Barry Stults, MD - Ogden Surgical
advertisement

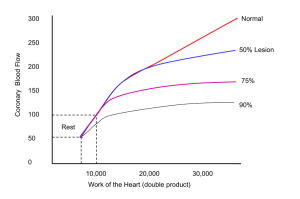
HYPERTENSION: EVIDENCE-BASED UPDATE, 2013 (Waiting for JNC-8, Still!) Barry Stults, M.D. Division of General Medicine University of Utah Medical Center May, 2013 This presentation has no commercial content, promotes no commercial vendor and is not supported financially by any commercial vendor. I receive no financial remuneration from any commercial vendor related to this presentation. HTN: DOMINANT CONTRIBUTOR TO GLOBAL MORTALITY Increases RR by 2.0-4.0 fold for: • CAD, stroke, HF, PAD • Renal failure, AF, dementia, cognition Attributable risk for HTN: • Stroke • CKD • HF 62% 56% 49% • MI • Premature death 25% 24% Aftermath: • Shortens lifespan 5y • $93.5 billion/y in U.S. Circulation 2012; 125:e12 J Hum Hypertension 2008; 22:63 Hypertension 2007; 50:1006 NEWLY RECOGNIZED CONSEQUENCES OF HTN Framingham cerebral MRI study (cross-sectional): – 579 subjects, mean age = 39.2y White-matter microstructural damage • Anterior corpus callosum Systolic BP: • Pre-HTN • HTN • Fronto-occipital fasciuli • Fronto-thalamic fibers Temporal lobe grey matter atrophy SBP before age 50 damages cerebral loci associated with cognitive dysfunction! Lancet Neurology 2012; 11:1039 HTN PREVALENCE, 2010: NHANES All • White • Black • Hispanic • Age 60y % BP 140/90 30% 29% 42% 27% 67% - No change in HTN prevalence since 2000 • 75 million Americans have HTN JACC 2012; 60:599 HTN CONTROL (< 140/90) RATES: 1988-2010 NHANES All 1988 2001 2010 Healthy People 2020 Goal Canada 2010 VA 2010 27% 29% 47% 61% 65% 76% (40% M, 56% W) • White --- 30% 50% --- --- --- • Black --- 25% 41% --- --- --- • Hispanic --- 25% 34% --- --- --- • CVD --- --- 55% --- --- --- • DM < 130/80 --- --- 42% --- --- --- • CKD < 130/80 --- --- 39% --- --- --- ‒ No U.S. improvement since 2007! Circulation 2012; 126:2105 CMAJ 2011; 183:1007 Circulation 2012; 125:2462 JACC 2012; 60:599 U.S. HTN CONTROL: 39 million 140/90! - YET 85% HAVE HEALTH INSURANCE! 40% Unaware 45% Rx’d, Uncontrolled • Older, women, obese, AA, CKD, CVD, DM 15% Aware, No Rx • Younger, men, Hispanic, finances, 0-1 visits/y Screening • Work, CC’s, church Media outreach Access to care Pseudo-HTN • Control for • Insurance BP variability • Availability • Measure BP accurately • Detect WCH MMWR 2012; 61:703 MMWR 2011; 60:103 Rx Rx inertia efficiency • 65% on 1-2 drugs Circulation 2011; 124:1046 Pt adherence Can J Card 2012; 28:375 HOW LOW TO GO? TARGET BP, 2013 Guideline General Age 80 JNC-7, 2003 < 140/90 CHEP, 2013 CKD DM --- < 130/80 < 130/80 < 140/90 < 150 < 140/90 < 130/80 --- --- <140/90 if ACR <30 130/80 if ACR ≥ 30 < 140/90 if ACR <30 130/80 if ACR ≥ 30 < 140/90 < 150/90 --- --- ACCF/AHA, 2011 --- 140-145* --- --- ADA, 2013 --- --- --- JNC-8, 2013 ? ? ? NKF-KDIGO, 2012 NICE, 2011 *Initiate Rx if SBP 150 mm Hg ** <130/80 in younger/↑ stroke risk pts < 140/80** ? Can J Card 2013; online 3/25 BMJ 2011; 343:d4891 Circulation 2011; 123:2434 Diabetes Care 2013; 36:Suppl 1:S11 Kid Int 2012; supplement 2:341 AGE 80Y: HOW LOW TO GO? HYVET RCT, 2008: 3845 pts age 80y, SBP = 160-199 Final SBP = 157 Initial SBP = 171 Placebo Indapamide ACE-I Final SBP = 143 Total Stroke Fatal Stroke Mortality CHF RRR 30% 39% 21% 64% J-Curve concern: too low BP in very elderly? • Optimal BP, age 80y: 140/70, INVEST RCT (post-hoc) NEJM 2008; 358:1887 Circulation 2011; 123:2434 GOAL BP: HOW LOW FOR AGE 80y? • INVEST RCT: BP Rx in 22,576 CAD pts Circulation 2011; 123:2434 CKD: HOW LOW TO GO? Systematic review, 3 RCTs: MDRD, AASK, REIN 133-141/80-86 2272 pts 130-139/80-89 < 130/80 126-130/77-80 RRR CVD events NS CKD progression NS Mortality NS • Subgroup with proteinuria 300-1000 mg/d*: HR CVD events NS CKD progression 24-39% *Low quality evidence Ann Int Med 2011; 154:541 DIABETES MELLITUS: HOW LOW TO GO? Meta-analysis: 13 RCTs, mean achieved systolic BP 37,736 pts < 140 135 130 Risk Reduction vs < 140 135 Total mortality Stroke MI ESRD/2X Cr 10% 17% NS NS 130 NS 47% NS NS • Target BP = 130-135 reduces mortality/stroke? • Target BP 130 reduces stroke? Circulation 2011; 123:2799 GOAL BP: HOW LOW TO GO? < 140/90: Low enough? < 130-135? < 110-120/60-70: Too low, J-curve? 1 Prevention vs 2 Prevention? SPRINT: 9000 patients, 2018 completion • High CVD risk • CKD • Age 75 PODCAST, SPSSS, SHOS: Post-stroke/TIA PLOS Medicine 2012; 9:e1001293 Hypertension 2012; 59: Circulation 2011; 124:1700 CHALLENGES TO CLINICAL VALIDITY OF OFFICE BP Inherent BP Variability: over min months! • 20% SBP 10 mm Hg over 1-2 min • 4-5 office visits for BP to stabilize Inaccurate BP Measurement: Rule, not Exception! • 93% make technical errors - Mean # errors = 4 “True” or usual BP Predicts CVD Risk Out-of-office BP Office BP for Many! • White-coat HTN in 20-33% • Masked HTN in 10% Am J Hypertens 2011; 24:1073 Ann Int Med 2011; 154:781 J Gen Int Med 2012; 27:623 BP MEASUREMENT: KEY TECHNIQUES BP (mm Hg) if not done Rest ≥ 5 min, quiet 12/6 Seated, back supported 6/8 Cuff at midsternal level 2/inch Correct cuff size 6-18/4-13 if too small 7/5 if too large Bladder center over artery 3-5/2-3 Deflate 2 mm Hg/sec SBP/ DBP No talking during measurement 17/13 If initial BP > goal BP: 1st reading higher 3 readings, 1 min apart • “Alerting response” Discard 1st, average last 2 • Reclassify 18-34% as normotensive with last 2 readings J Clin Hypertens 2012;14:751 Hypertension 2005; 45:142 J Gen Int Med 2012; 27:623 J Hypertens 2005; 23:697 Can J Card 2012; 28:270 RESEARCH QUALITY vs ROUTINE OFFICE BP # of pts Routine Clinical Practice BP Research Quality Office BP Difference Myers, 1995 147 146/87 140/83 - 6/4 Brown, 2001 611 161/95 152/85 -9/10 Myers, 2009 309 152/87 140/80 -12/5 Graves, 2003 104 152/84 138/74 -14/8 Gustavsen, 2003 420 165/104 156/100 -9/4 Campbell, 2005 107 150/91 139/86 -11/5 Head, 2010 6817 150/89 142/82 -8/7 Burgess, 2011 181 145/85 132/79 -12/6 Study Powers, 2011 444 145/129/Accurate measurement BP by 10/7 mm Hg -16/- 2X improved HTN control rate (Powers, Burgess, 2011) Ann Int Med 2011; 154:781 Am J Hypertens 2005; 18:1522 Hypertension 2010; 55:195 BMJ 2010; 340:1104 JASH 2011; 5:484 OUT-OF-OFFICE BP MEASUREMENT TO DX HTN? CHEP, 2005 2013; AHA, 2008: optional OBPM vs ABPM vs HBPM 2 Office Visits: BP ≥ 180/110 Yes or ≥ 140/90 and CVD, DM, or