Renal artery disease artery an intestinal artery disease
advertisement
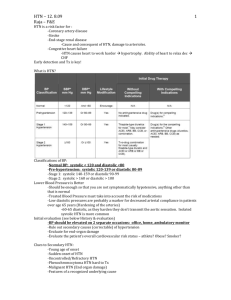
Renovascular Hypertension Definition Anatomically evident arterial disease Elevated blood pressure Goldblatt (1934) Cinically atypical Secondary to: – Renin-Angiotensin-Aldosterone Pathophysiology Renal artery stenosis Ischemia – release of renin Renin promotes conversion of angiotensin I to Angiotensin II Angiotensin II – severe vasoconstriction – Aldosterone release Pathophysiology One kidney model (diseased) – Volume is handled properly – Non-stenotic kidney – Vasoconstriction Two kidney model (both diseased) – Volume is not handled properly Unilateral renal ischemia 2 Kidney 1 clip model Hypersecretion of renin in one kidney, suppressed in the other Heyperreninemia Angiotensin II – vasoconstriction Pressure diuresis (excess sodium and water) Bilateral renal ischemia 1 kidney – 1 clip No pressure diuresis Aldosterone induced sodium and water retention Stages Immediate – Hyperreninemia – immediate rise in pressure Days to weeks – BP elevated – Contralateral kidney +/- Long term – With other kidney – Without other kidney With other kidney…. Volume expansion avoided Renin remains high Stenotic kidney retains sodium/produces renin Non-stenotic dumps sodium/water/ decreases renin Once long term defect reached – benefit of flow reversal less Without other kidney… Sodium and water retention Vasopressor effects of angiotensin II Renal perfusion maintained Renin levels fall HTN more dependent upon volume expansion …third stage HTN is unremitting Persists after removal of stenosis Ischemic nephropathy Angiotensin II Vasoconstrictive on both afferent and efferent arterioles Efferent arteriole smaller basal diameter Increase in efferent resistance > afferent Angiotensin II – mediates release of PGs and NO which dilate afferent arteriole Angiotensin II Reduces renal blood flow Decreases the mesangial surface area – Decreases filtration Increase in glomerular capillary pressure – Tends to increase filtration Healthy Kidney Fall in BP – activates renin-angiotensin Decrease in renal blood flow secondary to increased afferent resistance Preferential increase in efferent resistance – Increases glomerular hydraulic pressure – Maintains GFR Ischemic Kidney Reduced afferent flow Intraglomerular pressure depends upon Angiotensi II mediated efferent vasoconstriction ACE I – removes efferent vasoconstriction – Decreases intraglomerular pressure and GFR – ACE I – decreases renal function and azotemia Incidence Older males – proximal aortic disease Younger females – distal FMD Less common in African - Americans US – 1-5% of HTN in unselected populations – 30% of HTN in atheropaths – <1% of all HTN International – Possibly less prevalent Presentation HTN with azotemia (>1.5 mg/dl) and modest proteinuria (< 1.5 g/dl) HTN with progressive CRI, Severe HTN (diastolic > 120 mmHG) HTN with asymmetric kidney Paradoxical worsening of HTN with diuresis / ACEI Presentation Onset of HTN < 30 y.o., w/o risk factors Abrupt onset severe HTN (>160/100) HTN resistant to > 3 agents Abrupt increase in BP HX of smoking, No family Hx Systemic PAD with moderate to severe HTN, > 50 yo Presentation Recurrent pulmonary edema with modsever HTN Mod to sever HTN in a patient with an atrophic kidney Physical Exam Abdominal bruit – 46% of pts with RVHT – 9% of pts with essential HTN Advanced fundoscopic changes Recurrent flash pulmonary edema Differential Arteriosclerosis Fibromuscular dysplasia Other congenital disorders Cholesterol embolic disease Acute arterial thrombosis Aortic dissection Renal artery trauma Arterial aneurysm AVM Polyarteritis nodosa Aortic stenosis Takyasu’s arteritis Renal Vein Renin Renin release from each kidney Ischemic kidney – renal vein 1.5x non ischemic renal vein <10% of healthy patients have a > 1.5 ratio ACE I – increases the accuracy False positive and false negatives are common Of coures doesn’t work in bilateral disease Screening American College of Cardiology and the AHA – Screening for RAS – Only if intervention would be offered Imaging Studies MRA – 96-100% sensitivity, 71-96% specificity – Not useful in distal disease, FMD Spiral CT – Sensitivity 98%, specificity 94% – If Cr >1.7 mmg/dL 93% and 81% U/S – Seensitivity 72-92% Imaging studies U/S – Renal resistance indices (1-end diastolic velocity/maximum systolic velocity X 100) – RRI > 80% low likelihood that intervention will be effective Renogram with Captopril – Radioisotope 1)1 kideny accounting for < 40% of total GFR 2)delayed peak uptake by > 10 minutes – > 5 min washout in involved side A\ngiogram – RAS| > 70% – Or 50% stenosis with post-stenotic dilation SLRHC Algorithm Doppler MRA DSA - Angiogram Treatment Appropriate anti-HTN (no ACE I) Smoking cessation Antidyslipidemic Superiority if surgical intervention vs medical intervention - unproven PTA with Stent Non-total occlusions FMD – PTA (no stent) FMD “cured” 50-85%, 8-20% with atherosclerosis These numbers are improved with stenting Restenosis does occurr Surgical revascularization Reserved for pts with occluded main renal arteries Primarily a vein graft 80-90% benefit with cure or improvement Peri-op mortality < 5%