Microbiology Revision
Dr Anna Goyder and Dr Helen McKenna
19/03/13 - 21/03/13
Outline
2 lectures x 90mins each:
•
•
•
•
Bacteria and Abx
Viruses and Antivirals
Vaccinations
Infections by system:
- CNS
- Cardio
- Resp
- GI/hepatitis
- GU/gynae
- Musculoskeletal
• Mycobacterial
• Zoonoses
• Protozoa
Recap
Bacteria simplified
• Gram positive
- Cocci
staphylococcus streptococcus enterococcus
- Rods/bacilli
ABCDL (see next slide)
• Gram negative
- Cocci
the diplococci - neisseria (gonorrhoea, meningitidis
‘meningococcus’), moraxella
- Rods/bacilli
ENTERICS - E Coli, salmonella, shigella, klebsiella, proteus,
campylobacter, helicobacter, vibrio… ie most other things!
- Coccobacilli haemophilus, legionella, brucellosis, bordetella,
chlamydia* rickettsia*
*obligate intracellular
- Spiral spirochetes – treponema (syphilis), leptospira (Weil’s), borrelia (lyme)
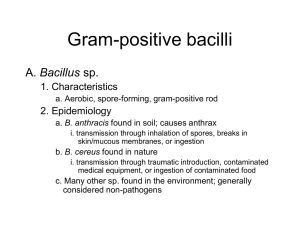
Gram + rods:
ABCD L
Actinomyces
Bacillus
(anthracis, cereus)
Clostridium (difficile, botulinum, perfringens)
Diphtheria
(corynebacterium diphtheriae)
Listeria
Respiratory Tract Infections
Upper RTI
Clinical Features
Organisms
Treatment
Coryza
Nasal symptoms
Mild pyrexia
Rhinovirus
Sinusitis
Frontal headache, nasal discharge
RF: asthma/aspirin intolerant
Pneumococcus
Haemophilus
Co-amoxiclav
Decongestant
(xylometazoline)
Fluticasone nasal spray
Pharyngitis
Soft palate, tonsils, LNs
2/3 viral (adenovirus)
1/3 bacterial (strep)
Penicillin V
Acute
laryngotracheobronchitis
(CROUP)
Child 6m-6y
Hoarse, seal-bark cough, stridor, recession,
cyanosis
Viral (parainfluenza, influenza,
measles, RSV)
Steroids/inhaled adrenaline
Acute epiglottitis
High fever, stridor, drooling
Haemophilus influenza B
(Vaccinatiions at 2,3,4m)
DO NOT INSPECT EPIGLOTTIS
Call Senior Anaesthetist
IV 3rd gen ceph +/- penicillin
(rifampicin for unvaccinated
contacts)
Influenza
Fever, headache, arthralgia, sore throat,
persistent dry cough
A (pAndemics)
B outBreaks
Secondary bacterial infection
(pneumococcus, haemophilus)
Bed rest, paracetamol
Neuraminidase inhibitors
(oseltamivir)
Vaccinate:
>65, DM, immunocompromise,
chronic bronchitis, heart or renal
failure
Scarlet Fever
Fever, rigors, blanching rash (neck
generalised punctate, sparing face, palms),
desquamation, circumoral pallor, strawberry
tongue
Complications:
rheumatic fever; glomerulonephritis.
Group A
Beta-haemolytic strep
Strep pyogehes
(throat swab, ASOT, anti-DNAse
B)
Penicillin
Diphtheria
Nasal discharge, tough grey membrane in
pharynx, bullneck LN
Day 5: myocarditis, CN palsy
Corynebacter
Antitoxin
Penicillin V
Lower Respiratory Tract
Infections
1. Acute bronchitis:
Medium airways
Irritating cough/sputum
Tightness, wheeze
Mild fever
Scattered crackles
Normal CXR
CAUSES:
Viral
with secondary bacterial infection in
smokers/COPD (pneumococcus, Hib,
Moraxella)
Treatment:
Bronchodilators, respiratory physiotherapy
to mobilise secretions.