CKD Dx HTN No: BP = 140-179/90-99 and low risk R/O White-coat HTN: 20-33% Serial Office Visits: • 3 if BP 160/100 • 5 if BP = 140-159/90-99 24h ABPM: • Daytime BP 135/85 • 24h BP 130/80 BP < 135/85 Home BPM x 7d • Mean BP 135/85 Dx HTN Can J Card 2012; 28:270 HOME BPM: PROS AND A FEW CONS! Pros vs Office BPM: • More accurate HTN Dx in most studies ‒ More measurements out-of-office measurements • Better CVD prediction: similar to ABPM ‒ Meta-analysis: 8 studies; 17,688 pts; 3.2-10.9y FU • Improves BP control: systolic BP 3.4-8.9 mm Hg ‒ AHRQ 2012 systematic review: 6 high quality studies Cons vs Office BPM: • Not yet proven to CVD events better • Expense/inadequate patient training J Hypertens 2012; 30:449, 463, 1289 Hypertens Res 2012; 35:750 AHRQ, 2012; #45 HBPM MONITOR VALIDATION: NOT ALWAYS ACCURATE! For populations: AAMI, BHS, IP validation protocols • Omron, A&D Medical (Lifesource), MicroLife, other • Listings of validated devices: www.hypertension.ca/devices-endorsed-by-hypertension-canada www.bhsoc.org/blood_pressure_list.stm www.dableducational.org For individuals: office validation at purchase and q 1y • Sequential method, 1 arm: < 5 mm Hg diff., last 2 tests: Osc D – Osc D – Ausc D – Osc D – Ausc D • Simultaneous method, 2 arms: < 5 mm Hg diff for averages Osc R arm/Ausc L arm Ausc R arm/Osc L arm • Esp. elderly, DM, CKD, obese (tronco-conical arm) Hypertension 2008; 52:13 Hypertension Res 2012; 35:777 HBPM: RECOMMENDED MONITORING PROTOCOL Morning Work Evening ? 6-9 PM 1h post-awaken Post-micturition --- Pre-breakfast Pre-supper (or pre-bed?) Pre-BP med Pre-BP med Rest quietly 3-5 min Rest quietly 3-5 min Measure X 2, 1 min apart Measure X 2, 1 min apart • For Dx or 2wk post-med: For 3-7 days (12-28 readings) - drop 1st day, average last 2-6 days - 66% adherence! • Stable BP period: For 3-7d, q 3-4 mo vs ongoing 3d/wk J Hum Hypertens 2010; 24:779 Hypertension 2011; 57:9081 Hypertens Res 2012; 35:777 HBPM: NEW BP DX THRESHOLDS, 2013 AHA/ESH 2008 home BP Dx thresholds: • Statistically-based (95th percentile) from cross-sectional analyses International Database of Home Blood Pressure, 2012 Dx thresholds: • CVD outcome-based from prospective population studies ‒ 5018 untreated patients, mean FU = 8.3y AHA/ESH Office BP Home BP IDHOCO 2012 Home BP 160/100 ? 145/90 140/90 135/85 130/85 130/85 ? 125/80 120/80 ? 120/75 Hypertension Res 2012; 35:1072 Hypertension 2013; 61:27 HBPM: DOCUMENTATION/COMMUNICATION/ACTION AM/PM BP X 3-7 days Documentation: avoid inaccurate/selected readings Paper: Horizontal logbook to gestalt mean BP Device with Printer: • Bring all print-outs Circuit memory: • Transfer via computer • Record all values Regular/Timely Communication of Data: • Office visit, mail, FAX, computer Action by Clinician/Team • Dx • Rx adjustment, prn Hypertension Res 2012; 35:777 Home BP Log: Horizontal Orientation REDEFINE OFFICE BP MEASUREMENT: AUTOMATED OFFICE BP (AOBP)? 