ABG Interpretation - Calgary Emergency Medicine
advertisement
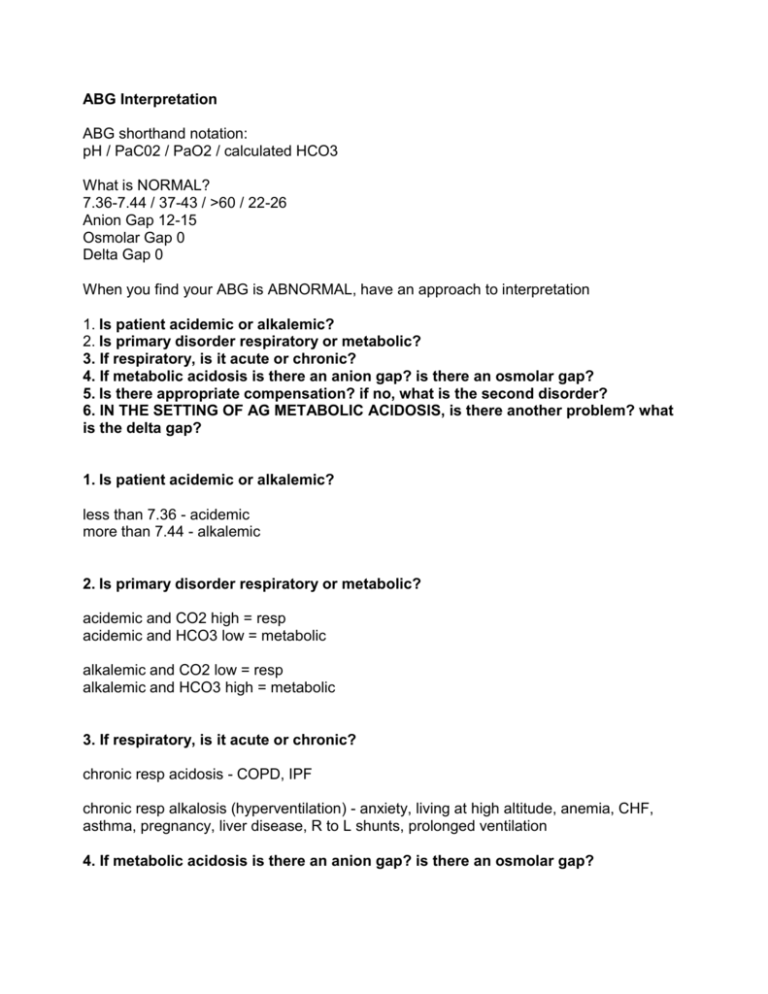
ABG Interpretation ABG shorthand notation: pH / PaC02 / PaO2 / calculated HCO3 What is NORMAL? 7.36-7.44 / 37-43 / >60 / 22-26 Anion Gap 12-15 Osmolar Gap 0 Delta Gap 0 When you find your ABG is ABNORMAL, have an approach to interpretation 1. Is patient acidemic or alkalemic? 2. Is primary disorder respiratory or metabolic? 3. If respiratory, is it acute or chronic? 4. If metabolic acidosis is there an anion gap? is there an osmolar gap? 5. Is there appropriate compensation? if no, what is the second disorder? 6. IN THE SETTING OF AG METABOLIC ACIDOSIS, is there another problem? what is the delta gap? 1. Is patient acidemic or alkalemic? less than 7.36 - acidemic more than 7.44 - alkalemic 2. Is primary disorder respiratory or metabolic? acidemic and CO2 high = resp acidemic and HCO3 low = metabolic alkalemic and CO2 low = resp alkalemic and HCO3 high = metabolic 3. If respiratory, is it acute or chronic? chronic resp acidosis - COPD, IPF chronic resp alkalosis (hyperventilation) - anxiety, living at high altitude, anemia, CHF, asthma, pregnancy, liver disease, R to L shunts, prolonged ventilation 4. If metabolic acidosis is there an anion gap? is there an osmolar gap? AG = Na - Cl - HCO3 (normal is 12-15) correct for albumin (every decrease of 10 in albumin, increase the gap 3) OG = measured serum osm - (Na x 2, Glu, BUN) 5. Is there appropriate compensation? if no, what is the second disorder? (you can not OVER compensate) PROBLEM acute resp acid acute resp alk chronic resp acid chronic resp alk CO2 up 10 down 10 up 10 down 10 HCO3 up 1 down 2 up 3 down 5 met acidosis met alk down 10 up 10 down 10 up 7.5 6. IN THE SETTING OF AG METABOLIC ACIDOSIS, is there another problem? you CAN NOT have more than one respiratory problem you CAN have more than one metabolic problem: AG Met acid + Met Alk AG Met acid + non AG Met acid you CAN have a respiratory problem and a metabolic problem (and even a secondary metabolic problem on top of that) look at delta gap - anion gap delta versus bicarb delta normally in AG Met Acidosis, the number of anions above 14 should equal the number of bicarb below 24 (calculated anion gap - 14) versus (24 - measured HCO3) for example 1. calculated anion gap of 23 is an anion delta of 9 (measured 23 - normal 14 = delta of 9) 2. measured bicarb of 15 is a bicarb delta of 9 ( normal 24 - measured 15 = delta of 9 ) normally the anion delta is equal to the bicarb delta if they are NOT equal, there is a second problem... if Bicarb delta is less than the anion gap delta = metabolic alkalosis as well if