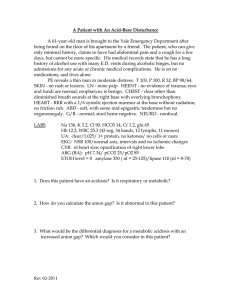
Acid Base Disturbances Ian Chan MS4 Eliza Long R2 Dr. Abdul-Monim Batiha
advertisement

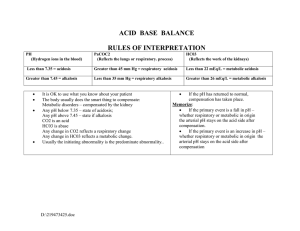
Acid Base Disturbances Ian Chan MS4 Eliza Long R2 Dr. Abdul-Monim Batiha ABG analysis Why do we care ? – – – – Critical care requires a good understanding Helps in the differential and final diagnosis Helps in determining treatment plan Treating acid/base disorders helps medications work better (i.e. antibiotics, vasopressors, etc.) – Helps in ventilator management – Severe acid/base disorders may need dialysis – Changes in electrolyte levels in acidosis (increased K+ and Na+, and decreases in HCO3) Acid buffering The Anion Gap Na – (Cl + HCO3) NaHCO3 + HCL NaCL + H2CO3 NaHCO3 + HX NaX+ H2CO3 Unmeasured cations: calcium, magnesium, gamma globulins, potassium. Unmeasured anions: albumin, phosphate, sulfate, lactate. Gap Acidosis Methanol Uremia Diabetic ketoacidosis Paraldehyde INH Lactic acidosis Ethylene Glycol Salicylate Non Gap Acidosis H: hyperalimentation A: acetazolamide R: RTA D: diarrhea U: rectosigmoidostomy P: pancreatic fistula Metabolic Acidosis Respiratory compensation process takes 1224 hours to become fully active. Protons are slow to diffuse across the blood brain barrier. In the case of LA this will be faster because LA is produced in the brain. The degree of compensation can be assessed by using Winter’s Formula. It is INAPPROPRIATE to use this formula before the acidosis has existed for 12-24 hours. – PCO2 = 1.5 (HCO3) + 8 +/-2. Decreased anion gap Decrease in unmeasured anions – Hypoalbuminemia Increase in unmeasured cations – Hypercalcemia – Hypermagnesemia – Hyperkalemia – Multiple myeloma – Lithium toxicity Metabolic Alkalosis Generation by gain of HCO3 and maintained by abnormal renal HCO3 absorption. This is almost always secondary to volume contraction (low Cl in urine, responsive to NaCl, maintained at proximal tubule) – – – – – Vomiting: net loss of H+ and gain of HCO3. Diuretics: ECFV depletion Chronic diarrhea: ECFV depletion Profound hypokalemia Renal failure: if we cannot filter HCO3 we cannot excrete it. Mineralocorticoid excess: increased H secretion, hypokalemia (Na/K exchanger), saline resistant). Respiratory Acidosis Acute or Chronic: has the kidney had enough time to partially compensate? The source of the BUFFER (we need to produce bicarb) is different in these states and thus we need to make this distinction. Respiratory Acidosis Acute : H is titrated by non HCO3 organic tissue buffers. Hb is an example. The kidney has little involvement in this phase. – 10 mm Hg increase in CO2 / pH should decrease by .08 Chronic: The mechanism here is the renal synthesis and retention of bicarbonate. As HCO3 is added to the blood we see that [Cl] will decrease to balance charges. – This is the hypochloremia of chronic metabolic acidosis. – 10 mm H increase in CO2 / pH should decrease by .03 Respiratory Acidosis Elevation of CO2 above normal with a drop in extracellular pH. This is a disorder of ventilation. Rate of CO2 elimination is lower than the production 5 main categories: – – – – – CNS depression Pleural disease Lung diseases such as COPD and ARDS Musculoskeletal disorders Compensatory mechanism for metabolic alkalosis Respiratory Alkalosis Initiated by a fall in the CO2 activate processes which lower HCO3. Associated with mild hypokalemia. Cl is retained to offset the loss of HCO3 negative charge. Acute response is independent of renal HCO3 wasting. The chronic compensation is governed by renal HCO3 wasting. Causes – – – – – Intracerebral hemorrhage Drug use : salicylates and progesterone Decreased lung compliance Anxiety Liver cirrhosis Sepsis Arterial Blood Gas (ABG) Analysis ABG interpretation Follow rules and you will always be right !! 