Anemia - MCE Conferences
advertisement

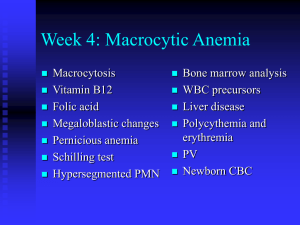
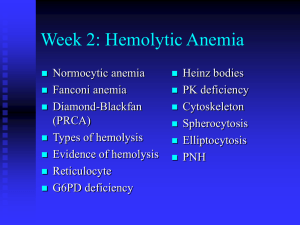
Anemia A Finding, Not Yet a Diagnosis Herbert L. Muncie, Jr., M.D. Case Finding – Symptoms or Signs Order CBC if suspect anemia due to: Symptoms Fatigue, weakness, blood loss, etc. Signs on Physical exam Look for pallor of conjunctivae, face & palms - if all 3 present helps confirm anemia Absence of pallor does not rule out anemia Pallor of nail beds/skin creases - of no value in assessing presence or absence of anemia When to order a CBC CBC is not a screening test for nonpregnant adults Who should be screened? Pregnant patients & high risk infants (USPSTF) – (SOR – B) infants 6 – 12 months of age – insufficient evidence for or against (SOR – I) Asymptomatic Against is low prevalence, cost & toxicity of Fe Diagnosing Anemia Diagnosis depends on Hgb/Hct being below a normal value The “normal” Hgb and Hct changes Throughout childhood During pregnancy Higher for men than women Normal does not imply optimal And we do not know what the optimal level is for a patient Normal Adult Red Cell Values Red Cell Parameter Adult male Adult Female Hemoglobin (g/dL) 13.0 - 17.2 11.6 - 15.1 Hematocrit (%) 41 - 50 36 - 44 Reticulocytes (%) 0.5 - 2.0 0.5 - 2.0 Mean corpuscular volume (fl) (MCV) 80 - 100 80 - 100 11.5 - 14.5 11.5 - 14.5 Red cell distribution width (%) (RDW) Question 52 year old white male, 2 PPD smoker, had a CBC done for mild fatigue & dyspnea on exertion WBC – 8.7 Hgb – 13.0 g/dL Hct – 41% MCV 81 fl Is this patient anemic? a) b) c) Yes No Maybe Adjustments to normal range Adjust for altitude Adjust for smoking > 3,000 feet - lower oxygen tensions, higher values Smokers have higher values due to carbon monoxide in smoke Adjust for ethnicity Smoking adjustments for Hgb/Hct Characteristic Hct (%) Non-smoker Hgb (g/dL) 0.0 All smokers +0.3 +1.0 1/2 - 1 pk/d 1 - 2 pks/d > 2 pks/d +0.3 +0.5 +0.7 +1.0 +1.5 +2.0 0.0 Add this to the normal Hgb/Hct range - e. g. • normal male non-smoker Hct = 41 - 50% • > 2 PPD male smoker normal Hct = 43 - 52% Ethnicity adjustment – Average Normal level 14 13.5 13 White Men 13.7 African American Men White Women 13.2 12.9 12.7 12.5 12.2 12.2 12 11.5 11.5 11.5 11 Men Age 20 - 59 Men Age Women 60+ Age 20 - 49 Women Age 60+ African American Women Question 52 year old male, 2 PPD smoker, had a CBC done for mild fatigue & dyspnea on exertion WBC – 8.7 Hgb – 13.0 g/dL Hct – 41% MCV 81 fl Is this patient anemic? a) b) c) Yes No Maybe 1st Diagnostic Step after finding anemia Once you determine the patient is ‘anemic’ then look next at MCV to determine diagnostic tests (if WBC & platelets are normal): MCV Anemia category < 80 fl Microcytic 80 – 100 fl Normocytic > 100 fl Macrocytic If you suspect blood loss or hemolysis Order Reticulocyte count (RC) Normal < 2% - marrow’s response to anemia Hemolytic anemia usually > 4% Absolute: RC% X RBC/100 Normal - 25K-75K > 75K suggests blood loss or hemolysis Corrected: RCc = RC% X hct/45 Normal RCc = 0.5 - 1% > 1% suggests blood loss or hemolysis Anemia - other testing if indicated Haptoglobin Low in hemolysis LDH High in hemolysis Hemoglobin electrophoresis Hemoglobinopathies Thalassemia Most Common Diagnoses based on MCV Microcytic Normocytic Macrocytic Iron deficiency* Chronic disease* Folate defic.* Thalassemia* Blood loss acute B12 defic.