3 validated devices automatically measure/average multiple BP’s: 6 readings – average last 5 BpTRU • q 1 min: start of one start of next ($900-1100) 3 readings – average all 3 Omron HEM-907 • q 1 min: end of one start of next ($520) Microlife Watch BP office ($1100) 3 readings – average all 3 • q 1 min: end of one start of next • Additional auscultatory mode • Provide comparable mean readings • Similar time to complete 6 vs 3 readings Can J Card 2012; 28:341 J Hypertens 2012; 30:1894 REDEFINE OFFICE BP MEASUREMENT: AUTOMATED OFFICE BP (AOBP)? 3 basic principles of AOBP: – Fully automated device Eliminates many technical errors • More accurate – Multiple measurements taken Controls for BP variability • More reproducible – Performed in isolation Reduces white-coat effect • Equivalent to daytime ABPM Can J Card 2012; 28:341 J Hypertens 2012; 30:1894 SEQUENTIAL BpTRU READINGS IN 284 PATIENTS IN PRIMARY CARE Reading No. AOBP 1 (observer present) 147/82 2 (observer absent) 140/79 3 “ 136/78 4 “ 134/77 5 “ 132/76 6 “ 133/77 Mean 2-6 136/78 What does this pattern mean? BMJ 2011; 342:d286 AOBP ON ISOLATED PATIENTS: WHITE COAT HTN Beckett, 2005 Routine Office BP BpTRU AOBP Daytime ABPM 151/83 140/80 142/80 152/87 132/75 134/77 150/89 133/80 135/81 149/83 138/80 141/80 150/81 136/78 133/74 • 481 pts Myers, 2009 309 pts Myers, 2010 254 pts *Godwin, 2011 654 pts *Myers, 2011 303 pts AOBP, isolated pt, is close to daytime ABPM: reduces WCH * 1 care Can J Card 2012; 28:341 Hypertension 2010; 55:195 BMJ 2011; 342:d286 Fam Pract 2011; 28:110 EQUIVALENT BPs TO DX HYPERTENSION Routine office BP Research quality office BP* Daytime ABPM* BP, mm Hg ? 140/90 135/85 130/80 • 24 hour ABPM* Home BP for 3-7 days* AOBP, isolated patient** 135/85 (130/85?) 135/85? *Supported by CVD outcome data **Superior to routine BP for LV mass, CIMT, albuminuria but CVD outcome data pending (CAMBO RCT) Hypertension 2012; 11/5 epub J Hypertens 2012; 30:1894 J Hypertens 2012; 30:1906 Am J Hypertens 2012; 25:969 Am J Hypertens 2011; 24:661 TREATMENT OF HYPERTENSION LIFESTYLE MODIFICATION: OLD AND NEW BP, mm Hg Wt loss/Kg: diet 1/1 • 4 kg: diet 6/- • 4 kg: orlistat 2.5/- • 4 kg: sibutramine 0/0 • 16%, 10y: bariatric surgery 0.5/ 2.6 Exercise: • Land-based, to 90 min/wk 5/3 - benefit in elderly • Swimming RCT, 45 min, 3-4d/wk, x 3 mo 9/4 Eur Heart J 2011; 32:3081 Am J Card 2012; 109:1005 LIFESTYLE MODIFICATION: OLD AND NEW BP, mm Hg DASH diet RCT: 11/6 • Fruit, veggies, low fat dairy, low sat fat Black tea RCT: 2/2 • 3 cups/d X 6 mo Coffee: 0.5/0.5 (NS) • 10 RCT; 5 cohort studies Alcohol meta-analysis: • 2 drinks/d 0/0 • 3-5 drinks/d 3/2 Eur Heart J 2011; 32:3081 J Hypertens 2012; 30:2245 Arch Int Med 2012; 172:186 J Clin Hypertens 2012; 14:792 LIFESTYLE MODIFICATION: OLD AND NEW Outcome Sugar-sweetened drinks: HTN 13% Artificially-sweetened drinks: HTN 14% • 3 prospective cohorts, 223,891 pts Vitamin D: • 2 meta-analyses No BP effect • RCT, winter months RCT, blacks 4/3 if Vit D < 32 ng/ml 4/2 Dark Chocolate: • RCT, 6.3 g, 30 cal/d 3/2 • RCT, 100 g, 500 cal/d 5/3 Hypertension 2013; 61:779 J Gen Int Med 2012; 27:1197 Am J Hypertens 2012; 25:1215 Eur Heart J 2011; 32:3081 Am J Hypertens 2012; 23:97 LIFESTYLE MODIFICATION 2012; “SALT WARS” Dietary Na < 1500 – 2300 mg/d (IOM, DHSS, AHA 2012) Benefits Na intake 1.2-2.4 g/d SBP: HTN: 4-7 mm Hg NT: 2.5-3.5 mm