NEWBORN TRANSITION
ASSESSMENT
Mary L. Dunlap MSN, APRN
Fall 10
Newborn Care Period
•
•
•
•
Physical Adaptations
Newborn Assessment
Nutrition
Discharge Assessment
Neonatal Physiologic Adaptations
Respiratory
• Breathing noted as
early as 11 weeks
gestation
• Fetal lung fluid
necessary for
development and
decreases with
gestational age
• Functioning lungs
occurs after 26
weeks gestation
• Surfactant found in
sufficient quantity
around 35 weeks
gestation
Respiratory Adaptations
•
•
•
•
Chemical Stimulation
Mechanical Stimulation
Sensory Stimulation
Pulmonary Blood Flow
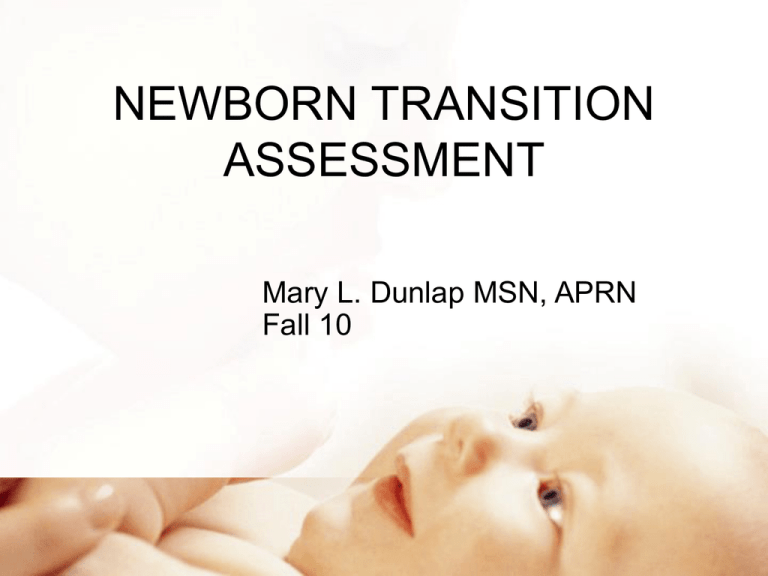
Chemical Stimulation
• Catecholamine surge prior to labor
corresponds to rapid drop in level of
fluid in lung field
• Catecholamines increase the release of
surfactant
Chemical Stimulation
• Decrease O2 & Increase CO2
concentration along with decrease pH
stimulates aortic & carotid
chemoreceptors triggering the
medulla to initiation of respirations
Respiratory Adaptations
• Surfactant promotes lung expansion
by preventing the complete collapsing
of the alveoli with each expiration.
• Increases the lungs ability to fill with
air
Mechanical Stimulation
• Compression of the chest during
vaginal birth forces 1/3 of the fluid out
of the lung fields
• Once the chest is delivered the reexpansion draws air into the lungs
• Crying creates positive intrathoracic
pressure keeping alveoli open
Sensory Stimulation
• Tactile
• Visual
• Auditory
Pulmonary Blood Flow
• Pulmonary vasodilatation occurs as
O2 enters the lungs
• The decrease in PVR allows for
adequate gas exchange and
transition
Respiratory Adaptations
• Established within 1 minute of birth
• Respirations should be quiet
• Diaphragmatic and abdominal
muscles used
• Nose breathers
• 30-60/minute
Respiratory Adaptations
• Acrocyanosis and circumoral
cyanosis 1-2hrs
• Respiratory distress nasal flaring,
grunting, costal retractions and a rate
less than 30 & greater than 60
Cardiovascular Adaptations
• Fetal to neonatal circulation occurs
simultaneously with the respiratory
adaptation
• Cessation of blood through the umbilical
vessels and placenta causes the
change from fetal to neonatal circulation
Cardiovascular Adaptation
• Closure of the ductus venosus,
foramen ovale and the ductus
arteriousus
• Shift to pulmonary circulation
Fetal to Neonatal Circulation
• Clamping the umbilical cord increases the
SVR
• Closure of the ductus venosus allows blood
flow through the portal/hepatic system
• Increase pressure in the left atrium from the
pulmonary venous return closes the foramen
ovale
• Rising O2 concentration in the blood and
decreased prostaglandin levels closes the
ductus arteriousus
Neonatal Circulation
• Apical pulse counted for a full minute
• PMI is at the 4th intercostal space to
the left of the midclavicular line
• Heart rate at birth 120-160
• Tachycardia greater than 160
• Bradycardia less than 100
Neonatal Circulation
• Capillary refill less than 3 sec.