* Lead poisoning Liver disease (alcohol abuse) Sideroblastic Hypothyroid * Discussed in more detail Iron Balance Controlled by absorption, not excretion Routine loss about 1 mg/day Menstrual loss averages 30 mg/month or on average 1 mg/day Normally absorb 1.5 - 3.0 mg/day Delicate balance for menstruating females Pica - Inappropriate consumption of nonnutritive substances (e.g. clay, starch, ice) Highly characteristic of iron deficiency Microcytic Anemia - Iron Deficiency Definition: anemia occurs after iron stores are totally depleted Etiologies: inadequate diet to meet demand, blood loss or both • Children, teens - inadequate diet • Young women – blood loss (menorrhagia) &/or inadequate diet • Older person • Neoplasm - always exclude cancer • GI loss - may be due to medication (esp. NSAIDs) • Angiodysplasia Iron Sources – Dietary Sources Heme Iron: Meat, poultry, fish Efficiently absorbed & minimally affected by dietary factors Non-heme Iron: Green leafy vegetables Less efficiently absorbed – requires acid digestion Ascorbic acid increases absorption Reduced absorption with calcium, tea, coffee Iron Deficiency Anemia (IDA) consequences Impaired attention Learning disabilities Altered immunity Reduced work capacity Pre-term labor Reduced athletic performance Reasonable indications for CBC Tests to Diagnose IDA MCV - changes occur late < 70 fL probably iron deficiency MCH, MCHC - no clinically useful information RDW % - reflects anisocytosis Almost always elevated in IDA – 90% However, about 50% of patients with thalassemia trait have elevated RDW MCV & iron deficiency anemia (IDA) Result (fL) Probability of IDA < 70 84.3% 70 -74 58.6% 75 -79 30% 80-84 28.1% 85 -89 24.6% > 90 11.1% Tests for Fe Deficiency Serum iron - level alone of little value Low in anemia of chronic disease Total Iron binding capacity (TIBC) - high in Fe deficiency Usually low in anemia of chronic disease Question 38 year old female with type 2 diabetes develops pyelonephritis & is hospitalized CBC – Hgb 11.0 g/dL, Hct 33%, MCV 79 fl Ferritin is ordered – result is 115 ng/ml You wonder if the elevated ferritin is the result of inflammation/infection or does it mean she does not have iron deficiency. What would you order to determine which it is? a) b) c) d) Serum iron Total iron binding capacity C-reactive protein (CRP) Transferrin saturation Tests - Ferritin Intracellular iron storage protein Best single test to assess for Fe deficiency Levels < 15 µg/L – diagnostic of Fe deficiency Levels > 100 µG/L - Fe deficiency very unlikely However, it is an acute phase reactant Can be elevated in inflammatory, malignant or liver disease & would not reflect Fe stores If C-reactive protein (CRP) is normal then inflammation is not causing the increased ferritin [Yang 2008] Ferritin and likelihood IDA Result Probability of IDA < 15 ng/ml 95.7% 15 - 24 ng/ml 79.1% 23 - 34 ng/ml 52.1% 35 - 44 ng/ml 44% 45 - 100 ng/ml 18.8% > 100 ng/ml 3.3% Additional Tests for Fe Deficiency Transferrin saturation Decreased in iron deficiency Soluble transferrin receptor assay (sTfR) Excellent for distinguishing between inflammation & iron deficiency sTfR is increased with iron deficiency sTfR is not affected by inflammation Normal with inflammation However, not available in all labs & expensive Transferrin saturation & iron deficiency Result Probability of disease < 5% 81.8% 5 - 9% 51.7% 10 - 19% 25.8% 20 - 29% 18.2% 30 - 49% 15.6% > 50% 6% Additional Tests for Fe Deficiency Bone Marrow Gold standard - any stainable iron excludes diagnosis No single biochemical test consistently diagnoses IDA except bone marrow aspirate 21 year old female with fatigue, found to have Hgb/Hct of 9.7/30.6. MCV – 76 Has heavy menses. This patient probably has iron deficiency anemia. How would you tell this patient to take her iron salt? a) b) c) d) Once daily (QD) Twice a day (BID) Three times a day (TID) As tolerated by the patient Iron Deficiency - therapy Do not give iron unless it is iron deficiency anemia & the etiology is determined Should have a probable etiology Treat with ferrous salts Sulfate (325 mg = approximately 60 mg elemental Fe) Gluconate (325 mg = approximately 36 mg elemental Fe) Sustained release forms not recommended as initial therapy Iron Deficiency - therapy Start once daily (QD), may increase to BID or TID with meals if needed & tolerated QD adequate in children, elderly & pregnancy if not actively bleeding More GI distress with more frequent doses Continue for 6 - 12 months to replete iron stores Hgb should increase 1 g/dL every 2 - 3 weeks or 2 g/dL within 4 weeks Serum ferritin > 100 µg/dL indicates appropriate iron stores Iron Deficiency - IV therapy Indications for IV therapy Chronic uncorrectable bleeding Intestinal malabsorption Intolerance to oral iron Nonadherence to oral therapy Hgb < 6.0 g/dL with poor perfusion who would otherwise have received transfusion but refused Iron Deficiency - IV therapy Iron dextran (Dexferrum®, INFeD®) 25 - 100 mg IM/IV Risk of anaphylaxis Ferumoxytol (Feraheme®) For patients with chronic kidney disease & IDA 510 mg IV x1 & repeat in 3 - 8 days Iron Deficiency - IV therapy Newer agents with less risk of anaphylaxis Sodium ferric gluconate complex (Ferrlecit® 125 mg IV each HD) Iron sucrose (Venofer® - 100 mg IV each HD) Primary indications for both drugs are chronic kidney disease or hemodialysis Heart failure & iron deficiency Patients with heart failure prone to iron deficiency from: Depletion iron stores – poor nutrition Defective iron absorption IV ferric carboxymaltose improved symptoms, functional capacity & QOL with or without anemia [Anker 2009] Criteria – ferritin < 100 mcg/L or ferritin 100 – 299 & transferrin saturation < 20% Hgb 9.5 – 13.5 g/dL Unknown if oral therapy would help Microcytic Anemia – Thalassemia Hereditary microcytic anemia [Muncie 2009] Autosomal recessive inheritance Defect in hemoglobin synthesis synthesis of α-globin chains α-thalassemia Reduced Controlled by two genes on each chromosome 16 synthesis of -globin chains -thalassemia Reduced Controlled by one gene on each chromosome 11 α-Thalassemia One of four gene deletions Two of four gene deletions α-thalassemia trait Three of four gene deletions α-thalassemia silent carrier α-thalassemia intermedia with significant Hb H (Hb H disease) Four gene deletions α-thalassemia major with significant Hb Bart’s α-Thalassemia - diagnosis No definitive test for α-thalassemia Hemoglobin electrophoresis normal in adults In infants if electrophoresis showed: Hb H – patient has α-thal Hb Bart’s – usually fatal due to hydrops fetalis α-Thalassemia - treatment No treatment necessary or helpful Suggest genetic counseling & possible prenatal diagnostic testing -Thalassemia One gene defect results -thalassemia Two trait (minor) gene defect Mild to moderate decrease in synthesis -Thalassemia intermedia Severe decrease in synthesis -Thalassemia major -Thalassemia Trait - diagnosis Usually Mild found incidentally when: microcytic anemia with normal RDW Normal RDW almost always β-thal trait RDW can be elevated in 50% patients If RDW is elevated additional tests are needed Ferritin to r/o iron deficiency Lead level to r/o lead poisoning Finally hemoglobin electrophoresis can help Reduced or absent Hb A, elevated levels HbA2 (> 3.5%) and elevated Hb F -Thalassemia Trait - treatment No disease specific treatment available Adjunctive treatment not needed for most cases Diagnosis has genetic ramifications