Maternal_Collapse_in..
advertisement

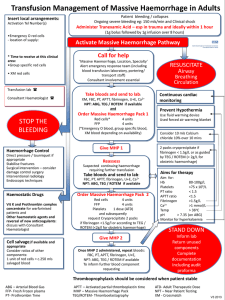
Maternal Collapse in labour ward Dr . J. Edward Johnson. M.D., D.C.H. Asst. Professor , Dept. of Anaesthesiology, KGMCH. DISCUSSION CAUSES OF MATERNAL COLLAPSE • • • • • • • • Haemorrhage (APH, PPH) Pul.Embolism Amniotic Fluid Embolism Pre-eclampsia/eclampsia Cardiac (Valvular HD) Syncope Sepsis Respiratory Causes of Collapse • 4 H’s: Hypoxia Hypovolaemia (bleeding/block) Hypothermia Hypo/hyperkalaemia (metabolic) • 4 T’s: Thromboembolic (PE or AFE) Toxic/therapeutic (local anaesthetic) Tension pneumothorax Tamponnade • Eclampsia Leading causes of Direct Deaths (Mortality rates/Million Maternities) Postpartum Hemorrhage “Obstetrics is Bloody Business”* *Cunningham, et. al: Williams Obstetrics, 21st ed., 2001 DIAGNOSIS OF ETIOLOGY Postpartum Hemorrhage Diagnosis of Causes Postpartum Hemorrhage Retained placenta Placenta Accreta Uterine atony Vaginal and cervical laceration DIC, AFE Factor disorder Uterine rupture / Uterine inversion MANAGEMENT RESUSITATION OF Haemorrhagic Shock & Cardiac Arrest -(CPR) RESUSITATION Haemorrhagic Shock Classification of Haemorrhage Class Acute Blood Loss % Lost 1 900cc 15 2 1200-1500cc 20-25 3 1800-2100cc 30-35 4 2400cc 40 Baker R, Obstet Gynecol Annu, 1997 ASSESSMENT OF BLOOD LOSS AFTER DELIVERY • • • • • Difficult Mostly Visual estimation (So, Subjective & Inaccurate) Underestimation is likely Clinical picture -Misleading Our Mothers-Malnourished, Anaemic, Small built, Less blood volume SYMPTOMS & SIGNS Blood loss Systolic BP Signs & Symptoms (% B Vol) ( mm of Hg) 10-15 Normal postural hypotension 15-30 slight fall PR, thirst, weakness 30-40 60-80 40+ 40-60 pallor,oliguria, confusion anuria, air hunger, coma, death Recognition is late - >30% B Vol loss Modified Early Warning Scoring System (MEWS) MEWS calculated from 5 physiological variables • • • • • Mental response Pulse rate Systolic BP Respiratory rate Temperature Modified Early Warning Scoring System (MEWS) The senior nurse would call the doctor for three or more of the following criteria: • Respiratory rate of ≥25 or <10 breaths per minute. • Arterial systolic blood pressure of <90mmHg. • Heart rate of ≥110 or <55 beats per minute. • Not fully alert and orientated. • Oxygen saturation of <90 per cent. • Urine output over the last four hours of <100ml. • Respiratory rate ≥35 breaths per minute or a heart rate ≥140 beats per minute. Vigilance is great, but you have to remember that studies show the half-life of vigilance is about 15 minutes. Author unknown DO NOT UNDERESTIMATE BLOOD LOSS Clinical Features of Shock System Early Shock Late Shock CNS Altered mental states Obtunded Cardiac Tachycardia Cardiac failure Orthostatic hypotension Arrhythmias Hypotension Renal Oliguria Anuria Respiratory Tachypnea Tachypnea Respiratory failure Hepatic No change Liver failure Gastrointestinal No change Mucosal bleeding Hematological Anemia Coagulopathy Metabolic None Acidosis Hypocalcemia Hypomagnesemia Goals of Therapy • Maintain the following: Systolic pressure >90mm Hg Urine output >0.5 mL/kg/hr Normal mental status • Eliminate the source of hemorrhage • Avoid overzealous volume replacement that may contribute to pulmonary edema Management of Obstetrical Hemorrhage Oxygen by mask 10 liter/min. – to keep O2 saturation > 94% 1st IV Line: Ringer Lactate with Pitocin 20-40 units at 1000 ml/ 30 minutes 2nd IV Line: 18 G IV: warm RL - administer wide open Sample blood; CBC, fibrinogen, PT/PTT, platelets, T&C and order 4u PRBCs Monitor I&O, urinary Foley catheter Get help Senior Obstetrician, Anesthesiologist, Interventional Radiology, Intensivist, Haemotologist etc. Management of Obstetrical Hemorrhage LR or NS replaces blood loss at 3:1 Volume expander 1:1 (albumin, hetastarch, dextran) Anticipate Disseminated Intravascular Coagulapathy (DIC) Verify complete removal of placenta, may need ultrasound