Radionuclide Pulmonary imaging lecture 3
advertisement

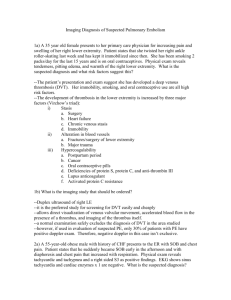
Radionuclide Pulmonary imaging (LUNG V/Q SCAN) Dr Hussein Farghaly Nuclear Medicine Consultant RMH ACUTE PULMONARY EMBOLISM CLINICAL PRESENTATION: (Non-specific) • Haemoptysis, Dyspnea and Pleuritic Chest pain (Virchows triad) • Back or Abdominal pain, cough, SOB, Lowgrade fever,---------• May be asympotmatic Evaluation • ABG – Respiratory alkalosis, hypoxia • ECG – Sinus tachycardia & S1Q3T3 • D-Dimer • CXR • Spiral CT with contrast • V/Q Scan • Angiogram Question 1 Pulmonary angiography as “gold standard” Sensitivity for PE is: • 97% • 93% • 87% Question 2 Accuracy of V/Q scan in PIOPED – incorrect answer? • 98% sensitivity • 10% specificity • High-probability V/Q scans as PE criteria: Failed to detect PE in 59% of patients • 70% specificity Question 3 Accuracy of multiple slice CTA – incorrect answer? • Variable sensitivities from 53% to 87% in different studies • Reader’s experience is important • Specificity > 90% • Sensitivity is higher than specificity Question 4 Diagnostic accuracy of CTA – incorrect answer? • Dependent on clinical probability for PE • CTA has high NPV similar to that at V/Q scan • Independent from clinical probability for PE Diagnostic Pathways in Acute Pulmonary Embolism Recommendations of The PIOPED II Investigators Diagnostic Pathways in Acute Pulmonary Embolism Pre Imaging Objective clinical probability • Three clinical scoring system have been tested prospectively and validated in large scale clinical trials: Wells’ score (Ann Intern Med 1998) Geneva Score (Arch Intern Med 2001, Ann Intern Med 2006) Pisa Score (Ann Respir Crit Care Med 1999, Ann j Med 2003) The diagnostic yield of D-Dimer is lower in cancer patient, the elderly, inpatient, recent trauma or surgery and during pregnancy CHEST X- Ray • Initial CXR usually normal. • May progress to show atelectasis, plueral effusion and elevated hemidiaphram. • Hampton’s hump and Westermark signs are classic findings but are not usually present. • Hampton’s Hump – consists of a pleura based shallow wedgeshaped consolidation in the lung periphery with the base against the pleural surface. • Westermark sign – Dilatation of pulmonary vessels proximal to embolism along with collapse of distal vessels, often with a sharp cut off. Lung V/Q scan • Should lung scan be omitted for pulmonary embolism diagnosis in the age of multislice spiral CT? A) YES B) NO NO, Lung scan has a role in PE diagnosis When there are: Contraindications to CT Scan: Allergy to iodinated contrast agent Renal failure Pregnancy? High diagnostic yield and avoidance of unnecessary radiation exposure. Pregnancy Young patient with normal X-ray. Interpretation Criteria of V/Q scan - Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED), 1990 - Revised PIOPED, 1995 - PISA-PED, 1996: Perfusion scan only - PIOPED II , 2006 - Modified PIOPED II : perfusion and CXR PIOPED • 933/1,493 patients analyzed • 755 of these patients with pulmonary angiography within 12– 24 h of V/Q scan • Posterior xenon-133 ventilation scan, followed by an 8-view Tc-99m MAA perfusion lung scan • One-year follow-up: New PE, major bleeding complications, or death 1Value of the ventilation/perfusion scan in acute pulmonary embolism. Results of the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED). The PIOPED Investigators. JAMA 1990; 263:2753-9 PIOPED: Probability of PE V/Q scan accuracy: PIOPED • Based on PA: 98% sensitivity and 10% specificity for V/Q scan • High-probability V/Q scans (V/Q mismatch) as criteria for PE: Failed to detect PE in 59% of patients, based on PA. Likelihood of PE: PIOPED Predictive values > 90%: Only 22% of patients. Combined V/Q scan and clinical probability: Highest diagnostic accuracy. High clinical probability & high-probability V/Q scan: 95% likelihood of PE. Low clinical probability & low-probability V/Q scan: 4% likelihood of PE. PISA-PED, 1996: Perfusion scan only • 890 patients with Q scan, compared with PA • 413/670 (62%) patients with abnormal Q scans had PA; no PA if normal/near normal Q scan • 92% sensitivity and 87% specificity • Positive Q scan and high clinical suspicion: PPV >90% • Negative Q scan and low clinical suspicion: NPV of 97%. Pisa Ped perfusion scan categories and interpretation criteria Normal Near normal No perfusion defects of any kind Perfusion defects smaller or equal in size and shape to the following roentgenographic abnormalities: cardiomegaly, enlarged aorta, hila and mediastinum, elevated diaphragm, blunting of the costophrenic angle, pleural thickening, intrafissural collection of liquid. Abnormal compatible Single or multiple wedge-shaped perfusion defects with or with pulmonary without matching chest-roentgenographic adnormalities. embolism (PE+) Wedge-shaped areas of overperfusion usually coexist. Abnormal not Single or multiple perfusion defects other than wedge-shaped compatible with with or without matching chest-roentgenographic pulmonary embolism abnormalities. Wedge-shaped areas of overperfusion are (PE-) usually not seen. Miniati M, et al: Value of perfusion lung scan in the diagnosis of pulmonary embolism: Results of the Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis (PISA-PED). Am J Respir Crit Care Med 1996;154:1387–1393. PISA-PED: Conclusion • Q scanning alone: Much closer to angiography than V/Q scanning • Q scanning rather than V/Q scanning: Imaging technique of first choice for diagnosis of PE PIOPED II: V/Q scan results • PE present or PE absent: 74% (PISA-PED: 75%) • Sensitivity for PE present: 77% (CTA: 83%) • Specificity of PE absent: 98% (CTA: 98%) Conclusions: V/Q scan provides definitive diagnosis in a majority of patients (74%) Sostman HD, et al. Acute pulmonary embolism: sensitivity and specificity of ventilation perfusion scintigraphy in PIOPED II study. Radiology 2008; 246: 941-946 Causes of perfusion defects Primary vascular lesions: Mismatch Q/V Pulmonary thrombpembolism Septic, fat and air emboli PA hypoplesia or atresia Vasculitis Primary ventilation Abnormality Pneumonia Atelectasis pulmonary edema Asthma COPD, Emphysema, Chronic bronchitis Bullae Mass Effect: Tumor Adenopathy Mismatch Q/V Pleural effusion Iatrogenic Surgery: pneumonectomy, lobectomy Radiation fibrosis: Mismatch Q/V Causes of Nonsegmental perfusion defects Pacemaker artifact Tumors Pleural effusion Trauma Hemorrhage Bullae Cardiomegaly Hilar adenopathy Atelectasis Pneumonia Aortic ectasia or aneurysm Stripe Sign: A thin line (stripe) of activity between a Q defect and adjacent pleural surface: sometime in emphysema. Only 6% prevalence of PE. Triple match: Matching Q and V defect, and CXR abnormality, regardless of size: Atelectasis, consolidation. Prevalence of PE: 26% (upper - 11%; middle 12%; lower - 33%)1 Focal Hot Spots on Perfusion Scan