2. Pneumonia
Alveoli
Productive cough
SICKER: fever, pleuritic pain
Localised signs of consolidation (dull to
percussion, crackles, bronchial breathing)
CXR: lobar, bronchopneumonia
Community Acquired Pneumonia
Organism
Treatment
Typicals
Pneumococcus: rusty sputum, lobar consolidation, vaccine
Haemophilus/Moraxella: smokers
MILD: amoxicillin
MOD: co-amoxiclav
Klebsiella: ETOH, rapid onset, destructive -> redcurrant jelly sputum
Atypicals
Mycoplasma:
outbreaks in institutions, dry cough, normal examination, normal WCC, CXR worse
(bibasal infiltrates)
cold agglutinins, erythema multiforme (target lesions) CNS, Stevens-Johnson,
AIHA
Send Serology
Legionella:
water systems, low Na, deranged LFTs
(Ag in urine; Ab serology)
Chlamydia
Poor response to antibiotics – consider:
Pertussis (“100 days cough”)
TB (ethnicity, weight loss, haemoptysis, upper lobe cavitation)
VIRAL:
Pregnancy, immunocompromise
usually Influenza A – also CMV/EBV/VZV (test for with NPA)
Intracellular organisms
cannot be treated with
antibiotics that target cell
wall
CLARITHROMYCIN
Which organism is responsible?
65 year old man presents to A&E
Productive cough and pleuritic chest pain
Rusty sputum: Gram positive cocci
30 year old pregnant woman presents to GP
Recent flu-like symptoms for last week
Now has productive cough and fever
Hospital Acquired Pneumonia
Inpatient > 48 h:
1.Staph aureus (including MRSA)
2.Aerobic Gram negative rods (Coliforms, Enterobacter,
Pseudomonas)
3. Aspiration: Anaerobes (most likely RLL)
4. Fungi
Now need to cover gram negative rods, including pseudomonas
(and, if suspect aspiration – anaerobes)
1. Ciprofloxacin (or tazocin)
2. MRSA -> ADD vancomycin
3. VRSA -> ADD linezolid
Pseudomonas
Naturally resistant to a large range of antibiotics
Develops resistance after unsuccessful treatment (porin modification)
Anti-pseudomonals include:
Aminoglycosides (gentamicin/amikacin)
Quinolones (ciprofloxacin)
Cephalosporins (ceftazidime – not ceftriaxone)
Certain Penicillins (piperacillin)
Carbapenems (Meropenem)
Polymixin B and colistin
All must be given intravenously – apart from ciprofloxacin
Questions
40 year old woman admitted with pneumonia following
holiday in Turkey.
Bloods show hyponatraemia and deranged liver function.
Which investigation is most likely to confirm the
diagnosis?
A Sputum culture
B Urinary Ag
C Blood culture
D Bone marrow aspirate
E LP
28 year old man admitted with SOB and fever.
2/7 itchy vesicular rash after contact with
brother with chicken pox.
T 39, HR120, BP 135/68, Sats 95% OA
Chest: occasional fine crackles
Which is the most important intervention?
A Elective intubation within next 24h
B Prednisolone
C VZIg
D IV aciclovir
E Paracetamol
17 year old presents with 4/7 sore throat,
headache and lethargy.
Doctor prescribed course of amoxicillin for
URTI.
2/7 later her symptoms persist and she
develops a maculopapular rash.
A Kawasaki Disease
B Penicillin allergy
C HIV seroconversion
D Beta-lactamase producing streptococcal
infection
E Infectious mononucleosis
Gastro/Hepatology
1. Diarrhoea and vomiting
2. Hepatitis
Bacteria simplified
• Gram positive
- Cocci
staphylococcus streptococcus enterococcus
- Rods/bacilli
ABCDL – Bacillus, Clostridium, Listeria
• Gram negative
- Cocci
the diplococci - neisseria (gonorrhoea, meningitidis
‘meningococcus’), moraxella
- Rods/bacilli
ENTERICS - E Coli, salmonella, shigella, klebsiella, proteus,
campylobacter, helicobacter, vibrio… ie most other things!
- Coccobacilli haemophilus, legionella, brucellosis, bordetella,
chlamydia* rickettsia*
*obligate intracellular
- Spiral spirochetes – treponema (syphilis), leptospira (Weil’s), borrelia (lyme)
Gastro – D&V
Incubation period
• 1-6
hrs: Staphylococcus aureus, Bacillus
cereus*
• 12-48 hrs: Salmonella, Escherichia
coli
Bacterial gastroenteritis
What
Source
Presentation
Buzzwords
Bacillus
Cereus
Gram +
rod
Rice
Vomiting <6hrs/diarrhoea >6hrs after
rice
REHEATED
RICE
Staph
Aureus
Gram +
cocci
Unrefrigerate
d meat/dairy
Food poisoning –vomiting ++, short
incubation time, self-limiting
Salmonella
Gram rod
Meat, eggs
Non-bloody diarrhoea
Gastro - Salmonella
Gram negative rods
Not normally present as commensals in the human GI
tract.