Inspect for bleeding -episiotomy, laceration, hematomas, inversion, rupture Emperic transfusion -2 u PRBC; FFP 1-2 u/4-5 u PRBC -Cryo 10 u, -Uncrossed (O neg.) PRBC – For emergency Warm all blood products and I.V.infusions -prevent hypothermia, coagulopathy, arrhythmias Platelets Random Donor Apheresis Pooled 4-8 units, ABO + Rh compatible Expire 4 h after pooling Single donor Expire 4 h after released 3-5 day survival in vivo (in DIC) FFP (contains all coag factors) PT, PTT > 50% increase or INR > 1.5 Warm Spin Cryoprecipitate (VIII, XIII, Fibrinogen, VW) Fibrinogen 5 mgldL Blood Component Therapy Fresh Frozen Plasma – INR > 1.5 - 2u FFP – INR 2-2.5 - 4u FFP – INR > 2.5 - 6u FFP Cryoprecipitate ( 1u/ 10Kg ) – Fibrinogen < 100 mg/dl – 10u cryo – Fibrinogen < 50 mg/dl – 20u cryo Platelets – Platelet. count. < 100,000 – 1u plateletpheresis – Platelet. count. < 50,000 – 2u plateletpheresis Blood Component Therapy Blood Comp Contents Volume (ml) Effect Packed RBCs RBC, Plasma 300 Inc. Hgb by 1 g/dl Platelets Platelets, Plasma 250 Inc. count by 25,000 FFP Fibrinogen, antithrombin III, clotting factors, plasma 250 Inc. Fibrinogen 10 mg/dl Cryoprecipita te Fibrinogen, VonWillebrand F, Factor V111, X111, Fibronectin 40 Inc. Fibrinogen 10 mg/dl Target Values • • • • • • • Maintain systolic BP>90 mmHg Maintain urine output > 0.5 ml per kg per hour Hct > 21% Platelets > 50,000/ul Fibrinogen > 100 mg/dl PT/PTT < 1.5 times control Repeat labs as needed – every 30 minutes Management of Major Obstetric Haemorrhage Recombinant factor VIIa (rFVIIa) 1. rFVIIa works at the site of vascular injury, where tissue factor (TF) is expressed and activated platelets aggregate. rFVIIa The fibrin clots formed in the presence of of a high thrombin concentration have a different architecture that is stronger and more resistant to degradation by fibrinolytic enzymes. Fibrin Fibrinogen Thrombin Va rFVIIa In pharmacological doses rFVIIa binds directly to the activated platelet surface. Xa X Prothrombin Here it enhances localized thrombin generation and the formation of a stable fibrin-based clot. Recombinant factor VIIa • It is not licensed for use in obstetric haemorrhage and there have been no randomised contolled trials for its use in this situation • The dose is approximately 90μg/kg. • Its efficiacy is dependent on -normothermia, -non-acidotic milieu -adequate levels of fibrinogen (> 1.0-1.5gr) -platelets (> 50,000) • A relatively early itervention to control PPH appears to be crucial for the success of rVIIa Management of Major Obstetric Haemorrhage - rFVIIa 1. rFVIIa will not replace ligatures in controlling bleeding from damaged or torn vessels. 2. To be effective there must be adequate circulation delivering platelets and fibrinogen to the site of bleeding. 3. You should make your best efforts to correct acidosis and hypothermia. TREAT THE ETIOLOGY OF PPH MANAGEMENT OF PPH TEAM - Obstetrician, - Anesthesiologist, - Haematologist and - Blood Bank Correction of hypovolaemia Ascertain origin of bleeding Ensure uterine contraction Surgical management Management of special situation Massive Obstetric Haemorrhage Treatment Medical Surgical Blood Component Therapy Post Treatment Care Massive Obstetric Haemorrhage Medical Volume Replacement (Crystalloid,Colloid) Blood (O –tive, Group Specific, X Matched) Coagulation Support (FFP, Cryoprecipitate, Platelets) Inotropic Support Uterine Massage / Compression Uterotonic Agents (Syntocinon ,Ergotamine, Carboprost Misoprostol ) Temperature Active Warming Massive Obstetric Haemorrhage Surgical • EUA Repair • Uterine Tamponade (78%) • B-Lynch Suture (81%) • Arterial Ligation • Radiological Arterial Embolisation • Hysterectomy ( 12%) Treatment of PPH: Hysterectomy A conservative option should be quickly efficacious The addition of successive conservative approaches is hazardous - Risk of delaying radical treatment Early Decision