Hg ?? Adverse effects renin, aldosterone catecholamines triglycerides insulin resistance (?) (esp. if abrupt, severe, or DM) Potentially prevent 11 million HTN cases Dietary Na CVD? • 2011-2012: 6 risk association studies 2 Benefits; 2 Harm; 2 J-curve • 2011-2012: 3 meta-analyses 1 Benefit 1 No benefit 1 J-curve NEJM 2013; 368:1229 Am J Med 2012; 125:443 Circulation 2012; 126:2880 Am J Hypertens 2012; 25:727 “SALT WARS”: THE SCIENTIFIC RESPONSE AHA Presidential Advisory, Dec 2012: “The evidence base supporting recommendations for reduced sodium intake to < 1500 mg/d in the general population remains robust and persuasive.” British Hypertension Society, July 2011: “The benefits of salt reduction are clear and consistent.” Reviewer commentary, AJH, Jan 2012: “Community sodium reduction: is it worth the effort?... A concerted campaign to reduce obesity and alcohol intake may be more rewarding and less risky.” Reviewer commentary, AJH, Jan 2012: “The solution to the debate is the conduct of a large-scale, long-term clinical trial.” “SALT WARS”: THE MEDIA/INDUSTRY RESPONSE NY Times, June 2012: “Now, salt is safe to eat.” London Daily Express, July 2011: “Now salt is safe to eat – Health fascists proved wrong after lecturing us all those years.” Forbes.com, June 2011: “Campbell Soup increases sodium as new studies vindicate salt.” EDUCATION TOOLS FOR LIFESTYLE MODIFICATION Low diet Na/DASH diet: Canadian HTN Education Program www.hypertension.ca/images/2012_HealthyEatingFor HealthyBloodPressure_EN_P1017.pdf www.sodium101.ca DASH diet: www.dashdiet.org www.mayoclinic.com/health/dash-diet/H100047 In Spanish: www.wellnessproposals.com/nutrition/handouts/dashdiet/DASH-diet-eating-plan-spanish-version.pdf OPTIMAL 1st DRUG RX FOR HTN? RECOMMENDATIONS FROM RECENT GUIDELINES Preferred Acceptable ACE-I ARB • Esp. age < 55, white • Concern with ─ ↓ BP MI protection in 2011/2012 Thiazides meta-analyses • Esp. age > 65, or blacks ─ ↓ BP • Chlorthalidone? ─ ↓ BP CCB Can J Card 2012; 28:270 J Gen Int Med 2012; 27:618 Less Useful Alpha-blockers • HF, stroke protection Beta-blockers • stroke, MI protection age > 60 DRI (aliskiren) • stroke in ALTITUDE BMJ 2011; 343:d4891 www.heartfoundation.org.au BMJ 2011; 342;d2234 Eur Heart J 2012; 33:2088 JAMA 2012; 208:1340 BMJ 2009; 338:b1665 HCTZ vs CHLORTHALIDONE: CHOICE GIVEN MOSTLY INDIRECT EVIDENCE? Efficacy to lower BP: • Meta-analysis: 26 RCTs; 4683 pts Dose to SBP 10 mm Hg HCTZ 26.4 mg CTDN 8.6 mg (Similar BP reduction at maximal doses) • RCT: 609 pts on azilsartan 40 mg 12.5-25 mg thiazide SBP: CTDN-HCTZ = 5.6 mm Hg, p < 0.001 HTN control < 140/90 = 64% vs 46%, p < 0.001 Hypertension 2012; 59:1104 Am J Med 2012; 125:1229.e1 HCTZ vs CHLORTHALIDONE: CHOICE GIVEN MOSTLY INDIRECT EVIDENCE? Efficacy to reduce CVD events: indirect comparisons Risk Reduction CTDN vs HCTZ Network meta-analysis: • 3 HCTZ RCTs; 6 CTDN RCTs MRFIT post-hoc analysis Observational Cohort 21% p value < 0.0001 21% 7% 0.002 NS ( Hosp. for K, Na) Ann Int Med 2013; 158:447 Hypertension 2012; 59:1110 Hypertension 2011; 57:689 HCTZ vs CHLORTHALIDONE: CHOICE GIVEN MOSTLY INDIRECT EVIDENCE? Practical