S. Enteritidis infection occurs following contamination with
animal faeces
Sp
Disease
Presentation
Treatment
S.
Enterocolitis
Enteritidis
Non-bloody diarrhoea. Fever in
half of patients. Lasts <1/52
None/
ciprofloxacin
S. Typhi
Typhoid
S.
Paratyphi
Paratyphoid
Systemic symptoms –
headache, fever, arthralgia,
bradycardia,
abdo pain,
constipation,
rose spots (more common in
paratyphoid)
Can lead to chronic carriage
Ceftriaxone/
ciprofloxacin
C. Inhibitors of DNA synthesis
Recap:
• Quinolones –
Ciprofloxacin, Moxifloxacin, Levofloxacin
(think Ciprofloxaquin, Moxifloxaquin etc)
Act on DNA Gyrase
Active mostly against Gram negatives –
use for UTIs, bacterial gastroenteritis
Bacterial gastroenteritis
What
Source
Presentation
Buzzwords
Bacillus
Cereus
Gram +
rod
Rice
Vomiting <6hrs/diarrhoea >6hrs after
rice
REHEATED
RICE
Staph
Aureus
Gram +
cocci
Unrefrigerate
d meat/dairy
Food poisoning –vomiting ++, short
incubation time, self-limiting
Salmonella
Gram rod
Meat, eggs
Non-bloody diarrhoea
E. Coli
Gram rod
Human
faeces
Watery diarrhoea, abdo pain, nausea
TRAVELLERS
’ DIARRHOEA
Gastro – E. Coli
Most strains are harmless, flora
Classified by virulence factors and diseases caused:
•ETEC – enteroToxigenic, Traveller’s diarrhoea - produces
two exotoxins, similar to cholera – heat labile toxin (LT) and heat stable
toxin (ST) – watery osmotic diarrhoea, non-invasive, no fever
•EPEC – enteroPathogenic, moderately invasive. Similar to
shigella – Shiga toxin/verotoxin
•EIEC – enteroInvasive – dysentery – causes host response clinically identical to Shigella
•EHEC – enteroHaemorrhagic – e.g. infamous O157:H7 strain –
shiga toxin, inflammatory response, can cause Haemolytic Uraemic
Syndrome
Bacterial gastroenteritis
What
Source
Presentation
Buzzwords
Bacillus
Cereus
Gram +
rod
Rice
Vomiting <6hrs/diarrhoea >6hrs after
rice
REHEATED
RICE
Staph
Aureus
Gram +
cocci
Unrefrigerate
d meat/dairy
Food poisoning –vomiting ++, short
incubation time, self-limiting
Salmonella
Gram rod
Meat, eggs
Non-bloody diarrhoea
E. Coli
Gram rod
Faecal oral
Watery diarrhoea, abdo pain, nausea
Shigella
Gram rod
Faecal oral
Bloody diarrhoea, abdo pain,
vomiting - Dysentery
Campylobacter
Gram rod
Animal
faeces
Flu-like prodrome, crampy abdo
pain, bloody diarrhoea, post-inf GBS
Cholera
Gram rod
Contaminate
d food/water
Watery diarrhoea ++
Dehydration, weight loss
TRAVELLERS
’ DIARRHOEA
RICE WATER
STOOL
C. difficile - SBA
A 88-year-old patient develops profuse, offensive watery
diarrhoea following a course of co-amoxiclav.
Clostridium difficile diarrhoea is diagnosed. On
examination, her observations are stable, she is apyrexial
and has no abdominal signs. What is the most
appropriate first-line therapy?
A.Oral vancomycin
B.Oral metronidazole
C.Oral metronidazole + vancomycin
D.Faecal transplant
E.Probiotic yoghurt
Gastro – Clostridium difficile
• Gram positive rod
Recap:
Gram positive rods:
ABCD L
Actinomyces
Bacillus
(anthracis, cereus)
Clostridium (difficile, botulinum, perfringens)
Diphtheria
(corynebacterium diphtheriae)
Listeria
Gastro – Clostridium difficile
• Gram positive rod
• Exotoxin produced-> damages gut ->
pseudomembranous colitis.
