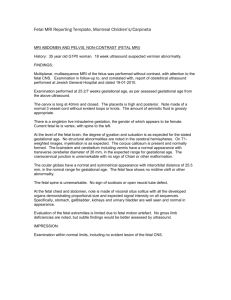
ObUsConcepts
advertisement

Jan Charmaine Almonte-Saret M.D., FPOGS, FPSUOG equal or less than 13 weeks - - Indications and advantages: confirmation of intrauterine pregnancy/ early pregnancy failure best estimation of G.A. Evaluation of vaginal bleeding Evaluation of ectopic pregnancy Confirmation of multiple pregnancy Evaluation of pelvic, ovarian or uterine pathology GUIDELINES FOR DATING PREGNANCY STAGE OF GESTATIODEVELOPMENT NAL AGE (WEEKS) Gestational sac 5 weeks Gestational sac with yolk sac Gestational sac with yolk sac & embryo LEVEL OF BHCG 5.5 weeks 1,000-2,000 mIU/L 7,200 mIU/L 6 weeks 10,800 mIU/L NUCHAL TRANSLUCENCY 11 to 14 wks =/> 3 mm Screening for fetal chromosomal abnormalities screening for trisomy 21 NON-BIOMETRIC PARAMETERS Uncertain of menstrual dates Measurement disparity in late trimester Narrow down error in estimation gestational age TRANSCEREBELLAR DIAMETER (TCD) - Numerically equivalent to the number of weeks of gestation NON-BIOMETRIC PARAMETERS COLONIC GRADE • >/= 16 weeks- grade 1, anechoic lumen • at 26 weeks & more- grade 2- lumen appears more echoic • >/= 36 weeks- grade 3, lumen becomes brigther SECOND & THIRD TRIMESTER DISTAL FEMORAL EPIPHYSES (DFE) • at least 32-33 weeks PROXIMAL TIBIAL EPIPHYSES (PTE) • Seen at 35 weeks PROXIMAL HUMERAL EPIPHYSES (PHE) • • at 38 weeks or more reliable predictor of term gestation SIGNIFICANCE OF THE RATIOS Cephalic Index (CI)BPD/OFD X 100 (74-83) > 83- brachycephaly –may suggest a genetic abnormality < 74 – dolichocephaly – seen with oilgohydramnios & breech presentation FL/AC RATIO –evaluating skeletal dysplasia - < 0.16 suggestive of a lethal type HC/ AC RATIO- determines growth lag; high ratio – implies fetal malnutrition/IUGR FL/BPD RATIO- can be used as one of the screening parameters for Down’s syndrome ( short femur & normal BPD= high ratio) - Gold standard for antepartum fetal surveillance WHEN TO REQUEST? -Antepartum testing started @ 26-28 weeks if with maternal complications -@ 32-34 weeks for high risk patients - HOW FREQUENT? Repeated weekly Most authors suggest 2x/week BPS &NST for: 1. IDDM 2. GDM with previous stillborn 3. IUGR 4. Post term pregnancy 5. Preeclampsia What are the signs of fetal hypoxia? Chronic Hypoxia (compensated) 1. Oligohydramnios 2. Asymmetric (head-sparing) IUGR Acute Hypoxia (non-compensated) 1. Abnormal fetal heart rate changes Non-reactive NST (+) CST MODIFIED BPS -uses 2 parameters, NST ( acute marker of fetal compromise) & AFV (chronic marker) Nueral Control of Fetal Biophysical Activities BIOPHYSICAL PARAMETER CNS CENTER GESTATIONAL AGE Fetal tone Cortex- subcortical area 7.5-8.5 wks Fetal movement Cortex- nuclei 9 wks Fetal breathing Ventral surface of 4th ventricle 20-21 wks Fetal Heart Reactivity Medulla & Posterior Hypothalamus 24-26 wks Note: In pregnancy complicated by IUGR, DOPPLER VELOCIMETRY studies will enhance the perfomance of BPS – changes in Doppler findings occur 4 days prior to the deterioration of BPS A sonologic procedure to assess maternal and fetal vascular resistance (vasoconstricted/vasodilated) the state of fetal perfusion. To whom should we request it for? 1. Diabetes 2. Maternal HPN 3. Autoimmune Diseases - SLE, APAS, Collagen vascular disease 4. Anemia 5. Post term Pregnancy 6. Unexplained Recurrent Pregnancy losses 7. Discordant multifetal pregnancy 8. IUGR UTERINE ARTERY WHAT ARE THE ABNORMAL RESULTS? Presence of notching Increase indices (SD, RI, PI) AND IT’S SIGNIFICANCE? Increase in the utero-placental resistance (vasoconstriction) Higher chance of pregnancy complications UMBILICAL ARTERY vasoconstriction increase intraplacental resistance elevated indices decreased fetal perfusion fetal hypoxia then IUGR ABSENT END DIASTOLIC FLOW (AEDF) highest risk to develop adverse perinatal outcome the mean duration from AEDF to onset of fetal distress is 6-8 days REVERSED END DIASTOLIC FLOW (REDF) most extreme form of intraplacental vascular resistance diagnosis to distress interval 4.2 +/- 1.4 days with perinatal moratality rate of 50% MIDDLE CEREBRAL ARTERY What is an abnormal result? DECREASED INDICES- brain sparing reflex Remember: fetal hypoxia induces compensatory reflex preferential blood flow to the brain (MCA dilatation=decreased indices) while vasoconstriction in the less vital organs NOTE: A sudden restoration of MCA indices to normal or higher or increasing indices from a serial decreasing pattern is omninous= failure of the fetal cerebral vessels to vasodilate = acute fetal brain injury Patients who are at high risk to develop abnormally adherent placenta includes: Multiparity Hx of previous CS Hx of previous curettage Placenta previa implanted anteriorly in the LUS 1. Unusually intense blood flow within the sonolucent space beneath the placenta 2. Hypervascularization within the placenta and non placental tissues 3. Turbulence of flow in areas where placentas appears to have lost parenchyma and within placenta lacunae Should be done routinely in a 20-24 weeks gestation Lowers perinatal mortality Lethal malformations-corrected early or appropriate timing of delivery to allow surgical intervention; if not amenable to surgery, early counseling ADVANTAGES OF TVS OVER TAS 1. Patient discomfort 2. Clearer images 3. Eliciting pain and tenderness 4. Earlier diagnosis of pelvic pathology 5. Good for obese patients and with abdominal scars DISADVANTAGES OF TVS OVER TAS 1. 2. 3. Discomfort & pain to pxs with intact hymen and postmenopausal Large pelvic masses Refusal of the procedure MENSTRUAL ENDOMETRIUM CYCLE OVARY Menstrual phase Early proliferative Thin echogenic line Developing follicles (5-10) Isoechoic Leading follicles Late proliferative Secretory phase Trilaminar Thick & Hyperechoic Dominant follicles (18-24) Corpus luteum Evaluates tubal patency primary investigative tool for infertility When it is performed? First part of the menstrual cycle (Day 10-12) advantage of eliminating the risk of X-ray exposure & hypersensitivity to radiographic contrast media Evaluation of endometrial pathology Evaluation of ovaries for follicular growth Evaluation of pelvic organs & structures for lessions and masses