Airway
advertisement

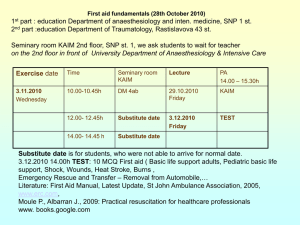
7: Airway Cognitive Objectives (1 of 5) 2-1.1 Name and label the major structures of the respiratory system on a diagram. 2-1.2 List signs of adequate breathing. 2-1.3 List signs of inadequate breathing. 2-1.4 Describe the steps in performing the head tilt-chin lift maneuver. 2-1.5 Relate mechanism of injury to opening the airway. 2-1.6 Describe the steps in performing the jaw-thrust maneuver. 2 Cognitive Objectives (2 of 5) 2-1.7 State the importance of having suction ready for immediate use when providing emergency care. 2-1.8 Describe the techniques of suctioning. 2-1.9 Describe how to artificially ventilate a patient with a pocket mask. 2-1.10 Describe the steps in performing the skill of artificially ventilating a patient with a bag-valvemask device while using the jaw-thrust maneuver. 3 Cognitive Objectives (3 of 5) 2-1.11 List the parts of the bag-valve-mask system. 2-1.12 Describe the steps in performing the skill of artificially ventilating a patient with a bag-valvemask device for one and two rescuers. 2-1.13 Describe the signs of adequate artificial ventilation using the bag-valve-mask device. 2-1.14 Describe the signs of inadequate artificial ventilation using the bag-valve-mask device. 2-1.15 Describe the steps in ventilating a patient with a flow-restricted oxygen-powered ventilation device. 4 Cognitive Objectives (4 of 5) 2-1.16 List the steps in performing the actions taken when providing mouth-to-mouth and mouth-tostoma ventilation. 2-1.17 Describe how to measure and insert oropharyngeal (oral) airway. 2-1.18 Describe how to measure and insert a nasopharyngeal (nasal) airway. 2-1.19 Define the components of an oxygen delivery system. 2-1.20 Identify a nonrebreathing face mask and state the oxygen flow requirements needed for its use. 5 Cognitive Objectives (5 of 5) 2-1.21 Describe the indications for using a nasal cannula versus a nonrebreathing face mask. 2-1.22 Identify a nasal cannula and state the flow requirements needed for its use. 6 Affective Objectives 2-1.23 Explain the rationale for basic life support, artificial ventilation, and airway protective skills taking priority over most other basic life support skills. 2-1.24 Explain the rationale for providing adequate oxygenation through high inspired oxygen concentrations to patients who, in the past, may have received low concentrations. 7 Psychomotor Objectives (1 of 4) 2-1.25 Demonstrate the steps in performing the head tiltchin lift maneuver. 2-1.26 Demonstrate the steps in performing the jawthrust maneuver. 2-1.27 Demonstrate the techniques of suctioning. 2-1.28 Demonstrate the steps in providing mouth-tomouth artificial ventilation with body substance isolation (barrier shields). 2-1.29 Demonstrate how to use a pocket mask to artificially ventilate a patient. 8 Psychomotor Objectives (2 of 4) 2-1.30 Demonstrate the assembly of a bag-valve-mask unit. 2-1.31 Demonstrate the steps in performing the skill of artificially ventilating a patient with a bag-valvemask device for one and two rescuers. 2-1.32 Demonstrate the steps in performing the skill of artificially ventilating a patient with a bag-valvemask device while using the jaw-thrust maneuver. 2-1.33 Demonstrate artificial ventilation of a patient with a flow-restricted, oxygen-powered ventilation device. 9 Psychomotor Objectives (3 of 4) 2-1.34 Demonstrate how to artificially ventilate a patient with a stoma. 2-1.35 Demonstrate how to insert an oropharyngeal (oral) airway. 2-1.36 Demonstrate how to insert a nasopharyngeal (nasal) airway. 2-1.37 Demonstrate the correct operation of oxygen tanks and regulators. 2-1.38 Demonstrate the use of a nonrebreathing face mask and state the oxygen flow requirements needed for its use. 10 Psychomotor Objectives (4 of 4) 2-1.39 Demonstrate the use of a nasal cannula and state the flow requirements needed for its use. 2-1.40 Demonstrate how to artificially ventilate the infant and child patient. 2-1.41 Demonstrate oxygen administration for the infant and child patient. 11 Additional Objectives* 1. Describe how to perform the Sellick maneuver (cricoid pressure). 2. Explain the rationale for applying cricoid pressure. 3. Demonstrate how to perform the Sellick maneuver (cricoid pressure). • These are noncurriculum objectives. 12 Anatomy Review 13 Breathing Process: Inhalation • Active part of breathing • Diaphragm and intercostal muscles contract, allowing the lungs to expand. • The decrease in pressure allows lungs to fill with air. • Air travels to the alveoli where exchange of gases occurs. 