Features
• Diarrhoea, abdominal pain
• a raised white blood cell count is characteristic
• if severe toxic megacolon may develop
• Hospital acquired infection (HAI) EPIDEMIC
• Associated with loss of normal gut flora – commonly
after broad-spectrum antibiotics.
Gastro – Clostridium difficile
Diagnosis
• Clostridium difficile toxin (CDT) in the stool
Management
• first-line therapy is oral metronidazole for 10-14 days
• if severe or not responding to metronidazole then oral
vancomycin may be used
• for life-threatening infections a combination of oral
vancomycin and intravenous metronidazole should be
used
Anaerobes
Recap:
• OBLIGATE
• FACULATIVE
CANNOT use O2/grow
where there is oxygen
Can grow where there is OR
isn’t oxygen
Bacteroides
Clostridium
Actinomyces
Staphylococcus, E. Coli,
Listeria
C. Inhibitors of DNA synthesis
Recap:
• Quinolones –
Ciprofloxacin, Moxifloxacin, Levofloxacin (think
Ciprofloxaquin, Moxifloxaquin etc)
Act on DNA Gyrase
Active mostly against Gram negatives –
use for UTIs, bacterial gastroenteritis
• Nitroimidazoles –
Metronidazole
Useful against anaerobes and protozoa
• Nitrofurantoin - UTIs
A. Cell wall synthesis inhibitors
β-lactams
Recap:
1. Penicillins
Crossreactivity – caution if hx
anaphylaxis
2. Cephalosporins
1st generation – gram + > 2nd generation – gram + and 3rd generation – gram - > +
- have T in them – T for ‘third’
cefotaxime, ceftazidime, ceftriaxone
3. Carbapenems
B R O A D spectrum
Glycopeptides
Require therapeutic drug monitoring
(TDM)
1. Vancomycin
Usually IV – covers MOST GRAM +
incl MRSA - but NOT VRE!
Exception - oral vancomycin – for
C. Difficile diarrhoea (where
metronidazole has failed)
Vancomycin
2. Teicoplanin – negligible
systemic absorption –
used ORALLY for C. Diff
Gastro – Clostridium difficile
Relative risk (RR) of developing
Clostridium difficile following antibiotic therapy:
Clindamycin: RR = 31.8
Cephalosporins: RR = 14.9
Ciprofloxacin: RR = 5.0
Second and third generation cephalosporins more
assoc with C. Difficile than first generation
www.passmedicine.com
Protozoa in Gastroenteritis
Species
Features
Clinical features
Treatment
Amoebiasis
Entamoeba
histolytica
4 nuclei
Dysentery – bloody
diarrhoea
Chronic infection –
weight loss
Liver abscess
Metronidazole
Giardiasis
Giardia
Lamblia
2 nuclei
Prolonged, foulsmelling non-bloody
diarrhoea, flatulence,
malabsorption
Travellers/institutions
Metronidazole
Severe diarrhoea in
the
immunocompromised
Paromomycin
Cryptosporid Cryptosporid
osis
ium Parvum
C. Inhibitors of DNA synthesis
Recap:
• Quinolones –
Ciprofloxacin, Moxifloxacin, Levofloxacin (think
Ciprofloxaquin, Moxifloxaquin etc)
Act on DNA Gyrase
Active mostly against Gram negatives –
use for UTIs, bacterial gastroenteritis
• Nitroimidazoles –
Metronidazole
Useful against anaerobes and protozoa
• Nitrofurantoin - UTIs
Protozoa in Gastroenteritis
Species
Features
Clinical features
Treatment
Amoebiasis
Entamoeba
histolytica
4 nuclei
Dysentery – bloody
diarrhoea
Chronic infection –
weight loss
Liver abscess
Metronidazole
Giardiasis
Giardia
Lamblia
2 nuclei
Prolonged, foulsmelling non-bloody
diarrhoea, flatulence,
malabsorption
Travellers/institutions
Metronidazole
Cryptosporidosis
Cryptosporid
ium Parvum
Severe diarrhoea in
the
immunocompromised
Paromomycin
GI EMQ 1
A)
B)
C)
D)
E)
F)
G)
H)
I)
J)
K)
L)
M)
N)
O)
Salmonella enteritidis
Salmonella typhi
Shigella
ETEC
EHEC
EIEC
Vibrio cholerae
Giardia Lamblia
Entamoeba Histolytica
Campylobacter Jejuni
Bacillus Cereus
Clostridium difficile
Clostridium perfringens
Rotavirus
Norovirus
A 24-year old medical student
preparing for his finals reports
a 4 week history of abdominal
pain, foul-smelling greasy
diarrhoea and increased
flatulence.