utility: • Availability: CTDN less available in retail pharmacies • Preparation: HCTZ: 12.5 mg, 25 mg tabs CTDN: unscored 25, 50 mg tabs • Fixed-dose combinations: HCTZ: 19 at 12.5 and 25 mg doses CTDN: 3 (azilsartan ($90/mo), atenolol, clonidine) INITIAL 2-DRUG vs DELAYED 2-DRUG Rx Rationale: • 75% need 2 drugs, 30% need 3 drugs ‒ Especially if BP 160/100, obese, CKD, DM • Low-dose 2-drug vs High dose 1 drug: ‒ Greater SBP reduction (3-4 mm Hg) ‒ Fewer side effects Benefits in studies: • year 1 HTN control rates 20-50% (RCTs, cohorts) • year 1 CVD events 11-34% (cohort, case-control studies) • health care costs 10% Caution: frail elderly, baseline orthostatic BP Hypertension 2012; 59:1124 Hypertension 2013; 61 (Feb) Curr Opin Neph Hypertens 2012; 21:486 OPTIMAL 2-DRUG RX FOR HTN? AMERICAN SOCIETY OF HYPERTENSION, 2010* Preferred Acceptable Less Acceptable ACE-I (ARB)/CCB CCB/D ACE-I/ARB • ACCOMPLISH RCT: 2008, 2010 ACE-I (ARB)/D • Esp. AAs BB/D • DM BB/DHP-CCB *Based on BP, side effects, or CVD-CKD outcomes Dual CCB DRI/D or CCB • No CVD, little BP, side effects ACE-I (ARB)/BB • Little BP DRI/ACE-I (ARB) • stroke in ALTITUDE BB/Clonidine or non-DHP-CCB • Bradycardia J Am Soc HTN 2010; 4:42 Eur Heart J 2011; 32:2499 ACE-I/CCB vs ACE-I/DIURETIC? ACCOMPLISH, 2008: 11,056 high CVD risk patients x 36 mo Benazepril/Amlodipine vs Benazepril/HCTZ Others CVD events CKD events Others ACE-I/CCB ACE-I/D HR CI 9.6% 2.0% 11.8% 3.7% 0.80 0.52 0.72-0.90 0.41-0.65 • 2X Cr • Dialysis • No difference in CVD events in obese • No difference in CKD events in AAs Kid Int 2012; 81:568 ASH, 2012 abst. NEJM 2008; 359:2417 Lancet 2010; 375:1173 PREFERRED 3-DRUG HTN RX? EXPERT CONSENSUS ONLY • Diuretic/ACE-I (ARB)/CCB • Diuretic/BB/DHP-CCB • ACE-I/CCB/alpha-blocker (ASCOT RCT) Can J Card 2012; 28:270 1 HTN DRUG AT BEDTIME: CHRONOTHERAPY? 2 RCTs: 448 pts, T2DM HTN 661 pts, CKD HTN 5.4y All HTN meds AM 5.4y 1 HTN med HS • nocturnal BP but same daytime BP • CVD events with 1 HTN med HS: ‒ T2DM: 75% for CVD death MI stroke ‒ CKD: 71% for CVD death MI stroke ADA 2013 Standard of Care: give 1 HTN med HS • Need more studies! J Am Soc Neph 2011; 22:2313 Diabetes Care 2011; 34:1270 Diabetes Care 2013; 36:(Suppl 1):S11 RESISTANT HYPERTENSION Definition: – BP 140/90 x 3 mo on 3 meds (diuretic optimal dosing) Prevalence: – Increasing in NHANES – 16 million Americans 1994 2004 2008 8.8% 14.5% 20.7% Risk factors: – Age 75, obesity, CKD, DM, SBP, blacks/Hispanics Prognosis: – 50% CVD/CKD events in 1st 4y (Kaiser Permanente) Circulation 2012; 125:1594, 1635 Hypertension 2011; 57:1045, 1076 Circulation 2011; 124:1046 Curr Opin Card 2012; 27:386 SUSPECT RESISTANT HTN: • BP ≥ 140/90 (AOBP ≥ 135/85) x 3 mo – accurately measured • ≥ 3 medications: optimal dosing diuretic RULE-OUT PSEUDO-RESISTANT HTN: for non-compressible arteries: RFs orthostatic symptoms for white-coat resistant HTN: 24h ABPM or HBPM for optimal 3 drug Rx: CCB ACE-I (ARB) diuretic eGFR for low Rx adherence to medication CONSIDER ( EVALUATE) 2 CAUSES OF HTN INTENSIFY LIFESTYLE RX: DIET Na EXERCISE ADD APPROPRIATE STEP 4/5 MEDICATIONS RULE-OUT PSEUDO-RESISTANT HTN for non-compressible