14 Breathing Process: Exhalation • Does not normally require muscular effort • Diaphragm and intercostal muscles relax. • The thorax decreases in size, and ribs and muscles assume their normal positions. • The increase in pressure forces air out. 15 The Body’s Need for Oxygen 16 Gas Exchange • Inhalation delivers oxygenrich air to alveoli. • Oxygen diffuses into the blood. • Breathing is primarily adjusted by the level of carbon dioxide in the blood. 17 Hypoxia • Not enough oxygen for metabolic needs • Develops when patient is: – Breathing inadequately – Not breathing 18 Signs of Hypoxia • Nervousness, irritability, and fear • Tachycardia • Mental status changes • Use of accessory muscles for breathing • Difficulty breathing, possible chest pain 19 Conditions Resulting in Hypoxia • Myocardial infarction • Chest injury • Pulmonary edema • Shock • Acute narcotic overdose • Lung disease • Smoke inhalation • Asthma • Stroke • Premature birth 20 Recognizing Adequate Breathing • Normal rate and depth • Regular pattern • Regular and equal chest rise and fall • Adequate depth 21 Normal Respiration Rates • Adults 12 to 20 breaths/min • Children 15 to 30 breaths/min • Infants 25 to 50 breaths/min 22 Recognizing Inadequate Breathing • Fast or slow rate • Irregular rhythm • Abnormal lung sounds • Reduced tidal volumes • Use of accessory muscles • Cool, damp, pale or cyanotic skin 23 Head Tilt–Chin Lift • Kneel beside patient’s head. • Place one hand on forehead. • Apply backward pressure. • Place tips of finger under lower jaw. • Lift chin. 24 Jaw-Thrust Maneuver • Kneel above patient’s head. • Place fingers behind angle of lower jaw. • Use thumbs to position the lower jaw. 25 Assessment of the Airway (1of 2) 26 Assessment of the Airway (2 of 2) • Assess whether breathing has returned using look, listen, and feel technique. – Listen by placing your ear about 10 inches above patient’s nose and mouth. – Feel and listen for movement of air. – Watch the patient’s chest and abdomen. – Place a hand on patient’s chest to feel for movement. 27 Severe Airway Obstruction • • • • There will be no movement of air. Chest and abdomen may rise and fall with patient’s attempts to breathe. Chest wall movement alone does not indicate breathing. Always use three-part approach: look, listen, and feel for movement of air. 28 Basic Airway Adjuncts (1 of 6) • Oropharyngeal airways – Keep the tongue from blocking the upper airway – Allow for easier suctioning of the airway – Used in conjunction with BVM device – Used on unconscious patients without a gag reflex 29 Basic Airway Adjuncts (2 of 6) Inserting an oropharyngeal airway 1. Select the proper size airway. 2. Open the patient’s mouth. 3. Hold the airway upside down and insert it in the patient’s mouth. 4. Rotate the airway 180° until the flange rests on the patient’s lips. 30 Basic Airway Adjuncts (3 of 6) 1 2 3 31 Basic Airway Adjuncts (4 of 6) • Nasopharyngeal airways – Conscious patients who cannot maintain airway – Can be used with intact gag reflex – Should not be used with head injuries or nosebleeds 32 Basic Airway Adjuncts (5 of 6) Inserting a nasopharyngeal airway 1. Select the proper size airway. 2. Lubricate the airway. 3. Gently push the nostril open. 4. With the bevel turned toward the septum, insert the airway. 33 Basic Airway Adjuncts (6 of 6) 1 2 3 4 34 Suctioning Equipment (1 of 2) 35 Suction Equipment (2 of 2) French, or whistle-tip, catheter 36 Suctioning Technique (1 of 2) • Check the unit and turn it on. • Select and measure proper catheter to be used. • Open the patient’s mouth and insert tip. • Suction as you withdraw the catheter. • Never suction adults for more than 15 seconds. 37 Suctioning Technique (2 of 2) 1 2 3 4 38 Recovery Position 39 Supplemental Oxygen • All patients in cardiac arrest should get oxygen. • Any patient with a respiratory or cardiac emergency needs oxygen. • Never withhold oxygen from anyone who may benefit from it. 40 Supplemental Oxygen Equipment • Oxygen cylinders – Available as a compressed combustible gas – Available in several sizes – Pin-indexing safety system – Oxygen regulators – Humidified oxygen 41 Oxygen Flowmeters • Pressure-compensated flowmeter – Affected by gravity; must be kept upright • Bourdon-gauge flowmeter – Not affected by gravity; can be used in any position 42 Using Supplemental Oxygen (1 of 2) • Inspect cylinder and markings. • “Crack” the cylinder. • Attach the regulator/flowmeter. • Open the cylinder. • Attach proper delivery device to flowmeter. 43 Using Supplemental Oxygen (2 of 2) • Adjust flowmeter to desired flow rate. • Apply the oxygen device to the patient. • When done, discard the delivery device. • Turn off the flowmeter. 