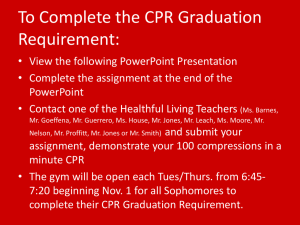
Automatic External Defibrilation 1
advertisement

Automatic External Defibrillation Past, Present & Future Prof. John McC Anderson CTO HeartSine Technologies Ltd THE DISTRIBUTION OF ACUTE CORONARY DEATHS Mc NEILLY (BELFAST), 1965-66, 818 DEATHS 100 PERCENTAGE ALIVE 90 80 70 60 50 40 30 20 10 0 0.1 HR 0.2 HR 1 DAY INTERVAL AFTER ONSET 7 DAY Modern Developments in Out-of-Hospital Defibrillation Period Defibrillator Operator Comments 1960’s Physicians Physicians staff the first mobile coronary care unit (Belfast, New York City). Early 1970’s Paramedics Extensively trained (400-1500 hours). Defibrillation added to many advanced life support skills. Late 1970’s EMT’s trained in defibrillation Rhythm recognition and skills of defibrillation taught to EMT’s in 10 hour course. The Semi-Automatic Defibrillator Flow Diagram for Ventricular Fibrillation Detection Energy Ratio Characteristic Energy Ratio i.e. Yellow/Red ratio constant in Sinus Rhythm Energy Ratio i.e. Yellow/Red ratio continuously variable in Ventricular Fibrillation Flow Diagram for Ventricular Fibrillation Detection Flow Diagram for Ventricular Fibrillation Detection The Future Management of Sudden Cardiac Death Defibrillators in the Home (PDU) The development of a CPR-ICG PAD The evolution of ‘Smart Defibrillation’ The Personal Defibrillation Unit – PDU 400 Statistics More than 650,000 deaths per year from cardiovascular diseases In the US around 800,000 patients suffer an AMI annually of whom 550,000 die Over 80% of the deaths occur in the home PEA accounts for over 65% of cardiac arrests In 2005 the ERC and AHA guidelines were updated to emphasize the importance of effective chest compressions with minimal interruptions In 2008 the AHA introduced the “hands-only” protocol Design Features Smaller Lighter Complete Resuscitation System High IP rating Advanced Algorithm Disposable User Friendly The Development of a CPR-ICG PAD The History of Impedance Cardiography Transthoracic Impedance: “Change in thoracic impedance may be due to any change in physical shape or content of the thorax, including ventilation, cardiopulmonary blood flow ….” Miller JC, Horvath SM. Impedance Cardiography. Psychophysiology 1978; 15: 80-91 ECG/ICG Timing Impedance Cardiography (ICG) The ICG measures the cardiac impedance during the cycle and gives a waveform relating to the change in blood volume within the heart during this time. (Cardiac Output) Example Cases from RVH Database Patient required terminating shock ; HR=189BPM, QRS width 201ms. Patient conscious ; HR=330BPM, QRS width varies between 133ms and 189ms. ECG ICG Causes of change in Cardiac Output Blood Flow in the aorta Blood Flow through the pulmonary vessels Contracting heart Changing resistivity of blood Improved contact with electrodes Importance of Effective CPR PEA accounts for over 65% of cardiac arrests In 2005 the ERC and AHA guidelines were updated to emphasize the importance of effective chest compressions with minimal interruptions. In 2008 the AHA introduced the ‘hands-only’ protocol to further minimize interruptions. CPR Feedback Indicator ICG can offer feedback on cardiac output during chest compressions The morphology of the ICG waveform during CPR is distinctive HeartSine has developed an algorithm based on the RVH database of CPR cases which uses a number of parameters to enable feedback on CPR efficacy for the user ICG Waveform During CPR ICG Waveform During Sinus Rhythm ICG Waveform During PEA ICG not present due to absence of CARDIAC OUTPUT during PEA ICG During VF ICG not present due to absence of CARDIAC OUTPUT during VF Challenges in Algorithm Development Noise due to motion artifact Noise due to incorrect pad or hand placement Initial ICG algorithm classified some cases of noise as CPR Results from initial Bench Tests It was found through a number of bench tests that excessive noise could be eliminated by measuring the rate and pulse width of the signal and by focusing efforts on good CPR training to ensure the correct hand positioning and applied force Recording of Correctly Applied CPR During Initial Bench Testing Recording of Poor CPR (No Compressive Force Applied) Recording of CPR on Top of Pads Proposed CPR-ICG Algorithm “PUSH HARDER” “PUSH FASTER/SLOWER” “GOOD COMPRESSIONS” Algorithm Results to Date CPR Criteria ICG Test Sample Size Performance Specifications Performance Results (%) 90% One-Sided Lower Confident Limit (%) CPR Speed Good 82377 Sensitivity: > 90% Specificity: > 90% Sensitivity: 95.38 Specificity: 93.11 Sensitivity: 83.40 Specificity: 82.19 CPR Force Adequate 108728 Sensitivity: > 90% Specificity: > 90% Sensitivity: 99.96 Specificity: 98.47 Sensitivity: 99.54 Specificity: 96.29 Animal Study Results ICG amplitude at varying compression depths: 1- ICG Amplitude in Ohms Thrust/depth 2cm = 20kg 4cm = 30-40kg 6cm = 60-70kg 0- 2cm 4cm 5cm The ICG amplitude (in ohms) is higher for higher CPR compression depths and values of ET CO2. Summary “In order to maintain high-quality CPR, feedback to rescuers is important. The use of prompt/feedback devices during CPR will enable immediate feedback to rescuers, and the data stored in rescue equipment can be used to monitor the quality of CPR performance and provide feedback to professional rescuers during debriefing sessions .” ERC Guidelines 2010 - European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators HeartSine samaritan PAD 500P with CPR advisor was launched in August 2009 in Europe Preparations are under way for FDA 510(k) clearance in the US The Development of a SMART Defibrillator Optimal treatment for Sudden Cardiac Arrest (SCA) Interactive CPR Accurate decision to defibrillate/CPR Management of PEA The FUTURE of Defibrillation Features to be included in the SMART AED: 1. CPR-ICG Indicator 2. Pulse checker (Uses ICG to discriminate between PEA and SR) 3. Therapy Advisor (Uses DSP to extract information on frequency content of the ECG signal during cardiac arrest to determine whether CPR or defibrillation is the most appropriate therapy) 4. Using ICG to discriminate between CPR and shockable rhythms during the “hands-off” period 5. Continuous chest compressions until administration of shock 3-Phases of a Sudden Cardiac Arrest Majority of customer queries result from nonadherence to the “hands-off” or analysis period of the PAD Using ICG technology we plan to develop an algorithm to discriminate between CPR and a shockable rhythm to prevent the device from charging and then disarming following the discontinuation of CPR The algorithm can output audio voice prompts which will advise the user to discontinue CPR Failure to adhere to CPR prompts CPR continued during analysis phase despite audio prompts Shock advised due to inappropriate CPR HeartSine Technologies currently has the basic science to build a SMART defibrillator. A SMART defibrillator will provide the optimal treatment for Sudden Cardiac Death SMART defibrillation will position HeartSine Technologies as a world leader in this field. In 1775 Abilgard recorded that he “shocked a single chicken into lifelessness and upon repeating the shock, the bird flew off and thus eluded further experimentation” Any Questions?