Clinical-Trials-talk-for-Regional-Conf-FINAL-VERSION
advertisement
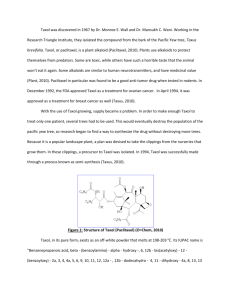
Clinical Trials in Ovarian Cancer Ovarian Cancer Coalition Regional Conference November 5, 2010 Overview • • • • • Preclinical drug development Regulations to protect participants Goals of clinical trials Landmark clinical trials in ovarian cancer Evolution of a phase I trial of immune therapy at Penn • Where to get more information Clinical trials vs. standard health care • Clinical care: interventions designed solely to enhance the well-being of the patient that have a reasonable expectation of success • Research: an activity designed to test a hypothesis, permit conclusions to be drawn, develop or contribute to generalizable knowledge Drug Development • Serendipity • Broad search and screen • Design based on natural substances • Molecular knowledge of a receptor Pre-clinical drug development • Maximum tolerated dose • Route of administration • Bioavailability and metabolism studies • Characterization of toxicity – – – – Acute toxicity Subacute toxicity Chronic toxicity Teratogenicity and carcinogenicity History of Clinical Trials • 1747 James Lind, Naval physician, tests therapies for scurvy Declaration of Helsinki • Developed by the World Medical Association as a set of ethical principles for human experimentation • Established Institutional Review Boards (IRB) • Emphasizes informed consent • Defined vulnerable populations • Regulates the inclusion and selection of placebo groups Regulatory Agencies in the US • Food and Drug Administration – – – • Research 21 CFR 50.3(c) defines research as an experiment that involves a test article and one or more human subjects that is subject to the IND or IDE regulations or which collects data to be submitted to or held for inspection by FDA. Research is subject to the IND regulations when it involves any use of a drug except for the use of a marketed drug in the course of medical practice (21 CFR §312.3) Human Subject 21 CFR 50.3(e) defines human subject as an individual who is or becomes a participant in research, either as a recipient of a test article or as a control. In the case of research involving a medical device, a human subject also includes an individual on whose specimen a medical device is used. Test Article 21 CFR 50.3(j) defines test article as any drug (including a biological product for human use, medical device for human use, human food additive, color, adaptive, electronic product, or any other article subject to regulation under the jurisdiction of the FDA Office for Human Research Protections: The Common Rule – – – – – – Research 45 CFR 46.102(d) defines research as a systematic investigation, including research development, and testing and evaluation, designed to develop or contribute to generalizable knowledge. Human Subject 45 CFR 102(f) defines a human subject as an individual about whom an investigator conducting research obtains data through intervention or interaction with individual or identifiable private information. Intervention or Interaction includes physical procedures performed on an individual, manipulation, communication or interpersonal contact with an individual or manipulation of an individual's environment. Private information includes information that an individual can reasonably expect will not be made public, and information about behavior that an individual can reasonably expect will not be observed or recorded. Identifiable means that the identity of the individual is or may be readily ascertained by the investigator or associated with the information. www.hhs.gov/ohrs;/humansubjects/guidance HIPAA Health Insurance Portability and Accountability Act, April 2003. Protects information about the physical or mental health of an individual relating to health, health care, or payment for care in the past, present or future. Institutional Review Boards (IRB) • Protects