Extended Treatment Effects with Zoledronic Acid
advertisement

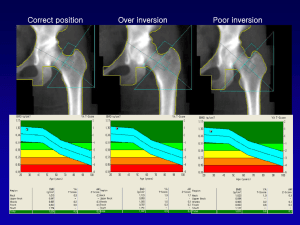
Extended Treatment Effects with Zoledronic Acid Based on Poster 1070 “The Effect of 3 Versus 6 Years of Zoledronic Acid Treatment in Osteoporosis: a Randomized Extension to the HORIZON-Pivotal Fracture Trial (PFT)” Saturday, October 16, 2010 ASBMR 2010 Toronto, Ontario Background and Method • Zoledronic acid (ZA) 5 mg used annually for 3 years has been shown to be effective in increasing BMD and decreasing fractures • The extension trial of HORIZON-PFT evaluated the effect of continuing ZA for 3 more years • All patients eligible for the extension trial had to have received all 3 annual infusions of ZA • A total of 1233 women were randomized to either ZA for 3 more years (Z6 group) or to placebo (Z3P3 group) • Baseline characteristics of the two groups were similar with about half of each group having bone mineral density (BMD) T-scores at the femoral neck <-2.5 and about 60% having 1 or more vertebral fractures. End Points Primary Outcome Measure: Per cent change in BMD of femoral neck at year 6 relative to year 3 Secondary Outcome Measures: • Change from baseline of biochemical markers of bone turnover at different time points • Per cent change from baseline in BMD of spine and distal radius at year 4.5 and 6 • Per cent change from baseline in BMD of femoral neck, total hip and trochanter at different time points • Proportion of patients with new vertebral fractures and incidence of clinical fracture • Bone biopsy to evaluate bone quality • Evaluation of safety parameters (renal function, laboratory parameters, adverse event profile) Results Mean per cent change in femoral neck BMD over the 3-year extension remained constant in the Z6 group compared with a slight drop in the Z3P3 group for a between-group difference at year 6 of 1.04% (P=0.0009) Results • Mean per cent changes in total hip BMD were similar to those at the femoral neck at 4.2% for the Z6 group vs. 2.8% for the Z3P3 group • Over the 6 years of treatment, the Z6 group had a significant mean femoral neck BMD increase of 4.5% vs. 3.1% for the Z3P3 group • Mean lumbar spine BMD increased by 12% from baseline for the Z6 group vs. 10% from baseline in the Z3P3 which was not statistically significant • Biochemical markers remained constant in the Z6 group but rose slightly in the Z3P3 group Results • The morphometric verterbral fracture rate was 6.2% in the Z3P3 group; this rate was reduced by about 52% in the group receiving ZA for 6 years • Only 11 clinical vertebral fractures were seen during the extension study and there was no difference between the 2 groups • There was no difference in non-vertebral fracture rates between the 2 groups • A total of 15 hip fractures occurred during the extension study and there was no difference in hip fracture rates between the 2 groups Adverse Events (AEs) • Overall AEs were similar in the 2 groups; serious AEs were numerically more frequent in the Z6 group but this difference was not statistically significant • No long-term effect on renal function was observed and there were no differences in CV event rates between the 2 groups • Only 1 case of osteonecrosis of the jaw occurred in the Z6 group and there were no atypical fractures in either group • Hypertension was almost twice as common in the Z3P3 group vs. the Z6 group Conclusions • A comparable safety profile was observed in the 3-year extension with the first 3-year data • After 3 years of ZA therapy, it may be beneficial for some women, particularly those at high risk for vertebral fracture, to continue on ZA • In making decisions about long-term use of BPs, it is important to individualize treatment decisions and to try to identify women for whom a drug holiday may be appropriate