• Femoral/Bracial pulses palpated for
symmetry, strength and rate will
provide information about the change
to adult circulation pattern
• Average systolic 60-80, diastolic 4050
Neonatal Circulation
• Average blood Volume 300ml
• Late clamping of the cord can lead to
polycythemia
• Hemoglobin 14-24g/dl
• Hematocrit 44%-64%
Neonatal Circulation
•
•
•
•
RBC 4.8-7.1/mm
WBC 9,000-30,00 per mm
Platelets 200,000-300,00
Factors II, VII, IX, and X are low due
to the lack of Vit. K
Thermogenic Adaptation
• Balance between heat loss and
production
• Newborns ability to maintain it’s
temperature is controlled by external
environmental factors and internal
physiologic process
Thermogenic Adaptation
Environmental
• Evaporation: Heat loss as water
evaporates from the skin
• Convection: transfer of body heat to
surrounding air ( cold del. Room)
Thermogenic Adaptation
Environmental
• Conduction: transfer of heat to
surface the newborn is lying on
• Radiation: loss of heat through the air
to a cooler surface ( not in direct
contact with the neonate)
Thermogenic Adaptation
Internal
• Newborns have limited ability to
shiver to generate heat
• Heat is produced by the metabolism
of brown fat
• Voluntary muscle activity: flexion of
extremities, restlessness, and crying
Thermogenic Adaptation
Effects of cold stress
• Increase O2 consumption can lead to
metabolic acidosis
• Increase glucose utilizes leads to
hypoglycemia
• Production of surfactant is decreased
and respiratory distress can occur
Signs of Cold
Stress/Hypothermia
•
•
•
•
•
•
Skin cool to touch
Mottling of the skin
Central cyanosis
Decreased responsiveness
Jittery
Tachypnea
Renal System
•
•
•
•
•
•
40 ml of urine at birth
2-6 voids/day for the first 2 days
5-25 voids/day after 48 hours
15-60 ml. of urine per/kg/day
Urine odorless straw color
Uric crystals cause pink staining in
diapers
• One year to fully mature
Gastrointestinal System
• Audible bowel sounds within 1 hour
• Stomach capacity 30-90 ml.
• Uncoordinated peristaltic activity in the
esophagus for a few days
• Immature cardiac sphincter
• Enzymes able to digest CHO, protein & fats
• 1 st meconium passed 12-24 hrs
• Transitional stool passed for 1-2 days
Hepatic Adaptation
• In utero iron is stored for use in hemoglobin
production after birth. If adequate will last till 5th
month without needing supplement.
• Glucose is stored as glycogen for neonatal
metabolic demands
• Due to the rapid depletion of glycogen during the
first 24 hours the glucose level will be between 50
to 60 mg/ml
• Feedings will help stabilize the glucose levels,
which after day 3 will be between 60-70 mg/ml
Immune System Adaptation
• Neonate depends on three
immunoglobins: IgA, IgG, and IgM
• IgG crosses the placenta and is found in
the fetus by the 3rd trimester. It protects
the newborn against bacterial and viral
infections the mother has developed
antibodies for ( tetanus, measles,
mumps)
Immune System Adaptation
• IgM is found in the blood and lymph and is
the first immunoglobulin to respond to
infection. Production starts at birth. If
elevated at birth may indicate exposure to
intrauterine infection
• IgA is found in colostrum and can
contribute to passive immunity. It limits
bacterial growth in the GI tract and is
produced gradually.
