KER UNIT - Mayo Clinic Shared Decision Making National

The Chest Pain Choice
Decision Aid: a Randomized
Trial
ISDM Conference
Maastricht, June 2011
E Hess, M. Knoedler, N. Shah, J
Kline, M Breslin, M Branda, L
Pencille, B Asplin, D Nestler, A
Sadosty, H. Ting, M. Montori
Knowledge and Evaluation Research Unit
Mayo Clinic College of Medicine
MN
Foundation for Informed Medical
Decision Making
AHA Fellow-to-Faculty Transition Award
Background
• Chest pain 2 nd most common complaint in U.S. Emergency
Departments
> 6 million patients annually
• 4% of ACS inappropriately discharged from ED
Pope, NEJM, 2000
• Large #’s of low risk patients admitted for prolonged observation and cardiac stress testing
• False positive test results, unnecessary procedures, cost
Background
• Kline and colleagues developed a quantitative pretest probability calculator
Kline JA, BMC Med Informed Decision Making, 2005
• Prospectively validated QPTP calculator in 3
Academic EDs
Mitchell AM, Kline JA, Annals of Emergency Medicine, 2006
• Demonstrated efficacy of QPTP calculator in
RCT
Kline JA, Annals of Emergency Medicine, 2009
4
Background
Decision Aids:
knowledge (by 15 of 100, 95% confidence interval 12-19%)
% patients with realistic perceptions of the chances of benefits and harms by 60% (40-
90%)
uncertainty related to feeling uninformed (by 8 of 100 (5-12)
% passive patients in decision making by 30% (10-50%)
% remaining undecided after counseling by 57% (30-70%)
O’Connor, Cochrane Database of Systematic Reviews, 2009
Hypothesis
Facilitating a patient-centered discussion regarding the short-term risk for ACS in otherwise low-risk chest pain patients will:
patient knowledge
patient engagement
Safely resource use
Objectives
(1) To design a DA for use in patients at low risk for ACS
(2) To test the DA in a randomized trial
Methods
Decision Aid Design
• Incorporate QPTP output in a literacy-sensitive DA, describe rationale of evaluation, list management options in value-neutral fashion
• Iteratively test DA in patient encounters
• Refine DA based on input from patients, clinicians, and investigative team thematic saturation
Breslin, Mullan, Montori Patient Educ Counseling 2008
Methods: Clinical Trial
• Design: single-center; allocation concealed by password-protected, web-based randomization
• Setting: Academic ED in Rochester, MN with
73,000 annual patient visits; 10-bed observation unit
• Eligibility:
–Included: Adults with chest pain considered for EDOU admission
–Excluded: +troponin, known CAD, cocaine use within
72 hrs, unable to provide informed consent or use decision aid
Outcome measures
• Decision quality
– Patient knowledge**
–Degree of patient participation (OPTION scale)
–Decisional conflict (DCS)
–Trust in physician (TPS)
• Quantitative
–Safety endpoint: 30-day MACE*
–Resource use
• Rate of cardiac stress testing in EDOU
• 30-day rate of stress testing
Statistical analysis
• Power: 200 patients
–90% power to detect > 25% ↑ in mean knowledge
–95% power to detect a 20% ↓ in proportion of patients who underwent stress testing in EDOU
• Hypothesis testing: chi-square, Fisher’s exact, t-test or Wilcoxon rank-sum as appropriate
• Intention-to-treat principle followed
Results
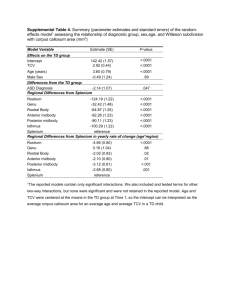
Baseline Characteristics
P-value Variable
Mean age
Female
HTN
Hyperlipidemia
Family history of premature CAD
Mean PTP of ACS
Intervention Control
(n=101)
54.5
59%
45%
45%
14%
3.2%
(n=103)
54.9
61%
28%
39%
12%
3.3%
0.81
0.97
0.01
0.46
0.61
0.81
Knowledge and Participation
Variable Intervention
(n=101)
Control
(n=103)
6 knowledge questions
OPTION score
3.6
51.4
3.0
32
Mean diff
(95% CI)/ p-value
0.67
(0.34, 1.0)
< 0.0001
Decisional Conflict* and
Physician Trust
Variable Intervention Control
(n=101)
22.3
(n=104)
43.3
Decisional conflict (DCS)
Trust in physician (TPS)
83.4
79.3%
Mean diff
(95% CI)
-13.6
(-19.1, -8.1)
4.1
(-1.4, 9.6)
*Conflict related to feeling uninformed
Acceptability to Patients
P-value Variable Intervention
Amount of information
(n=101)
93%
(just right)
Clarity of information
(extremely clear)
Helpfulness
(extremely helpful)
Would recommend to others
62%
53%
75%
Control
(n=104)
80%
37%
34%
45%
0.0051
<0.0001
<0.0001
<0.0001
Provider experience
Variable Intervention
(n=101)
59%
Control
(n=104)
20% Strongly recommend way information was shared
Want to present other diagnostic information in same way
64% 28%
P-value
<0.0001
<0.0001
Safety
Variable
Revascularization
MI
Death
MACE within 30 days of discharge
Intervention Control
(n=101)
3%
1%
0
0
(n=104)
2%
0%
0
0
P-value
0.68
0.49
NA
NA
Resource use
Variable
Stress test in
EDOU
Stress test performed within 30 days
Follow-up as outpatient
Intervention
(n=101)
58%
75%
39%
Control
(n=104)
77%
91%
9%
P-value
<0.0001
0.02
<0.0001
Limitations
• Single center
• Insufficient power to demonstrate safety
Conclusions
Summary of impact of DA
Variable
Patient knowledge
Patient participation
Decisional conflict
Direction of difference
↑
↑
Physician Trust
Acceptability
Safety
Resource use
↓
↔
↑
↔
↓
Lessons learned
• Integration in process of care challenging
• Care process redesign required??
• Feasibility of definitively demonstrating patient safety?
• Use of DA in emergency department requires reliable access to outpatient follow-up
Future Directions
• Identification of factors that promote or inhibit uptake of SDM in acute setting
• Prospective multicenter randomized trial