44 Hazards of Oxygen • Oxygen supports combustion. • Keep possible ignition sources away from the area. • Oxygen tanks are under high pressure. 45 Oxygen Delivery Equipment • Nonrebreathing mask – Provides up to 90% oxygen – Used at 10 to 15 L/min • Nasal cannula – Provides 24% to 44% oxygen – Used at 1 to 6 L/min 46 Methods of Ventilation • Mouth to mask • Two-person BVM device • Flow-restricted, oxygen-powered device • One-person BVM device Bag-valve-mask 47 Rate of Artificial Ventilations Adult — 1 breath every 5-6 seconds Children — 1 breath every 3-5 seconds Infants — 1 breath every 3-5 seconds Bag-valve-mask 48 Mouth-to-Mask Technique (1 of 2) • Kneel at patient’s head and open airway. • Place the mask on the patient’s face. • Take a deep breath and breathe into the patient for 1 second. • Remove your mouth and watch for patient’s chest to fall. 49 Mouth-to-Mask Technique (2 of 2) 50 Bag-Valve-Mask Device • Can deliver more than 90% oxygen • Delivers less tidal volume than mouth-to-mask • Requires practice to be proficient • May be used with advanced airways 51 Bag-Valve-Mask Components 52 Two-Person BVM Technique (1 of 2) • Insert an oral airway. • One caregiver maintains seal while the other delivers ventilations. • Place mask on patient’s face. • Squeeze bag to deliver ventilations. 53 Two-Person BVM Technique (2 of 2) 54 One-Person BVM Technique 55 Flow-Restricted, Oxygen-Powered Devices 56 Ongoing Assessment of Ventilation • Adequate Ventilation – Equal chest rise and fall – Ventilating at appropriate rate – Heart rate returns to normal • Inadequate Ventilation – Minimal or no chest rise and fall – Ventilations too fast or slow – Heart rate does not return to normal 57 Sellick Maneuver • Also referred to as cricoid pressure. • Use on unconscious patients to prevent gastric distention. • Place pressure on cricoid with thumb and index finger. 58 Gastric Distention • Artificial ventilation fills stomach with air. • Occurs if ventilations are too forceful or too frequent or when airway is blocked • May cause patient to vomit and increase risk of aspiration 59 Stomas and Tracheostomy Tubes • Ventilations are delivered through the stoma. • Attach BVM device to tube or use infant mask. • Stoma may need to be suctioned. 60 Causes of Foreign Body Obstruction • Relaxation of the tongue • Vomited stomach contents • Blood clots, bone fragments, damaged tissue • Swelling caused by allergic reactions • Foreign objects 61 Recognizing an Obstruction (1 of 2) • Obstruction may be mild or severe. • Is patient able to speak or cough? • If patient is unconscious, attempt to deliver artificial ventilation. 62 Removing an Obstruction (2 of 2) • Perform Heimlich maneuver. • Use suction if needed. • If attempts to clear the airway are unsuccessful, transport rapidly. 63 Review 1. Breathing is controlled by an area in the: A. lungs. B. brain stem. C. spinal cord. D. diaphragm. 64 Review Answer: B Rationale: The pons and the medulla are the respiratory centers in the brain stem that control breathing. 65 Review 1. Breathing is controlled by an area in the: A. lungs. Rationale: The lungs contain small pockets called alveoli where the exchange of oxygen and carbon dioxide takes place. B. brain stem. Rationale: Correct answer C. spinal cord. Rationale: Impulses are sent down the spinal cord from the brain stem. D. diaphragm. Rationale: The diaphragm receives the impulses which cause it to contract and bring air in. 66 Review 2. The EMT-B should assess a patient’s tidal volume by: A. observing for adequate chest rise. B. assessing the facial area for cyanosis. C. counting the patient’s respiratory rate. D. measuring the patient’s oxygen saturation. 67 Review Answer: A Rationale: Tidal volume—the volume of air that is moved into or out of the lungs in a single breath—is assessed by observing for adequate chest rise. If shallow chest rise is noted, the patient’s tidal volume is likely reduced. 68 Review 2. The EMT-B should assess a patient’s tidal volume by: A. observing for adequate chest rise. Rationale: Correct answer B. assessing the facial area for cyanosis. Rationale: Cyanosis is an indication of hypoxia and not tidal volume. C. counting the patient’s respiratory rate. Rationale: Counting the respiratory rate gives you minute volume: the number of times a patient breaths in one (1) minute. The normal respiratory rate is 12 – 20 breaths/min for an adult. D. measuring the patient’s oxygen saturation. Rationale: Oxygen saturation is an indication of tissue perfusion, which is the amount of oxygen attached to the hemoglobin. 