Normal Newborn Assessment
• Evaluate the newborns’ adjustment
to Extrauterine.
• Assess for possible birth trauma
• The assessment should progress
from head to toe.
Initial Assessment
•
•
•
•
•
•
•
Apgar score determined
Assess for gross abnormalities
Apply cord clamp
Obtain foot prints
Apply identification bands
Administer Vit. K & eye prophylaxis
Promote bonding
Transition to Extrauterine Life
First period of Reactivity
•
•
•
•
•
•
Birth to 30 minutes
Heart rate160 to 180 beats/min
Returns to 110-160 after 30 min
Resp. rate 60-80/crackles may be present
Reactive to stimuli
After this period newborn could sleep up to
60-100 min.
Transition Second Period
• 4-8 hours after birth
• 10 min to several duration
• Brief periods of Tachycardia and
Tachypnea
• Increase muscle tone and color
changes
• Meconium may be passed
Newborn Assessment
• Length-19 to 21 inches
• Weight- average 7lb 8oz (10th to 90th %)
SGA less than 5lb 8 oz (Less than
the 10th %)
LGA greater than 9 lb ( greater
than the 90th %)
• Newborns can loose up to 10% of birth weight
• Head circumference- 33-38 cm
• Chest circumference-31-36 cm
Newborn Assessment
• Temperature
–Normal axillary temperature 97°F–
99.5°F
• Cardiovascular system
–Normal heart rate 110–160 bpm
–Observe color, pulse, murmurs
Newborn Assessment
• Respiratory system
–Normal rate is 30–60/minute
–Nose-breather
–Observe for flaring, grunting,
retracting
–Auscultate for rales
Head
• Measure circumference
• Anterior fontanel diamond shaped closes in 18
months
• Posterior fontanel triangle shaped closes in 812 weeks
• Fontanels need to be open and soft
• Depressed fontanel indicates dehydration
• Bulging fontanel may indicate increased
intracranial pressure
Head
• Molding result of fetal position in utero and
pressure from passage through birth canal
( resolves in 24-48hrs)
• Cephalhematoma result from trauma
(resolves in few weeks)
• Caput succedaneum pressure from
delivery ( resolves in 1-2 weeks)
Head
• Inspect face for symmetry of eyes, nose, lips,
mouth and ears
• Eyes usually blue or gray, permanent color
established in 3-12 months
• Red reflex present cornea intact
• Can see up to 2 ½ feet clearest vision is 8 to
12 inched
• Subconjunctive hemorrhages may be
present due to the pressure from delivery
Head
• Nose midline with patent nares
• Ears aligned with outer canthus of eyes;
pinna well formed, open auditory canal ( low
set ears associated with chromosomal
abnormalities)
• Mouth mucosa pink and moist; tongue
mobile, strong suck, hard/soft palate intact(
Epstein’s pearls may be noted on the gums
or hard palate)
Neck
•
•
•
•
•
Shape typically short with deep folds of skin
Webbing associated with Down Syndrome
Assess for full range of motion
Palpate for abnormal masses
Note the position of the trachea
Chest
• Shape should be cylindrical (bell shaped could be a
sign of underdeveloped lungs)
• Palpate clavicle bones and ribs
• Assess nipples for size, placement and number
• Evaluate respiratory effort and movement
• Auscultate the lung fields and heart sounds
• Unequal breath sounds could be a pneumothorax
Abdomen
•
•
•
•
•
Umbilical cord, 2 arteries 1 vein
Cylindrical with some protrusion
Flat abdomen indicates diaphragmatic hernia
Auscultate for bowel sounds
Suprapubic area palpated for bladder
distention
• Femoral pulses palpated, if unable to locate
could signify coarctation of the aorta
Female Genital and Anal
Assessment
• Term newborn labia majora covers
labia minora and clitoris
• Mucoid vaginal discharge due to
maternal hormones
• Hymental tag may be present
• Annus patent
Male Genital and Anal
Assessment
• Rugae present on the scrotum
• Scrotal edema may be present due to