the rights and welfare of research subjects • Oversees the conduct of all human research • Ensures compliance with all federal, state, local and institutional requirements in human subject research. • Includes members of the community Principles governing clinical trials • Regulatory codes place the responsibility for the ethical conduct of research on the shoulders of researchers – Autonomy • • • • Informed consent Confidentiality Comprehension Voluntariness – Beneficience • • • • Risks-to-Benefit Ratio Research Design (minimizing risk) Investigator Qualifications Conflicts of Interest – Justice • • • • Balance of Burdens/Benefits Population of Inference Eligibility Criteria Representative of Population Equitable Recruitment Methods Informed Consent • Purpose • Methods and procedures in detail • Risks and discomforts – Risk of disease vs risk of study participation • Benefits • Alternatives to participation • Voluntary and uncoerced Randomization • Provides the best assurance that prognostic factors, both measured and unmeasured, are similar in treatment and control groups • Provides the most credible evidence of treatment effects • Placebo control is optimal to evaluate new treatments – Only appropriate when no known effective treatment is available Blinding • Limits possible bias – Patient response – Physician attitude – Outcome evaluation – Decision-making during study • Single-blind: treating physician knows but patient doesn’t • Double-blind: neither the treating physician nor the patient knows Phases • Phase I Trials: maximally tolerated dose – Safety and tolerability – Uncontrolled, unblinded – Not randomized • Phase II Trials: evaluate for evidence of a clinical effect – Dose-finding (and continued safety) (dose dependence) – Controlled or uncontrolled; may be blinded or unblinded – Randomized or not randomized • Phase III Trials: test whether a new treatment is superior – – – – Therapeutic ratio (and continued safety) (Drug x compared to drug y) Control is placebo or standard of care. Blinded Randomized • Phase IV Trials: post-marketing surveillance (safety) Eligibility • • • • Disease type Prior therapy Performance status Evidence of adequate renal and hepatic function • Measurable disease • Prior malignancies Study Endpoints • Adverse events – standard criteria to categorize as: none, mild, moderate, severe, life-threatening • Response – Progressive disease – Stable disease – Parital response: decrease in the size of measurable disease by 50% – Complete response • Progression-free survival • Overall survival • Quality of life Early stopping rules • To avoid subjecting participants to ineffective therapy • Interim analysis: – No effect, stop the trial – Significant effect, stop the trial – Intermediate, continue accrual. LANDMARK CLINICAL TRIALS IN THE TREATMENT OF OVARIAN CANCER GOG 111 trial established platinum/taxane combination therapy as the standard of care Suboptimal Stage III and any stage IV RANDOMIZE Cisplatin (75 mg/m2 q21d x 6) PLUS Cyclophosphamide (750 mg/m2) Cisplatin (75 mg/m2 q21d x 6) PLUS Paclitaxel (135 mg/m2/24h) GOG 111: progression-free survival Patients (N) 1.0 ProgressionFree Median Survival Relative Risk 0.9 Treatment 0.8 Cisplatin/ Cyclophosphamide 15 187 202 13.3 – Cisplatin/Paclitaxel 18 166 184 18.0 0.70 54 60 0.7 Proportion Surviving 0.6 Progression 0.5 Free 0.4 Failure Total 0.3 0.2 0.1 0.0 0 6 12 18 24 30 36 42 48 Months After Study Entry McGuire, NEJM, 1996 66 72 78 84 GOG 111: overall survival 1.0 No. Pts 0.9 Proportion surviving 0.7 Relative Risk Alive Died Cisplatin/ cyclophosphamide 28 174 202 24.8 – Cisplatin/paclitaxel 35 150 184 36.9 0.69 Treatment 0.8 Median Total Survival (mos) 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 6 12 McGuire, NEJM, 1996 18 24 30 36 42 48 54 60 Months from entry into study 66 72 78 84 Substituting taxol for cytoxan improved survival GOG 111 OV-10 Treatment Cis 