Suggest prenatal screening -Thalassemia intermedia/major Diagnosed during infancy or early childhood Will need chronic blood transfusions to survive With chronic transfusions will get iron overload Will eventually require iron chelation therapy Mortality due usually to cardiac iron overload 72 y. o. female with diabetes & hyperlipidemia had a CBC for pre-op evaluation for cataract surgery. HGB – 10.1; HCT -30.8, MCV – 89 fl. This patient probably has:? a) b) c) d) Iron deficiency anemia Anemia of chronic disease Pernicious anemia Anemia from folate deficiency Anemia of Chronic Disease (ACD) Most common outpatient etiology of normocytic anemia Misnomer - can be seen in acute illness Another name - anemia of chronic inflammation Occurs in infection/inflammation/neoplasia and unknown other conditions Anemia can be first clue to disease Without known disease - pursue further evaluation Evaluation for occult chronic disease ESR TSH LFTs BUN & creatinine If normal PE & lab tests No further workup is likely to be helpful Associated diseases Acute infections Chronic infections E. g TB, endocarditis, chronic UTI, coccidiomycosis Inflammatory diseases E. g. bacterial, fungal, viral E. g. Osteoarthritis (OA), rheumatoid, collagenvascular, PMR, hepatitis, decubitus ulcers Malignancy Protein-energy malnutrition Anemia of Chronic disease (ACD) Hematology: Usually mild anemia (Hct 30 – 34%) Normochromic/normocytic May be complicated by true iron deficiency anemia But would be microcytic or have elevated RDW Pathogenesis of ACD Pathogenesis: Inflammatory cytokines i.e. interleukin 1, tumor necrosis factor (TNF) mediate etiology Sequester iron in RE system Impair proliferation of erythroid progenitor cells Blunt erythropoietin response Anemia of Chronic disease Patients have impaired release of Fe from RE cells Increased Fe stores, not Fe deficiency Results in Ferritin level - normal Serum iron & transferrin saturation - low Transferrin level – normal or decreased True for both ACD & IDA IDA - increased Low reticulocyte count Diagnosis of ACD Diagnosis: Measure transferrin receptor level if unclear Raised in Fe deficiency Normal in anemia of chronic disease Female – 1.9 - 4.4 mg/L – normal range Male – 2.2 - 5 mg/L – normal range Anemia of Chronic disease Treatment: Anemia resolves if correct underlying disorder If cannot correct underlying disorder treatment of anemia is not usually indicated Supplements of Fe, vitamin B12 or folate are of no benefit Anemia of Chronic disease Treatment: If quality of life is impaired, you can increase the Hgb and Hct with either: Transfusion If severe or life-threatening anemia Erythropoietin Approved for cancer with chemotherapy; chronic renal disease; HIV infection with myelosuppressive therapy Good data on short-term outcomes Little data on effect on course of underlying disease Anemia of Chronic disease Treatment: Iron supplements of no benefit unless Patient has ACD & absolute iron deficiency ferritin < 100 ng/ml If ferritin > 100 ng/ml supplements associated with adverse outcomes Macrocytic anemia Typically presents with MCV > 110 fL MCV 100-110 common, often unexplained with no specific diagnosis found Consider evaluation even if not anemic Occult B12 deficiency? Spurious macrocytosis can occur with cold agglutinins, hyperglycemia, leukocytosis Etiologies B12 [cyanocobalamin (Cbl)] deficiency Folate deficiency Hypothyroidism Hepatic dysfunction (alcoholism) Macrocytic anemia – Diagnostic Evaluation Vitamin B12 & folate levels RBC folate level is more accurate if folate deficiency is suspected [Kaferle 2009] RBC folate better reflects