Placenta accreta is a frequent cause of failure of conservative Treatments Hysterectomy may be a life-saving procedure in case of - Failure of conservative approach - Uterine rupture - Placenta accreta Selective Angiographic Embolization (SAE) Strategically difficult in many centers Pulmonary Embolism Pulmonary Embolism Pulmonary embolism, along with amniotic fluid embolism, accounts for the leading cause of maternal mortality in the United States (Koonin, et al; MMWR) DVT: Key Facts • 40% of asymptomatic patients with DVT have radiographically documented pulmonary embolism • DVT of pelvic venous system is often an asymptomatic condition until clinical pulmonary embolism develops • Untreated pulmonary embolism mortality is up to 30%. Treated mortality is 3% (Moser et al, 1994; Cunningham et al, 1997; Toglia & Weg, 1996) The Wells score clinically suspected DVT - 3.0 points alternative diagnosis is less likely than PE - 3.0 points Tachycardia - 1.5 points immobilization/surgery in previous four weeks - 1.5 points history of DVT or PE - 1.5 points hemoptysis - 1.0 points malignancy (treatment for within 6 months, palliative) - 1.0 points Traditional interpretation Score >6.0 - High Score 2.0 to 6.0 - Moderate Score <2.0 - Low Alternate interpretation Score > 4 - PE likely. Consider diagnostic imaging. Score 4 or less - PE unlikely. Consider D-dimer to rule out PE. Diagnosis of Pulmonary Embolism • • • • • • • • D-dimer (0-300 ng/ml as normal) Chest X-ray ECG Arterial blood gas Ventilation-perfusion scintography Angiography Thoracic enhanced CT (64 slices MDCT) Extremity Doppler Chest X-Ray Findings in PE: • Hampton’s Hump: pleural based density at CPJ • Westermark’s Sign: peripheral aligemia with proximal vessel dilatation • Most common finding is normal X-Ray (30%)! ECG Changes in PE: • p-pulmonale, RBBB, RAD • S1 Q3 T3 classic signs -large S wave in lead I -a large Q wave in lead III and -an inverted T wave in lead III • New Onset A-Fib • Most common finding is normal (or sinus tach) ECG Radiographic Diagnosis of Pulmonary Embolism During Pregnancy: • Ventilation/Perfusion (V/Q) Scanning • Pulmonary Angiography • Spiral/Helical CT Treatment- Pulmonary Embolism in Pregnancy • Anticoagulation is mainstay of pharmacotherapy • Supportive care should not be forgotten during the rush to diagnose and treat Venous Air Embolism During the repair of hysterotomy wound Exteriorization of the uterus and traction on the wound edges increases the risk Trendelenburg position to be avoided Abdominal and Uterine incision always below heart CVP, High Uterine wound Air Embolism Amniotic Fluid Embolism “Anaphylactoid syndrome of pregnancy" Amniotic Fluid Embolism AFE is an - unpredictable - unpreventable and -an untreatable (for the most part) obstetric emergency Amniotic Fluid Embolism • Frequency- 1/15,000 - 1/20,000 Pregnancies • Catastrophic Consequences • Multisystem Collapse • Mortality Quoted as High as 80% (Probably Lower Now) First Victim of AFE 1817 an obstetrician named Sir Richard Croft The patient was Princess Charlotte of Wales She died, presumably from an undetected post-partum haemorrhage Condemnation and grief Croft experienced led him to commit suicide Charlotte's pregnancy is known in medical history as “the triple obstetrical tragedy”. Pathophysiology- Animal Data: • Amniotic fluid thought to be composed of some abnormal factor or mediator • Factor is heat stable • Factor is soluble? • Possible relationship with anaphylactoid phenomenon • Abnormal components such as meconium may play a role (Hankins, 1995; Hankins, et al, 1993; Clark, 1995) Situations Related or NOT Related to AFE: • Uterine Hyperstimulation- AFE registry suggests that hyperstimulation is EFFECT rather than cause of AFE • Oxytocin use- NOT RELATED • Drug Allergy and/or Atopy- RELATED, with 41% of patients in AFE registry with allergies • Normal labor!!?? (Clark, 1997) Amniotic