Rehabilitation following a burn injury
advertisement

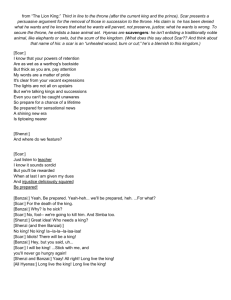
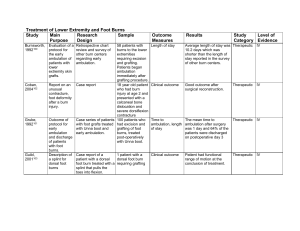
REHABILITATION FOLLOWING A BURN INJURY Sunny Chirieleison, MPT UNM Burn Center Adult & Pediatric Injury from tragedy… hope! Rehabilitation begins on the day of admission… • • • • • • • • Evaluation Assessment Wound care Prevention of contractures Positioning/splinting ROM Edema control Mobility training • • • • • Gait training Strengthening Desensitization ADL training ↑ endurance, coordination, balance • Scar management • Pt/family education Burn Classification Depth Healing Time Scar formation Appearance Current Common terminology terminology Sensation Superficial First degree Dry (no blisters) VERY PAINFUL 3-7 Days – generally no skin graft needed Pigment changes only Superficial partial thickness Second degree VERY PAINFUL 7-21 Days generally no skin graft needed Minimal scarring and pigment changes Red (blanches) Blisters, weeping Burn Classification (cont.) Depth Current terminology Common terminology Deep partial thickness Full thickness Healing Time Scar formation Appearance Sensation Second or third degree Variable color (mottled white, pale pink, cherry red with decreased blanching) VERY PAINFUL 21-35 Daysmay require skin graft Will have scarring and pigment changes Third or fourth degree Leathery with variable color (white, waxy, pearly, dark, charred – no blanching) Decreased or no pain Can require months to heal – probable skin graft Will have significant scarring – likely hypertrophic *Contracture Prevention* • Splints (& wearing schedules) – Daily assessment of ROM • Positioning – – – – Elevation to minimize edema Prevent tissue destruction Maintain soft tissues in an elongated state Influence scar formation • ↑ active movement (esp. hands & ankles) • Exercise program • Compression The position of comfort is most often the position of contracture Areas at ↑ risk for contracture • Neck • Axilla • Hand • Require special attention by the therapist to prevent long term impairments and functional limitations Anterior Neck Burns • NO Pillows under head • Frequent Cervical ROM • Use cervical collar (soft or rigid) for positioning • If tolerated hyperextension with head over edge of mattress – (generally only in ICU when pt sedated and monitored) This deformity could have been be prevented… Axillary Burns • POSITIONING – In ICU patient can be positioned using pillows or bedside tables 2° to sedation • Airplane splint – Monitor sensation changes – adjust splint PRN • ROM • Patient/family education Dorsal Hand Burns • Splint ASAP • Exposed tendons immobilized in a position of slack to prevent rupture – and future Boutonniere deformity • ROM – isolated joint flexion (no full fist) until healed or grafted Optimal position for dorsal hand burns Boutonniere Deformity Rupture of central extensor tendon or lateral bands Indications for splint use • • • • • Prevention of contractures Protection of a joint or tendon Immobilization following a skin graft Decreased ROM Maintenance of ROM achieved during an exercise session or surgical release • Poor patient compliance • Dorsal hand burns should be splinted as soon as possible to prevent deformity !!! Scar Management / prevention • Remember: fibroblasts work a 24 hour shift – every minute spent on scar management is worthwhile • Imagine scar tissue as cement – Early on, wet cement can be poured and molded. Once it dries, it is as hard as stone. -a little work today will result in major changes down the road (long term benefits) Hypertrophic Scar Hypertrophic Scar • Risk factors – Age of patient – younger more likely to develop scar 2° to growth factor – Depth of injury – involvement of dermis – Length of time to heal (>21 days) – h/o of hypertrophic scar formation – Genetic predisposition UNM Burn Center: from tragedy… hope! Custom Compression Garments Adult & Pediatric Injury Final Thoughts • Early splinting and positioning are crucial to minimize impairments and maximize function – Many impairments are preventable! • Burn patients will require long-term follow-up for ROM, scar management, etc., (even if initial ROM and mobility are normal) to maximize functional outcomes • Please remember special considerations (hands, LE’s, and areas at high risk for contracture)… and if in doubt consult with Burn Therapist THANK YOU!!! Questions… one child burned, is one child too many! Sunny Chirieleison, MPT UNM Burn Center Adults & Pediatrics from tragedy… hope!