obstruction and compensatory changes in detrusor function Voiding symptoms: .hesitancy,straining,weak/interrupted stream,incomplete bladder emptying .decreased flow rates may be seen on uroflowmetry. .due to out flow obstruction and/or impaired detrusor contractility. Clinical Feature storage symptoms: .urgency,frequency,nocturia,urgency incontinence .thought to be due to detrusor overactivity and decreased compiliance. Prostate is smooth ,rubbery and symmeetrically enlarged on DRE Complication: - Retention - Overflow incontinence - Hydronephrosis and renal compromise OVERFLOW Complication: - infection - gross hematuria - bladder stones AUA prostate symptom score funwise funwise frequency urgency nocturia Weak stream intermittency straining Emptying,incomplete feeling Each symptom graded out of 5 0-7 mildy symptomatic 8-19-moderately symptomatic 20-35 severely symptomatic Note: dysuria not included in score but is commonly associated with BPH Prostate size does not correlate well with symptoms in BPH APPROXIMATE PROSTATE SIZE 20cc-chestnut 25cc –plum 50cc-lemon 75cc-orange 100cc-grapefruit investigation history Assess LUTS and effect on quality of life ,may include self –administrede questionnires (AUA symptom and impact score) Physical exam:DRE Urinalysis to exclude UTI Creatinine to assess renal function +-renal ultra sound to assess for hydronephrosis. PSA to rule out malignancy (if life expectancy more than 10 y) investigation Uroflowmetry (optional) Bladder ultra sound post voiding urine(optional) Cystoscopy prior to potential surgical management. Biopsy if suspicious for malignancy TREATMENT Conservative for those with mild symptom: .watchful waiting-50% of patients improve spontaneously. .includes lifestyle changes(e.g evening fluid restriction,planned voiding) Medical treatment: .a-adrenergic antagonist-reduce stromal smooth muscle tone .5-a reductase inhibitor _block conversion of testosteron to DHT;acts on the epithelial component of prostate – reduces prostate size[e.g.finastride(proscar),dustride(avodart)] Transurethral resection of prostate(TURP) Objective To partially resect the periurethral area of prostate (transition zone)to decrease symptoms of urinary tract obstruction. Indications Obstructive uropathy (large bladder diverticula ,renal insufficiency) Refractory urinary retention Recurrent utis Recurrent gross hematuria Bladder stone Failure of medical therapy complication Acute: *intra or extraperitoneal rupture of bladder *rectal perforation *incontinence *hemorrhage *epididymitis *sepsis *trance urethral resection syndrome(post –TURP) .caused by absorption of large volume of hypotonic irrigation solution used ,usually through perforated venous sinusoid,leading to hypervolemic hyponatremic state. .characterized by: dilutional hyponatremia ,confusion,nausea,vomiting,hypertension,visual distrubance,pulmonary edema,bradycardia. .treat with diuresis and (if severe)hypertonic saline administration complication chronic: *retrograde ejaculation(>75%) *erectile dysfunction(5-10% risk increase with increasing use of cautery) *incontinence(<1%) *urethral stricture *bladder neck contracture. Open prostatectomy: .for large prostates or assochiated problems(e.g.bladder stones) .suprapubic (transvesically to deal with bladder pathology) .retropubic(through the prostatic capsule) Absolute indication for surgery Refractory urinary retention Recurrent utis Recurrent hematuria refractory to medical treatment Renal insufficiency (rule out other causes) Bladder stones Simple prostatectomy ALMOUSATE HOSPITAL Minimally invasive therapy .prostatic stent, microwave therapy , laser ablation, water –induced thermotherapy, cryotherapy, high intensity focoused ultra sound (HIFU), transurethral needle ablation (TUNA). Stent within prostate The passage way is wide and the lumen of bladder clearly seen Prostate specific Antigen(PSA) PSA Enzyme produced by epithelial cells of prostate gland to liquify the ejaculate Leaks into circulation and is present < 4ng/ml Measuerd total serum PSA is a combination of free(unbound)PSA (15%)and complexed PSA(85%) Screening Prostate cancer : PSA and DRE PSA may be elevated in prostate cancer and many other condition; not specific to cancer Population –based ,routine screening not recommended Must discuss risk factors,test characteristic , risk of over-detection and over treatment,treatment and active surveillance Well –informed patients can elect to undergo PSA and DRE The decision to proceed to prostate biopsy should be based primarily on PSA and DRE results,but should take into account multiple factors (free and total PSA,patient age,PSA velocity,PSA density,family history,ethnicity,prior biopsy history and comorbidities) AGE RANGE SERUM PSA (mg/L) 40-49 <2.5 50-59 <3.5 60-69 <4.5 70-79 <6.5 PSA is specific to the PROSTATE, but not to prostate cancer. In PSA testing , think “free and easy” : increased free/total ratio suggests benign cause of high PSA Causes of Increased PSA BPH,prostatitis,prosatic ischemia /infarction Acute urinary retention, prostate biobsy/surgery/ message Urethral catheteraization,TRUS Ejaculation ,acute renal failure Coronary bypass graft. Radiation therapy *free-to –total PSA ratio: Complexed PSA increases in prostate cancer,decreasing the percentage of the free fraction <10% free PSA suggestive of cancer ,>20% free suggest benign cause *PSA velocity: Change of >0.75ng/ml/year associated with increased risk of cancer *PSA density: PSA divided by prostate volume of as found on TRUS >0.15 ng/ml/ associated with increased risk of cancer Other Uses for PSA *Therapeutic decision making: patients with serum PSA level<10.0 are most likely to respond to local therapy *Work –up : bone scans are generally not necessary in patients with newly diagnosed prostate cancer who have a PSA <20 ng/ml unless the history or clinical examination suggests bony involvement Other Uses for PSA *Disease monitoring: serum PSA should fall to low level following radiation therapy,cryotherapy and should not rise on successive occasions. PSA should remain undetectable after radical prostatectomy Other Uses for PSA *Outcome prediction: in patients with metastatic disease receiving androgen suppresion therapy ,failur to achieve a PSA of<4.0 ng /ml seven months after initiation of therapy is associated with a very poor prognosis(median survival :one year) NOTE there is no easy , infallible method of determining when biopsies may be avoidable and when they are necessary.Until a perfect test is developed this determination must be made on the basis of clinical judgment and experience. NOTE Normal , hyperplastic, and neoplastic epithelial cells make PSA, but the amount of PSA produced by cancer cells is 10 times higher per gram of tissue than the amount by normal or hyperplastic tissue. NOTE Most PSA is produced in the hyperplastic transitional zone of prostate .A relatively small amount of PSA is produced in the peripherial zone,where 80% of prostate cancers orginate.cancers developing in the transitional zone tend to produce large amount of PSA. NOTE High-grade cancer cells tend to lose their ability to produce PSA. A GLEASON grade 5 prostate cancer produces less than a grade 3 cancer does. Some patients with advanced prostate cancer may have low or undetectable PSA level. THANK YOU