69 Review 3. In an otherwise healthy individual, the primary stimulus to breathe is a/an: A. increased level of oxygen in the blood. B. decreased level of oxygen in the blood. C. increased level of carbon dioxide in the blood. D. decreased level of carbon dioxide in the blood. 70 Review Answer: C Rationale: Under control of the brain stem, rising levels of carbon dioxide in arterial blood normally stimulate breathing in an otherwise healthy patient. In some patients with chronic lung disease, low levels of oxygen in the blood stimulate breathing; this is called the hypoxic drive. 71 Review 3. In an otherwise healthy individual, the primary stimulus to breathe is a/an: A. increased level of oxygen in the blood. Rationale: Increased levels of oxygen can be a result of Hyperventilation Syndrome. B. decreased level of oxygen in the blood. Rationale: This is typically not normal in healthy individuals. It can be a sign of inadequate breathing and results in hypoxia. C. increased level of carbon dioxide in the blood. Rationale: Correct answer D. decreased level of carbon dioxide in the blood. Rationale: This is usually not seen in healthy adults. It is typically 72a result of Hyperventilation Syndrome. Review 4. Signs of adequate breathing in the adult include all of the following, EXCEPT: A. pink, warm, dry skin. B. shallow chest rise. C. symmetrical chest movement. D. a respiratory rate of 16 breaths/min. 73 Review Answer: B Rationale: Signs of inadequate breathing in the adult include a respiratory rate less than 12 breaths/min or greater than 20 breaths/min, shallow chest rise (reduced tidal volume), cyanosis, and asymmetrical chest movement (both sides of the chest do not move equally). 74 Review 4. Signs of adequate breathing in the adult include all of the following, EXCEPT: A. pink, warm, dry skin. Rationale: This shows that breathing and perfusion are adequate. B. shallow chest rise. Rationale: Correct answer C. symmetrical chest movement. Rationale: This shows that the mechanical process of breathing is adequate, equal, and symmetrical bilaterally. D. a respiratory rate of 16 breaths/min. Rationale: This is a normal respiratory rate for an adult. 75 Review 5. A patient is found unconscious after falling from a third floor window. His respirations are slow and irregular. You should: A. place him in the recovery position. B. apply oxygen via nonrebreathing mask. C. suction his airway for up to 15 seconds. D. assist his breathing with a bag-mask device. 76 Review Answer: D Rationale: The patient is not breathing adequately. Slow, irregular respirations will not result in adequate oxygenation. You should assist the patient’s breathing with a bag-mask device attached to 100% oxygen. Suctioning is indicated if the patient has blood or other liquids in the airway; there is no evidence of this in the scenario. 77 Review 5. A patient is found unconscious after falling from a third floor window. His respirations are slow and irregular. You should: A. place him in the recovery position. Rationale: Due to a significant MOI, the patient will be placed supine on a long backboard with the head immobilized. B. apply oxygen via nonrebreathing mask. Rationale: A BVM device is indicated if the patient’s respirations are less than 12 breaths/min. C. suction his airway for up to 15 seconds. Rationale: Suction is indicated if a patient has blood or other secretions in the airway. D. assist his breathing with a bag-mask device. Rationale: Correct answer 78 Review 6. When ventilating an apneic adult with a bag-mask device, you should squeeze the bag: A. until it is empty. B. over a period of 2 seconds. C. at a rate of 20 breaths/min. D. until visible chest rise is noted. 79 Review Answer: D Rationale: When ventilating any apneic patient with a bag-mask device, you should squeeze the bag over a period of 1 second and observe for visible chest rise. Ventilate the apneic adult at a rate of 10 to 12 breaths/min (one breath every 5 to 6 seconds). Ventilate infants and children at a rate of 12 to 20 breaths/min (one breath every 3 to 5 seconds). 80 Review 6. When ventilating an apneic adult with a bag-mask device, you should squeeze the bag: A. until it is empty. Rationale: An appropriately sized bag for an adult will not totally empty. B. over a period of 2 seconds. Rationale: You should squeeze the bag over a period of 1 second. C. at a rate of 20 breaths/min. Rationale: Ventilate the apneic adult at a rate of 10 to 12 breaths/min (or one breath every 5 to 6 seconds). D. until visible chest rise is noted. Rationale: Correct answer 81 Review 7. During insertion of an oropharyngeal airway into an unconscious patient, she begins to vomit. Immediately the first thing you should do is: A. turn the patient on her side. B. remove the airway at once. C. suction the patient's mouth. D. use a smaller sized oral airway. 