long-term stores Nl = 160-700 ng/ml Serum folate more easily affected by recent dietary intake Nl = 2.7 – 17 ng/ml Consider ordering only a B12 level since if normal could just treat with folate without worrying about complications Macrocytic anemia – Diagnostic Evaluation Other tests as indicated TSH; Free T4; Free T3 Liver function tests (LFTs) Folate level with Vitamin B12 Deficiency Folate level usually increased with B12 deficiency If both levels are low – is it a mixed deficiency? Low folate level can cause low B12 level If both results are low, treat the patient with folic acid & repeat B12 level in 4 weeks If B12 then is normal, do not need to treat with B12, just continue to give folate If B12 remains low either treat with B12 or measure MMA level Cbl Deficiency Level < 100 pg/ml confirms deficiency Levels > 400 pg/ml rules out deficiency With levels > 100 & < 400 pg/ml Measure methylmalonic acid (MMA) – normal < 0.4 μmol/L Elevated only in Cbl deficiency If MMA normal – points to folate deficiency Etiologies B12 Deficiency Inadequate nutritional intake Unless strict vegetarian, Cbl deficiency implies reduced absorption Reduced absorption Loss of intrinsic factor; achlorhydria Pernicious anemia (PA) Drugs, gastro-duodenal surgery etc. Takes 2-5 years to develop deficiency even with severe malabsorption Occult B12 Deficiency Anemia can be absent in early Cbl deficiency Especially with Cbl level < 350 pg/mL Consider occult deficiency with new neurologic or psychiatric symptoms Most common psychiatric symptoms are depression, mania, psychotic symptoms, OCD behavior & cognitive impairment 72 year old female with H/H 9.2/28.1 & MCV – 112 fl. Diagnosed with pernicious anemia. I would treat this patient with: a) Monthly injections of B12 for life b) Quarterly injection of B12 for life c) Daily oral B12 for life d) Monthly injections of B12 for one year Treatment of B12 Deficiency Oral therapy equal to IM therapy short-term Oral 2000 µG qd equally effective to IM for hematologic results [Butler 2006] ($100/year) Passive diffusion accounts for 1-2 % of total absorbed & is unaffected in pernicous anemia or gastro-duodenal resection Long-term data not available for oral therapy Cost of medications equal, difference is medical personnel costs 1000 µG IM q month ($70/yr) or 1 mg IM q 3 months Treatment of B12 Deficiency Nasal vitamin B12 for maintenance after stores repleted & without nervous system involvement (approximately $500/year) Duration of therapy Life-long unless reversible cause identified No evidence of harm associated with elevated B12 levels 72 year old female with H/H 9.2/28.1 & MCV – 112 fl. Diagnosed with pernicious anemia. I would treat this patient with: a) Monthly injections of B12 for life b) Quarterly injection of B12 for life c) Daily oral B12 for life d) Monthly injections of B12 for one year Etiologies Folate Deficiency Inadequate nutritional intake Especially with alcohol dependence Medications Seizure medications Chemotherapy Reduced absorption Metformin (Glucophage®) Cholestyramine (Questran®) Treatment of Folate Deficiency 1 mg orally every day CAUTION - folate may correct anemia of B12 deficiency but not the neurologic sequelae Before initiating folate therapy verify normal B12 level Key Points - Anemia Order CBC for case finding Anemia is a finding that requires a diagnosis MCV helps establish the probable differential diagnosis Give Fe therapy only for Fe deficiency anemia Vitamin B12 deficiency can be treated with oral therapy No specific treatment for the anemia of chronic disease (no supplements) Questions from the Audience?