1) determine PH acidemia or alkalemia 2) calculate the anion gap 3) determine Co2 compensation (winters formula) 4) calculate the delta gap (delta HCO3) ABG analysis Arterial Blood Gas (ABG) –interpretation – Always evaluate PH first Alkalosis – PH > 7.45 Acidosis – PH < 7.35 – Determine anion gap (AG) – AG = NA – (HCO3+ CL) AG metabolic acidosis Non AG acidosis – determined by delta gap – Winters formula Calculates expected PaCO2 for metabolic acidosis PaCO2 = 1.5 x HCO3 + 8 ABG analysis Delta gap – Delta HCO3 = HCO3 (electrolytes) + change in AG Delta gap < 24 = non AG acidosis Delta gap > 24 = metabolic alkalosis – Note: The key to ABG interpretation is following the above steps in order. ABG analysis 33 y/o with DKA presents with the following: – Na = 128, Cl = 90, HCO3 = 4, Glucose = 800 – 7.0/14/90/4/95% – PH = acidemia – AG = 128 – (90 + 4) = 34 – Winters formula – 1.5(4) + 8 = 14 – Delta gap = 4 + (34 – 12) = 26 ABG analysis Answer – AG acidosis with appropriate respiratory compensation – History c/w ketoacidosis secondary to DKA with appropriate respiratory compensation ABG analysis 56 y/o with COPD exacerbation and hypotension and associated diarrhea x 7 days presents with the following ABG: 139 110 20 – 7.22/30/65/10/90% 120 4.0 10 1.5 PH(7.22) = acidemia AG = 139 – (10 + 110) = 19 (nl AG = 8-12) Winters formula – PaCO2 = 1.5 (HCO3) + 8 = 1.5 (10) + 8 = 23 Delta gap – Delta gap = HC03 + change in the AG = 24 – Delta gap = 10 + (19 – 12) = 10 + 7 = 17 – Delta gap = 17 ABG - example Triple disorder – AG acidosis – Incomplete respiratory compensation – Non AG acidosis History would suggest AG acidosis is secondary to hypotension with lactic acid build up and the patient is not able to compensate with his COPD therefore there is no respiratory compensation and the non AG acidosis is secondary to diarrhea with associated HCO3 loss. Look at the pH. – pH < 7.35, acidosis – pH > 7.45, alkalosis Look at PCO2, HCO3• Main pathology will be the change correlates with the pH. • If alkalosis pCO2 will be low or Bicarb high • If acidosis pCO2 will be high or Bicard low • The other abnormal parameter is the compensator response Respiratory or Metabolic • pCO2 - respiratory • Bicarb - metabolic Metabolic Acidosis? Anion Gap? • >12 - ketoacidosis, uremia, lactic acidosis, or toxins • Delta ratio to check for gap and non gap disorders , or metabolic alkalosis happening simultaneously • Normal anion gap - diarrhea OR unknown. If unknown calculate urine anion gap, if positive likely RTA, if neg liekly diarrhea Metabolic Alkalosis If urin Cl is > 20 it is chloride-resistant alkalosis (increased mineralcorticoid activity If <20 chloride responsive alkalosis (vomitting or gastric loss) Example # 1 44 yo M 2 weeks post-op from total proctocolectomy for ulcerative colitis. Na+ 134, K+ 2.9, Cl- 108, HCO3- 16, BUN 31, Cr 1.5 BG: 7.31/ 33 /93 / 16 Example #2 9 yo M presents with N/V. Na 132 , K 6.0, Cl 93, HCO3- 11 glucose 650 BG: 7.27/23/96/11/-8 Example #3 70 yo M s/p lap chole, on the morning of POD #1. Pt received 2L bolus of crystalloid throughout pm for tachycardia. Now with SOB. 7.24 / 60 / 52 / 27 /+3 Example #4 54 yo F s/p mult debridements for necrotizing fasciitis, now on vassopressin to maintain blood pressure BG - 7.29/40/83/17/-6 Example #5 35 yo M involved in crush injury, boulder vs body. Na 135 , K 5.0, Cl 98, HCO3- 15 BUN 38, Cr 1.7, CK 42,346 BG: 7.30/32/96/15/-4 Example #6 4 wks M with projectile emesis Na: 140, K:2.9, Cl: 92 7.49/40/98/30/+6