75 + Cytoxan 750 Cis 75 + Taxol 135 24 hr Cis 75 + Cytoxan 750 Cis 75 + Taxol 175 3hr PFS (months) 13 18* 11.5 15.5* OS (months) 24 38* 26 36* Neuropathy McGuire, NEJM, 1996 4% *p<0.001 14% Piccart, JNCI, 2000 GOG 158: Is carboplatin as effective as cisplatin? Ozols, JCO, 2003 Outcome is the same, toxicity is different Ozols, JCO, 2003 Carboplatin and Taxol currently are standard chemotherapy for ovarian cancer. GOG 111 GOG 158 Treatment Cis + Cytoxan Cis + Taxol Cis + Taxol (135) Carbo (AUC 7.5) + Taxol PFS (months) 13 18 19 21 OS (months) 24 38 49 57 GOG 182: Is there anything to add to Carbo and taxol to improve outcomes? Treatment PFS OS Carbo/Taxol x 8 16.1 40.0 Carbo/Taxol/Gemzar x 8 16.4 40.4 Carbo/Taxol/Doxil every other x 8 16.4 42.8 Carbo/Topo x4 then Carbo/Taxol x 4 15.3 39.1 Carbo/Gemzar x 4 then Carbo/Taxol x 4 15.4 40.2 Does the route of administration make a difference? • GOG 104: patients with optimally debulked stage III disease were randomized to IV cyclophosphamide and IV cisplatin or IV cyclophosphamide and IP cisplatin • IP regimen was superior – 25 vs 20% reponse rate – 49 vs 41 month median survival • Not widely adopted because standard of care shifted to carboplatin/taxol GOG 172: Does IP administration improve results with platinum/taxane therapy? Stage III, all < 1.0 cm RANDOMIZE Cisplatin IV (75 mg/m2) PLUS Paclitaxel IV (135 mg/m2) Paclitaxel (135 mg/m2) IV Day 1 THEN Cisplatin (100 mg/m2) IP Day 2 THEN Paclitaxel (60 mg/m2) IP Day 8 Prolonged remission seen with IP administration Armstrong, NEJM, 2006 Overall survival improved with IP administration Armstrong, NEJM, 2006 GOG 172 participation 86/205 = 41.9% 84/205 = 41.0% Armstrong, NEJM, 2006 IP chemotherapy summary GOG 104 GOG 172 GOG 158 Treatment Cytoxan + Cis IV Cytoxan + Cis IP Cis IV + Taxol Taxol IV + Cis IP + Taxol IP Carbo + Taxol PFS (months) NR NR 18 24 21 OS (months) 41 49 50 66 57 Will targeted therapeutics improve response? • Bevacizumab (Avastin) is an antibody to the vascular endothelial growth factor (VEGF) which blocks the formation of new blood vessels • In phase II trials, Avastin demonstrated significant activity in patients with recurrent ovarian cancer • GOG 218 tested Carboplatin/Taxol/Placebo vs Carboplatin/Taxol/Avastin vs Carboplatin/Taxol/Avastin + maintenance Avastin • Improved progression free survival was seen in the group that got maintenance Avastin • Most patients experience only mild toxicity with Avastin treatment Active GOG trials • GOG 262: Does administering dose-dense Taxol improve the response? – Weekly Taxol vs every three weeks with carboplatin, with or without Avastin • GOG 213: Does Avastin improve the response to chemotherapy for recurrent disease? Does secondary surgical debulking benefit patients? – Randomized to secondary debulking or no surgery – Randomized to Carboplatin/Taxol/Placebo vs Carboplatin/Taxol/Avastin (concurrent and maintenance) • GOG 252: Does Avastin improve response to IP chemotherapy? – IV Carboplatin, IV weekly Taxol, Avastin – IP Carboplatin, IV weekly Taxol, Avastin – IV Taxol (day 1), IP Cisplatin (day 2), IP Taxol (day 8), Avastin • GOG 212: Does monthly Taxol improve survival after primary adjuvant chemotherapy? – Maintenance therapy with Taxol or CT2103 or no treatment for 12 months after primary adjuvant chemotherapy Evolution of a clinical trial: Penn • 2003: T cells in the tumor correlates with improved survival Survival of patients with ovarian cancer: Tumor Infiltrating Lymphocytes (TIL) TIL+ TIL- First Phase I Vaccine Trial • 2006: Dendritic cell vaccine – Goal: to enhance the anti-tumor T cell response – A cellular vaccine comprised of a subject’s own cells primed against ovarian cancer was developed – Confirmed the safety of this approach Second Phase I trial: Whole tumor antigen vaccine • Evidence in other solid tumors of a survival benefit following vaccination with dendritic cells pulsed