Please choose one answer
from the adjacent list
GI EMQ 2
A)
B)
C)
D)
E)
F)
G)
H)
I)
J)
K)
L)
M)
N)
O)
Salmonella enteritidis
Salmonella typhi
Shigella
ETEC
EHEC
EIEC
Vibrio cholerae
Giardia Lamblia
Entamoeba Histolytica
Campylobacter Jejuni
Bacillus Cereus
Clostridium difficile
Clostridium perfringens
Rotavirus
Norovirus
An 18-year old Imperial student
comes to the GP with a 4 hour
history of vomiting, which
began at lunchtime. He
wonders if it might be related to
the leftovers he had for
breakfast that morning
following his Chinese New
Year celebrations last night.
Please choose one answer
from the adjacent list
GI EMQ 3
A)
B)
C)
D)
E)
F)
G)
H)
I)
J)
K)
L)
M)
N)
O)
Salmonella enteritidis
Salmonella typhi
Shigella
ETEC
EHEC
EIEC
Vibrio cholerae
Giardia Lamblia
Entamoeba Histolytica
Campylobacter Jejuni
Bacillus Cereus
Clostridium difficile
Clostridium perfringens
Rotavirus
Norovirus
A 40-year-old female patient
reports loose stools for a week
ever since returning from
Morocco last week. She
otherwise feels well.
Please choose one answer
from the adjacent list
GI EMQ 4
A)
B)
C)
D)
E)
F)
G)
H)
I)
J)
K)
L)
M)
N)
O)
Salmonella enteritidis
Salmonella typhi
Shigella
ETEC
EHEC
EIEC
Vibrio cholerae
Giardia Lamblia
Entamoeba Histolytica
Campylobacter Jejuni
Bacillus Cereus
Clostridium difficile
Clostridium perfringens
Rotavirus
Norovirus
A 25-year-old patient comes to
see the clinic you are running
whilst on your elective.
She reports a lengthy history of
bloody diarrhoea and weight
loss. On examination, her
abdomen is soft but tender,
particularly in the right upper
quadrant.
Please choose one answer
from the adjacent list
Gastro/Hepatology
1. Diarrhoea and vomiting
2. Hepatitis
Viral hepatitis
SBA:
Which one of the following statements best describes the
prevention and treatment of hepatitis C?
A.No vaccine is available and treatment is only
successful in around 10-15% of patients
B.No vaccine and no treatment is available
C. A vaccine is available and treatment is successful in
around 50% of patients
D. A vaccine is available but no treatment has been
shown to be effective
E.No vaccine is available but treatment is successful in
around 50% of patients
Hepatitis B vs C
Hep B
Hep C
Structure
dsDNA
RNA
Genotypes 2,3 GOOD, 1,4 BAD
Vaccines
YES
NO
Transmission
Bloodborne, vertical, sexual
Bloodborne, esp transfusions
in emqs
Complications •chronic infection (5-10%)
•Fulminant liver failure (1%)
•Fibrosis, cirrhosis
•HCC
•Glomerulonephritis
•Polyarteritis nodosa
•Cryoglobulinaemia
•chronic infection (80-85%)
•cirrhosis (20-30% those with
chronic disease)
•HCC
•Cryoglobulinaemia
Treatment
Pegylated IFN-alpha + ribavirin
- Up to 55% clear the virus with
treatment (up to 80% for some
strains)
Oral antivirals e.g. lamivudine,
tenofovir and entecavir
Hep B
You wish to screen a patient for hepatitis B
infection. Which one of the following is the most
suitable test to perform?