maternal hormones
• Testes descended
• Check for placement of the meatus
• Dorsal surface- epispadias
• Ventral surface-hypospadias
• Anus should be patent
Extremities
• Assess for full range of motion, symmetry and
signs of trauma
• Spontaneous motion of all extremities should
be present
• Assess muscle tone
• Hyperflexibility of joints associated with Down
Syndrome
• Hips assessed for dislocation
Extremities
• Nail beds pink- persistent cyanosis associated
with hypoxia
• Palms should have normal creases
• Simian crease (transverse palmer) suggests
Down syndrome
• Count digits on extremities (more than five
digits polydactyl-Digits fused together
syndactyl
Spine
• Straight
• Flat
• Shoulders, scapulae and iliac crests
line up in same plane
• Evaluate for dimpling or fissures
• Dimpling associated with spina bifida
Skin
• Assess color
• Check for birth marks, trauma, rashes or
bruises
• Presence of lanugo
• Palpate texture ( ranges from smooth to
peeling)
• Turgor ( elasticity)
Skin Assessment
• Common variations
– Milia
– Mongolian spots
– Birthmarks
• Common problems
– Petechiae
– Blisters, lesions
– Abnormal hair distribution
– Port wine stains
Neurological System
• Infant alert, responsive, strong lusty cry in
a flexed position
• Reflexes provides information on the
system and maturity
• Reflexive behaviors are necessary for
survival and safety
• Absence, weakness or asymmetry
indicates abnormalities
Neurological Reflexes
•
•
•
•
•
•
Sucking
Rooting
Grasping
Extrusion
Tonic neck
Moro
•
•
•
•
•
Stepping
Crawling
Babinski
Truncal incurvation
Blinking
Neurologic System
• Common problems
– Brachial plexus injury (Erb’s palsy)
– Spina bifida
– Anencephaly
– Absent or abnormal reflexes
– Seizure activity
Behavioral Assessment
•
•
•
•
Sleep-wake cycles
Activity
Social interactions
Response to stimuli
Pain Assessment
•
•
•
•
Most common sign crying
Changes in heart rate
Intracranial pressure
Respiratory rate and oxygen saturation
Pain Management
• Nonpharmacologic management:
containment (swaddling),
nonnutritive sucking and
distraction: visual, oral, auditory,
tactile
• Pharmacologic management:
local and topical anesthesia,
Nonopioid analgesia and opioids
Gestational Age Assessment
Ballard Score
• Neuromuscular
maturity
– Posture
– Square window
– Arm recoil
– Popliteal angle
– Scarf sign
– Heel-to-ear
• Physical maturity
– Skin
– Lanugo
– Plantar surface
– Breasts
– Eye and ear
– Genitalia
Infant Nutrition
• American Academy of Pediatrics (AAP)
recommends infants be breastfed
exclusively for first 6 months of life
• Breastfeeding should continue for at least 12
months
• If infants are weaned before 12 months, they
should receive iron-fortified infant formula
Infant nutrition
• Human milk designed specifically for human
infants; nutritionally superior to any alternative
• Breast milk considered living tissue because it
contains almost as many live cells as blood
• Bacteriologically safe and always fresh
• Nutrients in breast milk more easily absorbed
than those in formula
Contraindications of
Breastfeeding
• Maternal cancer therapy/ radioactive isotopes
• Active tuberculosis
• HIV
• Maternal herpes simplex lesion
• Galactosemia in infant
• Cytomegalovirus (CMV)
• Maternal substance abuse
Choosing a Feeding Method
Nurse must provide information to
parents in nonjudgmental manner
and respect their decision
• Provide Factual information about nutritional
and immunologic needs met by human milk
• Potential benefits to infant and mother
• Inherent risks with infant formulas
Choosing a Feeding Method
• Cultural beliefs and practices are a
significant influences
• Immigrants from poorer countries often
choose to formula feed because they