arteries: • RFs: age, ESRD, DM calcific AS, scleroderma • Orthostatic dizziness despite standing BP Clinical suspicion high Intra-arterial BP measurement J Hum Hypertens 1997; 11:285 Blood Press Monit 2003; 8:97 RULE-OUT PSEUDO-RESISTANT HTN for White-coat resistant HTN: 24h ABPM or HBPM Study # Patients % White-Coat RH Redon, 1998 86 33% Brown, 2001 118 28% Pierdomenico, 2005 276 49% Hermida, 2005 700 17% Oikawa, 2006 528 16% Salles, 2008 556 37% Douma, 2008 2302 29% De la Sierra, 2011 8295 38% • 1/3 with office RH have white-coat RH! Nat Rev Nephrol 2013; 9:51 RULE-OUT PSEUDO-RESISTANT HTN for optimal 3-drug Rx – maximal tolerated doses of: • CCB ACE-I (ARB) diuretic eGFR eGFR < 30 ml/min ≥ 30 ml/min total body Na Furosemide/bumetanide bid (8AM, 5PM) Chlorthalidone 25 mg/d or Torsemide qd Titrate dose to 4-5 lb wt loss only *22% not on diuretic 1y after Dx of RH in Kaiser system! 57% not maximally dosed on meds! Monitor creatinine/potassium carefully Eur Heart J 2013; on-line 2/5, Messerli BMJ 2012; 345:e7473 Hypertension 2012; 60:303 RULE-OUT PSEUDO-RESISTANT HTN for low Rx adherence to medication: “Drugs don’t work in people who don’t take them.” C.E. Koop, M.D. • Ask the patient: occurs in only 30% of visits with BP • Pharmacy refill rates: < 80% possession ratio • Epidemiologic clues: young, male, non-white, depression, > qd dosing, branded meds, side-effect worries • Difficult to confirm objectively: Toxicologic urine screening in RH pts in Germany 37% non-adherent J Hypertension 2013; 31:766 TRUE RESISTANT HTN: CONSIDER 2 ETIOLOGIES Drugs that BP Primary Aldosteronism Renovascular HTN OSA • NSAIDS: SBP 5 mm Hg, ≥ 10 mm Hg in 10% • OCPs: age ≥ 35, obese, smoke, AA • Epogens: in 20%, Hct • Corticosteroids: in 15-20% • Calcineurin inhibitors: cyclosporine, tacrolimus • Antiangiogenic cancer Rx agents • Stimulant/anorexic drugs for ADD, wt loss • Herbals: ephedra, ginseng, bitter orange • ETOH > 4 drinks/d, cocaine, amphetamines J Clin Hypertens 2008; 10:556 Am Heart J 2013; 165:477 TRUE RESISTANT HTN: CONSIDER 2 ETIOLOGIES Drugs that BP Primary Aldosteronism Renovascular HTN OSA • 10-20% of RH pts • < 40% have K+ • Aldosterone: independent CV toxin - 3-6X more CVD than essential HTN • AHA, 2008: screen all RH patients - Spironolactone Rx for all to CVD - Evaluate a few for adenoma – adrenal vein cath Hypertension 2008; 51:1403 J Clin Endo Metab 2008; 93:3266 PRIMARY ALDOSTERONISM: EVALUATION Aldosterone/Renin Ratio (ARR): AM sitting blood draw • No K+ - sparing diuretic x 4 wks • Normokalemic ARR < 20 No PA ARR ≥ 20 3d Na oral loading, 200 mEq/d • Early AM PRA • 24h urine: aldosterone, Na, creatinine PRA < 1.0 ug/ml/h and urine aldosterone ≥ 12 ug/d and urine Na > 200 mEq No Yes PA Spironolactone Rx vs Surgical evaluation: CT adrenal vein cath Hypertension 2008; 51:1403 TRUE RESISTANT HTN: CONSIDER 2 ETIOLOGIES Drugs that BP Primary Aldosteronism Renovascular HTN OSA Fibromuscular Dysplasia Atherosclerotic RAS Women age 50y Refractory HTN with RH Progressive eGFR, spontaneous or if Rx Screen with MRA/CTA • 50% curable • 30% improved or Recurrent HF Screen with MRA/CTA/US • Uncertain