Fluid Embolism Mechanism Clinical presentation The classic clinical presentation of the syndrome has been described by five signs that often occur in the following sequence: (1) Respiratory distress (2) Cyanosis (3) Cardiovascular collapse cardiogenic shock (4) Hemorrhage (5) Seizure & Coma. Diagnosis The presence of squamous cells in the pulmonary arterial blood obtained from a Swan-Ganz catheter once considered pathognomonic for AFE is neither sensitive nor specific The monoclonal antibody TKAH-2 may eventually prove more useful in the rapid diagnosis of AFE. National registry’s criteria for diagnosis of amniotic fluid embolism AFE- Differential Diagnosis • • • • • • Pulmonary Embolism Venous Air Embolism Myocardial Infarction Eclampsia Anaphylaxis Local Anesthetic Toxicity Management of AFE RECOGNITION FIRST STEP IMMEDIATE MEASURES : - Set up IV Infusion, -O2 administration. - Airway control endotracheal intubation maximal ventilation and oxygenation. LABS : CBC,ABG,PT,PTT,fibrinogen,FDP. Management of AFE Treat hypotension, increase the circulating volume and cardiac output with crystalloids. After correction of hypotension, restrict fluid therapy to maintenance levels since ARDS follows in up to 40% to 70% of cases. Steroids may be indicated (recommended but no evidence as to their value) Dopamine infusion if patient remains hypotensive (myocardial support). Other investigators have used vasopressor therapy such as ephedrine or levarterenol with success (reduced systemic vascular resistance) Treat Coagulopathy RESUSITATION OF CARDIAC ARREST Cardiopulmonary Resuscitation in Pregnancy If you think that this will never happen to you, you are wrong! Being an Obstetrics provider is no excuse not to be CPR literate. Non-Obstetrics providers may know more than you do about CPR, but they may know little or nothing about pregnancy, fetal evaluation, etc. Possible Outcomes • Mother and babies die or brain-damaged • Mother and babies intact • Mother intact, babies die or impaired • Mother brain damaged, babies intact • Family takes legal action against hospital, anesthesiologist, obstetrician Cardiac Arrest in Pregnancy What happens next depends on: Maternal diagnosis Fetal condition and maturity How rapidly and appropriately medical and nursing personnel respond Resources available in hospital Cardiac Arrest in Pregnancy: Complicated by Physiologic Changes Rapid development of hypoxia, hypercapnia, acidosis Risk of pulmonary aspiration Difficult intubation AORTO-CAVAL COMPRESSION by pregnant uterus when mother supine Changes greater in multiple pregnancy, obesity Cardiac Arrest in Pregnancy: Special Problems • Cardiac output during closed chest massage in CPR is only ~ 30% normal • Cardiac output in the supine pregnant woman is decreased 30-50% due to aortocaval compression • Combined effect of above: There may be NO cardiac output! MRI Scan • NORMAL • Aortocaval Compression- occurs during second 1/2 of pregnancy Cardiff Resusitation Wedge Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiac Care An international evidence and science-based consensus: What’s new or different? Anticipatory treatment of cardiac arrest Emphasis on Automatic External Defibrillators (AEDs) Competent bag-mask ventilation - may be better than intubation attempts Use of amiodarone 300 mg IV (in place of lidocaine*) Vasopressin 40 mg x 1 (alternative to repeated doses epinephrine 1 mg IV every 3-5 min*) Family presence during resuscitation *Insufficient evidence to support efficacy American Heart Association, 2000 Why is Urgent Delivery Indicated? Maternal brain damage may start at ~ 4-6 min What is good for mother is usually good for baby Most intact newborns delivered within 5 min Closed chest massage is less effective with time CPR may be totally ineffective before delivery: Many reports of mother “coming back to life” after delivery Advantages of Early Delivery Aortocaval