believe it a better, “modern” method
• Others formula feed because they want to
adapt to American culture and perceive it
the custom to bottle feed
Lactation
• Female breast composed of 15 to 20
segments (lobes) embedded in fat and
connective tissues, well supplied with blood
vessels, lymphatic vessels, and nerves
• Within each lobe are alveoli, the milkproducing cells, surrounded by myoepithelial
cells that contract to send the milk forward into
the ductules
Lactation
• Ductules enlarge into lactiferous ducts and
sinuses, where milk collects behind nipple
• Each nipple has 15 to 20 pores through which
milk is transferred to the suckling infant
• After birth, precipitate decrease in estrogen
and progesterone levels triggers release of
prolactin from anterior pituitary gland
Lactation
• Prolactin highest first 10 days
• Gradually decline, but remain above
baseline levels for duration of lactation
• Prolactin produced by infant suckling and
emptying of the breasts
• Breasts never completely empty
• Milk production supply/demand
Lactation
– Oxytocin: other hormone essential to
lactation
– As nipple is stimulated by suckling infant,
posterior pituitary prompted by
hypothalamus produces oxytocin
• Responsible for milk-ejection reflex
(MER), or let-down reflex
– Nipple-erection reflex is integral to
lactation
Lactation
• Colostrum, a clear yellowish fluid birth to
48hrs.
• More concentrated than mature milk
• Extremely rich in immunoglobulins
• Higher concentration of protein and
minerals
• Less fat than mature milk
• Coates and protects the stomach and
intestines from invading organisms
Lactation
• Transition milk 48-72hrs
• High levels of fat, lactose and water
soluble vitamins
• Higher calorie content
• Larger volume
Lactation
• Mature milk produce by 10th to 15th day
• Two types of milk: foremilk and hind milk
• Hind milk higher in fat which is needed for
growth
• 90% water which maintains newborns fluid
balance
• Remaining 10% contains carbohydrates,
proteins and fats
Lactation Frequency/Duration
• A newborns stomach is the size of a
small marble and can hold 5-7 cc’s.
This is matches the amount of
colostrum produced
• From 7-10 days it increases to the
size of a golf ball and can hold 1.5 to
2 oz
Lactation Frequency/Duration
• Newborns nurse on average 8-12
times/24hrs
• Feed by cue signs about every 1-3
hours
• Should have no more than one 4 hr
period
Lactation Education
– Positioning
– Latch-on
– Let-down
– Frequency of
feedings
– Pumping
– Milk storage
– Duration of
feedings
– Supplements,
bottles, and
pacifiers
– Diet
– Breast care
Breast feeding Special
Considerations
• Sleepy baby- use gentle stimulate to
bring to alert state
• Fussy baby- use calming techniques
• Slow weight gain- evaluate
breastfeeding
Breastfeeding
• Engorgement noted when milk comes in and
is bilateral (increase feedings to q2hrs)
• Sore nipples usually result of poor
latch on
• Plugged milk ducts result of inadequate
emptying or underwire bra/apply warm
compresses prior to nursing
• Mastitis infection characterized by sudden
flu like symptoms usually effects only one
breast
Formula-Feeding
• Personal preference
• Influence by significant family
members
• Lack of familiarity with breastfeeding
• Contraindications present
Formulas
•
•
•
•
•
•
•
Ready to feed
Concentrated
Powdered
Cow’s milk–based
Soy-based
Casein/ whey
Amino acid
Formula-Feeding Education
•
•
•
•
•
Types of formula
Formula Preparation
Feeding patterns
Feeding techniques
Bottles preparation
Discharge Assessment
•
•
•
•
•
•
Determine knowledge deficits
Educate on car safety
Importance of Immunizations
Follow care
Newborn hearing screen
Collect blood for PKU