benefits Kidney International 2012; 83:28 - Θ in ASTRAL, STAR - CORAL pends TRUE RESISTANT HTN: CONSIDER 2 ETIOLOGIES Drugs that Primary Renovascular Aldosteronism HTN BP OSA • Prevalence in RH: 71-85% (vs 38-55% in non-RH) • CPAP efficacy to SBP: - Non-RH: 1.6-2.5 mm Hg (4 meta-analyses) - RH: 7-9 mm Hg?? (small observational studies) J Hypertension 2012; 30:633 MEDIATORS OF RH: ALDOSTERONE/VOLUME Gaddam, 2008; 249 RH pts vs 53 controls (controlled HTN, normal BP) Plasma aldosterone (ng/dl) 24h urine aldosterone (ug/24h) ARR BNP (pg/ml) ANP (pg/ml) RH pts 13.0 Control pts p value 8.4 < 0.001 13.0 22 37.2 95.9 9.7 6 22.5 54.8 0.02 < 0.001 0.007 0.001 RH mediated by: • Relative aldosterone excess • Persistent ECF volume expansion Arch Int Med 2008; 168:1159 INTENSIFY LIFESTYLE RX FOR RESISTANT HTN Lower Dietary Na: • 12 pts with RH: mean BP = 146/84 on 3 meds Final BP 1g Na x 7d 123/75 6g Na x 7d 146/84 ‒ Very low Na diet BP 23/9 mm Hg Aerobic Exercise: • 50 pts with RH: mean BP = 141/78 on 4 meds 8-12 wks treadmill exercise BP 6/3 mm Hg Hypertension 2009; 54:475 Hypertension 2012; 60:653 RESISTANT HTN: ALDOSTERONE BLOCKADE # Patients Office BP, mm Hg Retrospective: 2 studies 386 -25/12 Prospective obs.: 5 studies 1803 -22/10 RCT (Alvarez-Alvarez, 2010) 41 -32/11 RCT (Parthsarathy, 2011) 141 -27/12 111 -15/7 52 -18/8 Study Type Spironolactone: RCT (Vaclavik, 2011) Eplerenone: Prospective obs.: • Spironolactone side effects: hyperkalemia (3-5%); breast tenderness (5-10%) Ann Pharmacother 2010; 44:1762 J Hypertens 2010; 28:2329 J Hypertens 2011; 29:980 J Am Soc HTN 2010; 4:290 Hypertension 2011; 57:1069 RESISTANT HTN: 4-5 DRUG RX? ACE-I (ARB) DHP-CCB Thiazide (chlorthalidone) BP > goal K < 4.5 and eGFR 45 HR > 84-90/min “Sequential nephron blockade” • Spironolactone, 12.5-25 mg/d Beta-Blocker (? vasodilating) K 4.5 or eGFR < 45; HR < 84-90 Alpha-blocker: BP 16/9, obs. study Non-DHP CCB: BP 10/10, obs. study • Furosemide, 20-40 mg/d Beta-blocker alpha-blocker: Controlled 25%, obs. study • Amiloride, 5 mg/d RCT: BP 18/13, controlled 58% Device Therapy? Rev Esp Card 2009; 62:158 J Clin Hypertens 2005; 7:50 J Clin Hypertens 2012; 14:191 Am J Hypertens 2011; 24:863 BMJ 2012; 345:e7473 J Hypertension 2012; 30:1656 J Clin Hypertens 2012; 14:191 DEVICE RX FOR RESISTANT HTN: HOPE OR HYPE? Rationale: Inhibit Sympathetic NS Renal Sympathetic Overactivity: • PTRA sympathetic nerve ablation Activate Carotid Baroreceptors: • CS electrical stimulators SYMPLICITY HTN-2 RCT Rheos Pivotal RCT • 106 pts; mean BP = 178/96 • 265 pts; mean BP = 169/101 • Office BP, 6 mo = 32/12 • office BP, 12 mo: 25/- • 19% HTN control rate • 42% HTN control rate • 25% minor complication rate • FU: sustained BP to 24 mo • 25% complication rate – 5% permanent nerve deficit! • FU: sustained BP to 22 mo CAUTION! • Sub-optimal Rx regimens pre-enrollment • Short duration FU on small numbers • Based on office BP – ABPM 11/8, SYMPLICITY-2 - Suppressing primarily white-coat effect? - SYMPLICITY HTN-3 RCT in U.S. pends Hypertension 2012; 60:596 Lancet 2012; 380:591 J Hypertens 2012; 30:837, 874 Heart 2012; 98:1689 Interven Image 2012; 93:386