Bicarb delta is more than the anion gap delta = non AG metabolic acidosis as well Anion Gap Acidosis addition of exogenous acids or creation of endogenous acids Methanol/ Metformin Uremia Diabetic/starvation/alcoholic Ketoacidosis Paraldehyde / Phenformin Ischemia / iron / isoniazid Lactic acidosis Ethylene glycol (antifreeze) Cyanide / Carbon Monoxide ASA Toluene Solvents Pearls most common: ketoacidosis, lactic acidosis, ASA (IF ruled out investigate toxic alcohols) ASA not only results in AG met acidosis but also Resp alkalosis a low glucose does not rule out ketoacidosis: look out for starvation, dehydration, alcohol consider cyanide and carbon monoxide in inhalation and burn victims don’t be fooled by normal Osat and PaO2 - carbon monoxide needs carboxyhemoglobin isoniazid (aka inh) antidote is vit b6...think about it in refractory seizures (esp high risk TB populations) reduced arterial-venous oxygen sat difference (<10%) suggests cyanide toxicity cyanide antidote is induced methemaglobinemia ethylene glycol or methanol antidote is etoh or Fomepizole if you suspect Iron OD, get an AXR - pills may show up on the flat plate! ethylene glycol in urine will fluoresce using a Wood’s lamp - easy bed side test! calcium oxalate crystals in urine are sign of possible ethylene glycol ingestion Non-anion gap acidosis inability to excrete H+ or loss of HCO3 Fistulae (pancreatic - duodenal, ureter - enteric) diarrhea carbonic anhydrase inhibitors diuretics saline (large amounts) RTA parenteral nutrition Pearls most common loss of bicarb by GI or kidneys - diarrhea - tubular acidosis or renal failure - Metabolic Alkalosis - Saline Responsive -either loss of H+ or contraction (volume contraction around constant HCO3) -Urine Cl <10 Gastric suction Vomiting Diuretics give Saline, gets better Metabolic Alkalosis - Non Saline Responsive -retention of HCO3 associated with mineralcorticoid excess -Urine Cl>20 Hyper aldosteronism Exogenous steroids adenocarcinomoa Bartter’s syndrome Cushing’s syndrome VBG vs ABG? correlation does not equal accuracy studies show excellent correlation of ph, pco2, calc hco3 between abg and vbg but the accuracy was the problem!-the differences between the two were outside the range noted to be sig by emerg docs “Can peripheral venous blood gas replace arterial blood gases in ED patients” cjem Jan 2002 however, most notable delta is in the post arrest patient that being said, most problems in the ED can be sorted out using vbg. It’s easier to get and less painful for the patient. perhaps the only time for abg is when you cant get venous access or when u want to qualify for home o2 or in post arrest patients.