with tumor lysate • Demonstration of immunomodulatory effects of Avastin and Cytoxan chemotherapy • UPCC 11807 Chemo Bev + CY Whole tumor antigen vaccine - Monocytes GMCSF+IL4 Immature DC Pulsing with Tumor antigen Mature DC An example of disease regression in a patient treated with Avastin and vaccine Pre-treatment Pre-treatment Post-vaccine Nov 2007 Feb 2008 L PAoLN - 1.1x1.5 cm L PAoLN - 0.6 x 1.1 cm PET scan 11807-01 UPCC-11807: Vaccination was safe and welltolerated with evidence of a clinical response •Combination therapy was feasible and well tolerated • Of the six patients enrolled, two had a partial response (PR), 2 had stable disease (SD), and two had progressive disease (PD) • Responses paralleled decreases in serum CA-125 levels. • Evidence of vaccine-specific immune responses were demonstrated Pilot study of T cell transfer following antitumor vaccination UPCC-01808 Bev C/F Bev + CY Phase II Chemo Phase I UPCC-11807 CY CY CY CY CY Goal is to amplify anti-tumor T cells in the lab and then administer large numbers of tumor-specific T cells to the subject along with additional vaccinations and metronomic cytoxan chemotherapy. A second-generation whole tumor vaccine • Growing evidence of the impact of the immunosuppressive tumor environment • Research in the lab demonstrates enhanced immune function with changes in cell preparation • UPCC 11809 Cohort 1 Chemo Cohort 2 Chemo Cohort 3 Chemo Bev UPCC-11809 Eligibility Women with recurrent ovarian, fallopian tube or primary peritoneal cancer Prior cytoreductive surgery yielding tumor for lysate No residual tumor nodules >4.5 cm Good performance status May have received chemotherapy or other therapy after harvest of tumor and prior to enrollment – subjects without evidence of disease after therapy are still eligible Must recover from any toxicities resulting from chemotherapy prior to receiving the vaccine Future Directions New approaches to vaccine development: • Planned clinical trial of intradermal vaccination with killed tumor lysate • Transfer of T cells genetically engineered to recognize tumor • Preclinical data in a mouse model suggests that an antitumor vaccine could be developed using ascites cells – This could have the potential to reduce the cost and increase the availability of immune therapy for women with advanced disease Hurdles • Differences in the characteristics of clinical trial subjects and the general population • Persistent bias • Competition for patients • Research Funding Outcomes continue to improve GOG 111 GOG 158 GOG 104 GOG 172 Carbo (AUC 7.5) + Taxol Cytox an + Cis IV Cytox an + Cis IP Cis IV + Taxol Taxol IV + Cis IP + Taxol IP Cis + Cytoxan Cis + Taxol Cis + Taxol (135) PFS (months) 13 18 19 21 NR NR 18 24 OS (months) 24 38 49 57 41 49 50 66 Treatment For more information • Department of Health and Human Services www.dhhs.gov • FDA (U.S. Food and Drug Administration) www.fda.gov • FDA Center for Drug Evaluation and Research www.fda.gov/cder/ • National Institutes of Health www.nih.gov/ or https://clinicaltrials.gov • NIH: National Cancer Institute www.nci.nih.gov/ • Office of Human Research Protections http://www.hhs.gov/ohrp/ • The University of Pennsylvania – Susan Mauro RN CCRCsusan.mauro@uphs.upenn.edu – Cathi Ybarra, BSN, RN ybarrac@obgyn.upenn.edu Acknowledgements George Coukos, MD, PhD Christina Chu, MD Daniel Powell, PhD Lana Kandalaft, PhD Susan Mauro RN CCRC TRP Clinical Trials Unit 3620 Hamilton Walk Anatomy-Chemistry Bldg B-24 Philadelphia Pa 19104 P: 215-422-2560 susan.mauro@uphs.upenn.edu Cathi Ybarra, BSN, RN GOG Research Program Manager ybarrac@obgyn.upenn.edu The Sandy Rollman Ovarian Cancer Foundation Kaleidoscope of Hope Foundation AACR Scholar-in-Training Award ASCO Young Investigators Award Ovarian Cancer SPORE Paul Calebressi NIH K12 Training Grant The Florence and Marshall Schwid Ovarian Cancer Research Grant from the Gynecologic Cancer Foundation