A. HBcAg
B. HBsAg
C. Hepatitis B viral load
D. anti-HBs
E. HBeAg
Hepatitis B serology
Vaccination
Anti-HBs (Ab)
HBsAg
Anti-HBc
IgM
Anti-HBc
IgG
HBeAg
Anti-HBe
Incubation Acute
Chronic Recovery
/carrier
+
+
+
+
+
Hepatitis B serology
Vaccination
Anti-HBs (Ab)
HBsAg
Incubation Acute
+
+
+
+
Anti-HBc
IgM
+
Anti-HBc
IgG
+
HBeAg
Anti-HBe
Chronic Recovery
/carrier
+
+
+
Hepatitis B serology
Vaccination
Anti-HBs (Ab)
HBsAg
Incubation Acute
Chronic Recovery
/carrier
+
+
+
+
+
Anti-HBc
IgM
+
Anti-HBc
IgG
+
+
+
+/-
HBeAg
Anti-HBe
+
+/-
+
+/-
Hepatitis A, D, E
• Hepatitis A, E – faecal-oral transmission
• Hepatitis D – co-infects patients already
infected with Hepatitis B
Urinary Tract
Symptoms
Lower Urinary Tract
Upper Urinary Tract
Dysuria, suprapubic pain
Frequency (nocturia)
Haematuria
Offensive Urine
Loin pain
Unwell, Fever (rigors)
+/- LUTS
Children < 2y
Elderly
FTT
Vomiting
Fever
Incontinence
Hesitancy
Abdominal pain
Change in mental status
2 symptoms of UTI
3 symptoms of UTI
+
NO vaginal
discharge/irritation
NITRITES
Leucocytes
Blood or
Protein
Negative
90% culture positive
Treat
empirically
Review time
of sample
Send culture
Treat if
severe
Consider
other
diagnosis
Reassure
Treat empirically
DIPSTICK
MICROSCOPY
Indications for Urine Culture:
White cells
Squamous cells
Pyuria
contamination
If Sterile =
treated UTI,
calculus, catheter,
bladder tumour,
TB, STI
Pregnant (1st visit, symptomatic)
Any sick or febrile child
Men
Pyelonephritis > 39, rigors, NVD, loin pain
Catheter and systemic symptoms
Persistent symptoms
Renal impairment
Structural abnormalities.
Culture indicates infection if > 10 ^ 5 CFU of single organism
Uncomplicated
Complicated
E. Coli
Increased likelihood of:
Proteus
Pseudomonas
Klebsiella
Enterobacter
Staph saprophyticus
Enterococcus
3 days Cephalexin
7 days Nitrofurantoin (NOT IF CrCl <60)
Pregnant:
7 days cephalexin or co-amoxiclav
Male:
7 days cephalexin
Prostatitis: ciprofloxacin for 14 days
4-6 weeks if chronic
Pyelonephritis or urosepsis
IV co-amoxiclav +/- aminoglycoside (amikacin or
gentamicin)
Pen-allergic: ciprofloxacin
IMAGING to look for calculi/structural abnormality
Catheter:
Stat gentamicin prior to removing catheter (only
treat post- removal if systemically unwell)
Sexually Transmitted Infections
Most common
organisms
1.
2.
3.
4.
5.
