race/ethnicity incidence mortality
advertisement

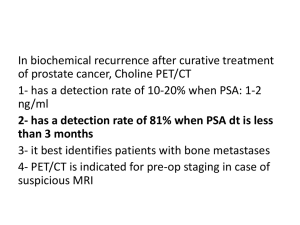
Radiation therapy for Early Stage Prostate Cancer John A. Kalapurakal MD Professor, Radiation Oncology Northwestern University Medical School Chicago, IL ARS 1-B It is estimated that 217,730 men will be diagnosed with and 32,050 men will die of cancer of the prostate in 2010 (SEER DATA) RACE/ETHNICITY INCIDENCE MORTALITY All Races 156.9 per 100,000 men 24.7 per 100,000 men White 150.4 per 100,000 men 22.8 per 100,000 men Black 234.6 per 100,000 men 54.2 per 100,000 men Asian/Pacific Islander 90.0 per 100,000 men 10.6 per 100,000 men American 77.7 per 100,000 Indian/Alaska Native men 20.0 per 100,000 men Hispanic 125.8 per 100,000 men 18.8 per 100,000 men Anatomy Risk stratification of Prostate Cancer • Low risk T1c-T2a and PSA<10 and Gleason score <6 • Intermediate risk T2b-T2c or PSA 10-20 or Gleason score 7 • High risk T3-T4 or PSA >20 or Gleason score 8-10 Low-risk Prostate Cancer • External beam RT: (x-rays, protons) – – • 70.2Gy-79.2Gy in 39-45 sessions (5 treatments/week, 8-9 weeks) 3D Conformal, Intensity Modulated RT, Protons Brachytherapy: I-125 (Iodine), Pd-103 (Palladium) – 144Gy in single session Intermediate-risk Prostate Cancer • External beam RT: (x-rays, protons) – – 75.6-79.2Gy in 42 sessions (5 treatments/week, 8-9 weeks) 3D Conformal, Intensity Modulated RT (IMRT), Protons • External beam RT + Short term Hormone therapy (6-8 months) • External beam RT + Brachytherapy: I-125 (Iodine), Pd103 (Palladium) – 45 Gy in 25 sessions (5 weeks) + brachytherapy (seeds, HDR) Image Guided RT (IGRT) • ALL MODERN RT DELIVERY SHOULD BE IGRT • Improve accuracy of treatment • Track daily position of the prostate before delivering RT • Fiducial markers (x-rays), ultrasound scans, electromagnetic tracking, CT scans (cone beam CT, fiducials), endorectal balloon (x-rays, CT scan) 3D conformal versus IMRT versus Protons Prostate Seed Implantation: Indications, Techniques and Outcomes Post Implant CT scan dosimetry Long-term results: Brachytherapy alone (Low-risk) and RT+Brachytherapy in intermediate-risk Prostate Cancer IJROBP 2010 IJROBP 2007 Higher RT dose (79.2Gy) resulted in higher PSA control in low and intermediate-risk prostate cancer without any increase in toxicity Low risk Intermediate-risk JCO 2010 Harvard Study: Adding 6 months of hormones to RT improved survival in intermediate-risk and high-risk disease Intermediate-risk High-risk IJROBP 2010 MD Anderson Study: Higher RT dose (78 Gy) for intermediate-risk patients resulted in better PSA control and cancer–specific survival IJROBP 2010 Low-intermediate risk Prostate Cancer: RTOG 94-08 Study • • • • • • • • T1b-T2b, PSA <20 RT: 66.6Gy + 4 months of hormone therapy 1979 patients randomized Overall survival significantly better RT+ hormones (51% vs. 4%) PSA control significantly higher with RT+ hormones in low and intermediate risk patients Subset analysis: survival benefit mainly for higher GS and PSA Final results awaited IJROBP 2009 Radiation-related Side Effects • Likely – – – • Less likely – – – • Increased urinary frequency, burning and urgency Increased bowel frequency, burning and urgency Fatigue Rectal bleeding, urinary bleeding Chronic bowel/bladder symptoms Temporary blockage of urination requiring a catheter Rare but serious – Permanent Rectal and Bladder injury requiring surgery Hormone-related Side Effects Conclusions – RT for Early Prostate Cancer • • • • • • Best Results: Higher tumor RT doses with improved technology treatments (Brachytherapy, IMRT, Proton therapy) Role of hormone therapy with RT in low and intermediate-risk patients remains to be defined Stereotactic Body Radiotherapy (SBRT): Cyberknife, Linear Accelerator, Tomotherapy Role of hypofractionated RT (70 Gy in 28 fractions, 50Gy in 5 fractions) ? Role of protons PATIENT’S CHOICE: Surveillance vs. Surgery vs. Radiation* vs. Seeds Radiation therapy for Early Stage Prostate Cancer John A. Kalapurakal MD Professor, Radiation Oncology Northwestern University Medical School Chicago, IL