82 Review Answer: A Rationale: Any time an unconscious patient begins to vomit—whether you are inserting an oropharyngeal airway or not—you should immediately turn the patient onto his or her side; this will allow drainage of vomit from the mouth and prevent aspiration. After the patient is on his or her side, remove the oral airway and suction the mouth. 83 Review 7. During insertion of an oropharyngeal airway into an unconscious patient, she begins to vomit. Immediately the first thing you should do is: A. turn the patient on her side. Rationale: Correct answer B. remove the airway at once. Rationale: Remove the airway after the patient has been rolled onto his or her side. C. suction the patient's mouth. Rationale: This must be completed after the patient is positioned and the airway is removed. D. use a smaller sized oral airway. Rationale: Oropharyngeal airways are contraindicated if the patient has a gag reflex. 84 Review 8. You are delivering oxygen to a patient with a nasal cannula at 4 L/min when he begins to complain of a burning sensation in his nose. You should: A. remove the nasal cannula. B. apply a nonrebreathing mask. C. attach an oxygen humidifier. D. increase the flow rate to 6 L/min. 85 Review Answer: C Rationale: Administering “dry” oxygen through a nasal cannula—especially over a prolonged period of time— can result in drying of the nasal membranes, in which the patient might complain of a burning sensation in the nose. Humidified oxygen will serve to keep the nasal membranes moist. 86 Review 8. You are delivering oxygen to a patient with a nasal cannula at 4 L/min when he begins to complain of a burning sensation in his nose. You should: A. remove the nasal cannula. Rationale: The oxygen should be humidified. B. apply a nonrebreathing mask. Rationale: This can still cause an irritation due to providing “dry” oxygen. C. attach an oxygen humidifier. Rationale: Correct answer D. increase the flow rate to 6 L/min. Rationale: The oxygen should be humidified. 87 Review 9. In which of the following patients would a nasopharyngeal airway be contraindicated? A. A semiconscious patient with a gag reflex B. An unconscious patient with an intact gag reflex C. A patient who fell 20' and landed on his or her head D. An unconscious patient who gags when you insert an oral airway 88 Review Answer: C Rationale: Nasopharyngeal (nasal) airways are contraindicated in patients with severe head or facial injuries and should be used with caution in patients who have delicate nasal membranes or are prone to nosebleeds. The nasal airway is better tolerated in patients who are semiconscious and/or those with a gag reflex. 89 Review 9. In which of the following patients would a nasopharyngeal airway be contraindicated? A. A semiconscious patient with a gag reflex Rationale: This airway works best with an intact gag reflex. B. An unconscious patient with an intact gag reflex Rationale: This airway works best with an intact gag reflex. C. A patient who fell 20' and landed on his or her head Rationale: Correct answer D. An unconscious patient who gags when you insert an oral airway Rationale: This airway can be used when the patient gags with an oral airway. 90 Review 10. You and your partner are ventilating an apneic adult when you notice that his stomach is becoming distended. You should: A. suction his airway for up to 15 seconds. B. reposition his head and use cricoid pressure. C. increase the rate and volume of your ventilations. D. decrease your ventilation rate but use more volume. 91 Review Answer: B Rationale: Gastric distension occurs when air enters the stomach. Severe gastric distention can result in vomiting and aspiration if not recognized and treated. To minimize the amount of air that enters the stomach during ventilations, you should reposition the patient’s head and use cricoid pressure (Sellick maneuver). 92 Review 10. You and your partner are ventilating an apneic adult when you notice that his stomach is becoming distended. You should: A. suction his airway for up to 15 seconds. Rationale: Suctioning is indicated when there is blood or secretions in the airway. B. reposition his head and use cricoid pressure. Rationale: Correct answer C. increase the rate and volume of your ventilations. Rationale: This action may only result in more air going into the stomach. D. decrease your ventilation rate but use more volume. Rationale: This action may only result in more air going into the stomach. 93