Chlamydia
Genital warts
Herpes
Gonorrhoea
Syphilis
DISCHARGE
ULCERATION
RASH/LUMP
CHLAMYDIA
GONORRHOEA
HERPES (HSV)
SYPHILIS
GENITAL WARTS
Trichomonas
Candida
BV
LGV (chlamydia)
Chancroid
Donovanosis
Molluscum
Scabies
Pubic Lice
Chlamydia
Organism
Features
Complications
Test
Treatment
Obligate intracellular parasites
2 forms:
None
A, B, C: Trachoma
D- K : Genital infection, ophthamlia neonatorum
Gold standard:
Nucleic Acis
Amplification Tests
(urine, vulvovaginal
swab)
Tetracyclins
for 7d
(or one-off
azithromycin)
Extracellular infectious
elementary bodies
Intracellular metabolically active
reticulate particules
Discharge
Dysuria
PID (59%)
Tubal factor infertility (70%)
Ectopic pregnancy (x9.5)
Endometrioisis
Reiter’s
“Non-specifif
urethritis”
Partner
identification
(“treat than
test”)
L 1,2,3 (Tropics): lymphogranuloma venerum:
Primary – painless ulcer
Secondary – painful inguinal buboes and
constitutional symptoms
Encephalitis, pneumonia, hepatitis, proctocolitis
(strictures, abscesses, fistulae, lymphorrhoids)
Gonorrhoe
a
Intracellular
Gram negative diplococcus
Men:
Urethra
(rectum)
Complicate
d: prostatitis
Women:
Urethra
(cervis)
Complicate
d:
salpingitis
Trichomoni
asis
Flagellate protazoan
Irritating,
frothy
discharge
Candida
Yeast
Usually albicans
Not an STI – normal flora
RF: immunocompromise; poor
Discharge,
itchiness,
erythema,
pain
Disseminated gonococcal infection:
-associated with AHU-requiring strains
-RF: deficiencies in late complement components
Septicaemia
Rash
Arthritis
Urethral smears:
95% sensitive in
symptomatic women
35% sensitive in
asymptomatic cases
or men
Rectal smear
>20% sensitive
3rd gen
cephalospori
n
(increased
ciprofloxacin
resistance)
Gold standard:
Culture (also
demonstrates
sensitivities)
NAATs
Wet prep microscopy
PCR
(culture rarely done)
Topical:
clotrimaxole
Oral:
Organism
Features
Complications
Test
Treatment
Herpes
DNA virus
HSV-2
(HSV-1 in 1/6)
Asymptomatic
Clusters of inflamed
papules and vesicles
(cold sores)
PAIN, burning, itching
Recurrence
Cutaneous
dissemination
Visceral involvment:
Oesophagitis, colitis,
hepatitis, myelitis
Swab PCR
Biopsy
Blood
To shorten course:
Aciclovir
valaciclovir
Syphilis
Treponema pallidum
Obligate HUMAN
pathogen
1: macule – indurated
painless ulcer
(CHANCRE)
Regional adenopathy
2: 6 weeks later:
Systemic bacteraemia
Symmetrical
maculopapular rash
Uveitis
Neurolocgical: CN
palsies, optic neuritis,
aseptic meningitis
3. 2-40 years later:
Skin, bone
Aortitis
Neurosyphilis: tabes
dorsalis, general
paresis of the insane
Dark ground
microscopy
Multiplex real-time PCR
Penicillin G
Azithromycin
Chancroid
Haemophilus ducreyi
Multiple PAINful ulcers
Gold standard:
Serum antibody (TST)
ELISA
VDRL slide (detect
lipoidal antibody)
Increased risk of HIV
Culture
PCR
Gram negative
coccobacillus
(Africa/Tropics)
Donovaniasis
Klebsiella granulomatis
Gram negative bacillus
(Africa/India/Australia)
Beefy red ulcer
Painless
Granuloma inguinale
Biopsy:
Giemsa stain
Donovan bodies
Azithromycin
Organism
Features
Complications
Genital warts
Human papilloma
virus
Ds DNA virus
No envelope
98% HPV 6 and 11
Papular, planar,
pedunculated
Keratinised
pigmented
Oncogenic types =
16 and 18
associated with
cancer of:
Cervix, Vulva
Anus
Penis
Head and neck
Molluscum
contagiosum
Ds DNA pox virus
GIANT
Facial in adult –
consider HIV
Scabies
Mite
Sarcoptes scabiei
Itching
crescendoes over
2-3w.
Noctural pruritis
Test
Treatment
Podophylotoxon/I
miquimod
Permethrin
Questions
20 year old man presents with dysuria and watery
discharge from urethra.
Urethral swab: non-specific urethritis.
Which is the most appropriate antibiotic?
A Erythromycin
B Ciprofloxacin
C Metronidazole
D Cefixime
E Azithromycin
35 homosexual man developed solitary
painless penile ulcer associated with painful
inguinal lymphadenopathy. He also has
rectal pain and tenesmus.
A Herpes simplex
B Syphilis
C Granuloma inguinale
D Chancroid
E Lymphogranuloma venereum
38 year old man presents with multiple
painless genital ulcers. What is the most
likely causative organism?
A Klebsiella granulomatis
B Chlamydia
C Herpes simplex
D Treponema pallidum
E Haemophilus ducreyi
30 year old woman presents with white,
malodorous vaginal discharge. No itch or
dyspareunia.
What is the most likely organism?
