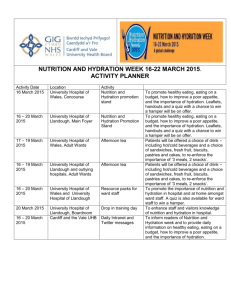
View Putting Human Rights at the Heart of Hydration and Nutrition
advertisement

Human Rights in Healthcare Betsi Cadwaladr University Health Board Anne-Marie Rowlands: Deputy Director of Nursing Sally Hughes-Jones: Head of Equality and Human Rights Julie Smith: Associate Chief of Staff Nursing About BCU Health Board Largest health organisation in Wales Primary, community, mental health & acute hospital services for a population of around 676,000 Workforce around16,000 staff Budget around £1.2 billion Acute and Community services 3 district general hospitals 22 other acute and community hospitals 90 health centres, clinics, community health team bases and mental health units 121 GP practices and NHS services provided by North Wales’ dentists, opticians and pharmacies. Our Strategic Direction “Anyone coming in contact with a public service should be treated with respect and dignity, have their health need assessed, be helped and not handed off to someone else, receive a responsive, safe and high quality service that continually improves, is easy to access and understand” (Strategic Directions 2009) Our Positive Obligation Positive obligations on public authorities to take a proactive approach to human rights. FREDA principles (Fairness, Respect, Equality, Dignity, Autonomy) underpin Human Rights and public service ethos. Supports BCU Strategic Equality Plan & our organisational values Human Rights Based Approach Empowers service users and staff Protects vulnerable people Improves experience Improves outcomes Bring human rights to life by applying the principles to a clinical pathway Leading & Defining the Project Championed at Board level by the Director of Nursing, Midwifery and Patient Services Deputy Director of Nursing, whose portfolio includes nutrition Head of Equality and Human Rights Associate Chief of Staff Nursing, lead for transformational group Why Human Rights, Nutrition and Hydration? Patient Association, Care Quality Commission, Ombudsman, Age Concern No specific guidance – direct link nutrition, hydration, human rights & obligations of service providers Evidence, guidance and best practice BCU – huge organisation – different ways of working Quality Patient Care Ward staffing/ nurse : patient ratio review Supernumerary ward sisters/charge nurses Introduction of matrons Strategic nutritional and catering group Saving 1000 Lives – Intentional rounding Striving for excellence– ‘good is not good enough’ Project Aims Development of a practical toolkit Directly links nutrition, hydration, human rights & obligations of service providers Increase knowledge and awareness of human rights, nutrition and hydration Embed dignity and human rights within everyday ward routine Place the patient at the centre of care. Achieving the Aims Multidisciplinary project steering group Redefined the role of nutritional sub group BIHR Human Rights training Brainstorming session - practical starting point Project plan & driver diagram agreed Draft toolkit developed Engagement and Involvement Communication & press briefing Stakeholder event - ward staff, dietetics, Speech and Language, education, catering, service users, specialist nurses BIHR training, questionnaire, workshop Draft toolkit –questions posed – positives and negatives? what would you change? barriers to implementation? Outcome of Stakeholder Event Event ideas and feedback discussed Changes to toolkit made 6 pilot wards identified (mix of acute medical, care of the elderly, acute surgical, acute orthopaedic) BIHR training for pilot wards, matrons and senior nursing team Transformational sub group Reporting to Human Rights steering group Monthly meetings Leads identified to support pilot wards Focus on establishing the baseline, identifying areas for change Testing (and changing) the toolkit Drivers to Succeed Over arching aim Primary Driver (Patients receive the required level of support with eating & drinking) Secondary Drivers (Safety, Environment etc.) Interventions Cornerstone of the toolkit Drivers & Key Components of Nutrition & Hydration in relation to Ward Routine Safety Identify vulnerable patients and those at risk at the beginning of every shift. Establish an alert system. Environment Ensure appropriate environment of care including access to equipment. Putting Human Rights at the Heart of Hydration and Nutrition Empower patients and their families. Ensure and enable regular communication. Ensure patients autonomy and dignity is respected. Audit compliance and measure improvement MUST audit and fundamentals of care audits. Identify, monitor and learn from concerns. Choice Enable and promote choice and ensure 24 hour access to food and drinks. Meal times Ensure mealtimes are protected. Enable and promote appropriate involvement of carers and volunteers Principles of Improvement Methodology Initiative to improve patients nutrition and hydration in various areas of practice using PDSA cycle methodology with fast cycling Measure it > change it > re-measure it > change it Until you get it right! Aims to introduce effective processes and systems for staff in ward environments Aims for culture change! Methodology Human Rights Strategic Group In Patient Transformational Group East Patient Safety & Empowerment Central Patient Choice Measurements West Mealtimes & Environment How did we do it ? East pilot areas Patient safety and empowerment work streams in line with improvement methodology Wards and teams identified Operational definitions for measurements developed Baseline measurements undertaken PSDA cycles - process redesign We stacked the odds in our favour!! Patient Safety 3 dimensions of patients safety Identification of patients at risk during safety briefing (measure 1) (Safety briefing – measure 2) Delegation of Nursing orders (measure 3) Methodology Baseline measurement on pilot ward showed identification of patients at risk at safety briefing at 59% Target compliance = 95% Methodology (2) Changes introduced Raise awareness of human rights approach and toolkit development – matrons meeting/staff meetings All Wales e learning directive for all nurses to complete Posters for SBAR Symbols Letters to nurses in charge outlining roles and responsibilities Red jugs/lids At a glance board Roles and responsibilities e.g. For house keepers for data collection, Change ward routine in relation to undertaking distribution of red jugs/symbols Example of reliable design evolution Implement a system to ensure patients at risk are identified at safety briefs Who - All team leaders What – ensure at risk patients are identified at safety briefing When – during safety briefings (3x daily) Where - Pilot ward How Design – brief the nurses regarding responsibilities of identifying patients at risk Redesign – re introduce safety briefing into ward 3 times daily Redesign – develop a poster to be clearly displayed at nurses station prompting safety brief times Redesign - change the pm SB time to accommodate shift patterns Redesign – introduction of symbols relating to patients at risk Reliable Process Design AM ....... Don’t forget Don’t Forget Safety Briefing PM …… Nights …….. Results – weekly data Results – monthly data Introduced symbols/posters Re affirmed R&R No SB (nights) Delegation of need Empowerment Conclusion Through repeated testing and process redesign, reliability and sustainability achievable Lessons learnt – At the beginning state who, what, where and when (prevents defects being the people you forgot to include! Keep it simple Spread only when processes reliable Next Steps Project steering group meeting Dec 12 Agree implementation plan Development of ward resource file/website Communication within organisation Strategic Nursing and Midwifery Committee Improving Service User Experience Committee Evaluation of impact Sharing across Wales and wider Thank You Our contact details: Anne-Marie.Rowlands@wales.nhs.uk Sally.HughesJones@wales.nhs.uk Julie.Smith@wales.nhs.uk