compression relieved: Venous return , Cardiac output Ventilation improved: -Functional Residual Capacity -Oxygenation improved Oxygen consumption , CO2 production Improved maternal and newborn survival The Cesarean Delivery Decision - Not an Easy One! • Has 3-4 min passed since cardiac arrest? • Has the mother responded to resuscitation? • Was resuscitation optimal - can it be improved? “Perimortem” Cesarean Section Start by 4 minutes, deliver by 5 minutes (From the time of Arrest) Perform operation in patient’s room: Can move to OT after delivery Don’t worry about sterility Vertical abdominal incision quickest Prepare for uterine hypotonia and bleeding Optimal Outcome Immediate CPR ACLS IS THIS REALISTIC OUTSIDE THE OR? Early intubation Left Uterine displacement Start Cesarean by 4 min Delivery by 5 min Essential Equipment (Should be available in Labour ward) Pulse oximeter Cardiac arrest cart; defibrillator Automatic Electric Defibrillator (AED)? Cesarean section instruments Difficult intubation equipment (including LMA, jet ventilator, fiberoptic laryngoscope) Thoracotomy instruments Blood warmer and rapid fluid infuser Central venous and arterial line equipment Common Problems in Obstetrics Denial of problem delay in response Communication errors Obstetric staff not prepared for catastrophes Inadequate response from transfusion or labs No specialty in-house surgeons (e.g., for airway, vascular, cardiac problems) No OB-ICU facilities Family Support When the mother and infant are gravely ill, keep their family members well informed. Be cool and calm while communicating with the family members Allow as much access to the loved ones as possible. Get informed consent at each stage. WORK FORCE & PROTOCALS • In such emergency situation It appears important to: – Streamline the workflow – Co-ordinate the efforts of different specialities ІObstetrician ІІAnaesthetist • Assessment of patient condition • Resuscitation – General condition, BP, pulse, revealed blood –Maintenance of haemodynaemic status of patient loss – Fluid & blood product replacement • Assessment of blood loss • Estimation of blood loss – Estimation of blood loss is notoriously –More experienced in blood loss estimation difficult & inaccurate • Anaesthesia • Control bleeding – Induction a & maintenance of anaesthesia –Manual pressure, oxytocic, operative • Drug administration procedures 5 Elements in management ІІІOperating Theatre • Preparation for emergency operation • Assistance in operative procedures – Scrub nurse to conduct operation – Assist in administration of anaesthesia – Assist in fluid, blood product and drug administration ІV Radiologist • Control of haemorrhage – Cannulisation of pelvic vessels – Embolization of pelvic vessels to control bleeding VPaediatrican • Resuscitation of newborn – Stand by delivery – Immediate resuscitation of newborn – Escort newborn to NICU Multidisciplinary Team Approach Obstetrician Hospital Administration Neonatology Risk Management Anesthesiology PATIENT Blood Bank Social Work Nursing Radiology Hemorrhage protocol Logistics • Protocal should be specific for your hospital (Hospital specific) • Protocal depends upon your hospital infra- structure and the availability of Resource persons •Determine the hemorrhage response team •Determine team member responsibilities • Update and modify your Protocal periodically • Conduct periodic Emrgency drill Early Haemorrhage Early Recognition Early intervention Hypotention Prevent shock Shock Resusitation Late intervention CPR Cardiac Arrest Deliver the baby < 5mts Summary Successful treatment requires: Communication Preparedness Multidisciplinary Team Approach Hospital Hemorrhage Protocol A Good understanding between MULTIDISCIPLINARY TEAM IS A MUST FOR THE SUCCESS Intelligent anticipation, skilled supervision, prompt detection and effective institution of therapy can prevent disastrous consequences .