A Lactobacilli
B Trichomonas
C Candida
D Mycoplasma hominis
E Gardnerella
Bone and Joint
Risk Factors
Route
• Septic
ArthritisBlood/
Any abnormal
JOINT:
joint/
direct
Septic
predisposition to
Arthritis
infection
Clinical
features
Organisms
Ix
Pyrexial
Hot swollen
joint
S. Aureus 46%
Strep 22%
CoNS 4%
Gram - rods
Joint aspiration
and blood
cultures BEFORE Abx!
Inflammatory
markers
Imaging
• Osteomyelitis
Salmonella
in patients
with
Cell Aspirate,
Surgical factors:
Blood/
Pain,
failureSickle
Gram + cocci
JOINT:
Prosthetic
Joint
infection
prosthesis with
long operation/
wound healing
complications
Patient factors:
as above
direct
of joint,
sinus
formation
Gram - rods
Inflammatory
markers
Imaging
BONE:
Osteomyelitis
As above
Sickle cell
Blood/
direct
Pain, fever,
local
swelling
S. Aureus most
common
Salmonella in
patients with
Sickle Cell
MRI
Biopsy
Mycobacterial disease
• Mycobacterium tuberculosis
• Mycobacterium leprae
Mycobacterium tuberculosis
• 30% of close contacts of pulmonary TB patients will be
infected
• Of these
– 5% will develop tuberculosis in next 1-2 years
– 5% will develop tuberculosis in later life
• Primary infection – from aerosolised droplets
– Localised pneumonitis
– Bacteria enter macrophages and spread via lymphatics and
blood, leading to either:
• Asymptomatic primary infection
• Symptomatic disease – in children, elderly, immunocompromised
• Secondary/reactivation tuberculosis- 10% lifetime risk for
healthy people, 10% annual risk in HIV!
Zoonoses
Zoonoses
Presentation
• Leptospirosis
Leptospirosis 2 phases separated by ~1 week
1.
fever, muscle aches, malaise,
• Lyme disease
+ Weil’s
disease
Lyme disease
– borrelia
burgdorferi
photophobia, RED
CONJUNCTIVA
2.
Symptoms return with
meningitic signs ++
WEIL’S disease – severe form, with
renal failure and hepatitis
with jaundice
3 phases
1.
Early localised – ECM for
4/52 with flu-like Sx
2.
Early disseminated – multiple
smaller ECM, neuro, cardiac,
arthritis
3.
Late stage – Chronic arthritis,
encephalopathy
Source
Mx
Drinking/
swimming in water
contaminated with
urine of rats, dogs
Penicillin/
Doxycycline
Ixodes tick
Animal reservoir =
small rodents and
the white-tailed
deer
Penicillin/
Doxycycline
Lyme disease
Protozoa
• Malaria
• Leishmania
• Trypanosoma
Malaria
Clinical
P. falciparum
Fevers
Liver phase?
Chloroquine
resistance?
Severe,
multiorgan
Continuous
/48hrly
no
Y
P. vivax
Mild
48hrly
Y–
primaquine
needed
No
P. ovale
Mild
48hrly
Y–
primaquine
needed
No
P. malariae
Mild
72hrly
No
No
Source
Geography
Leishmaniasis
Sandfly
South/central
america,
africa, middle
east
Trypanosomiasis
– African
‘African Sleeping
sickness’
Tsetse fly
West Africa –
1.
T. gambiense,
East Africa – T. 2.
rhodiense
(rhodiense
3.
more severe
form)
Trypanosomiasis
– American
‘Chagas disease’
Reduviid
bug
‘Kissing
bug’
Southern US,
central, south
America
T. cruzi
(Think Tom
Cruise)
`
Presentation
Mx
Simple Cutaneous
“oriental sore” = ulcer
Diffuse cutaneous =
multiple nodules
Mucocutaneous =
ulcers in mouth
Visceral = Kala Azar –
hepatosplenomegaly
Stibogluconate
1.
Initial painful red
ulcer
Systemic spread,
intermittent fevers
CNS symptoms –
drowsiness –
coma – death
Acute disease ‘Chagoma’ – hard
red area +/Systemic spread
2.
Intermediate
asymptomatic
phase
3. Chronic phase – GI,
Cardiac
Nifurtimox,
eflornithine
Nifurtimox,
benznidazole
Thanks for coming
• Good luck
• PLEASE FILL IN A TEACHING
FEEDBACK FORM!