PEDIATRIC HIP FRACTURES - Orthopaedic Trauma Association
advertisement
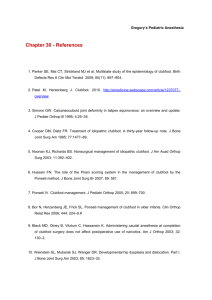
Fractures and Dislocations about the Hip in the Pediatric Patient Joshua Klatt, MD Original Author: Mark Tenholder, MD; March 2004 Revised: Steven Frick, MD; August 2006 Harish Hosalkar, MD; April 2011 Joshua Klatt, MD; November 2011 “Hip fractures in children are of interest because of the frequency of complications rather than the frequency of fractures.” Canale Femoral Neck Fractures in Children Rare fracture Anatomic and vascular differences Emergent treatment High complication rate Background Different from Adults – – – – – High-energy Thick periosteum Vascularity Physes Treatment options Background Osseous Anatomy – Proximal femoral physis – Trochanteric apophysis – Dense bone – Small neck Background Vascular Anatomy – Immature – Variable Ligamentum teres Lateral epiphyseal vessels (bypass physis) Metaphyseal circulation (after physeal closure) – Vulnerable to injury Mechanism MVC Auto-ped High falls Minor trauma can still be a cause Classification Type 1 – Transepiphyseal Type 2 – Transcervical Type 3 – Cervicotrochanteric Type 4 - Intertrochanteric Colonna PC. Fractures of the neck of the femur in children. Am J Surg 1929;6:793-7. Type I Transepiphyseal Type I Very rare Little evidence High risk of AVN (up to 100% in some series) Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977 Jun.;59(4):431–443. Type I Treatment Nondisplaced – Can treat with spica cast Displaced – Past Closed reduction and spica ORIF – Present Closed or open reduction plus internal fixation – Threaded pins – Cannulated screws – Smooth pins Forlin E, Guille JT, Kumar SJ, Rhee KJ. Transepiphyseal fractures of the neck of the femur in very young children. J Pediatr Orthop. 1992 Feb.;12(2):164–168. Type I Results Recent literature following better understanding of hip vascularity In some circumstances the femoral head may not be completely avascular, and, with appropriate surgical care, the hip can be preserved Schoenecker JG, Kim Y-J, Ganz R. Treatment of traumatic separation of the proximal femoral epiphysis without development of osteonecrosis: a report of two cases. The Journal of Bone and Joint Surgery. 2010 Apr.;92(4):973–977. Type I Example 10 yr female Type I fracturedislocation of hip Type I Example ORIF and Pins Attempted Type I Example Postop film Malreduced and dislocated Type I Example Repeat ORIF Type I Example 3 month follow-up Type I Example 8 Months Heterotopic ossification evident Type I Example 11 Months Osteonecrosis Type II Transcervical Type II Most common type (50% of peds hip fx) Most common AVN (50%) 3/4 will be displaced Type II Nondisplaced Displaced Lam (1971) Traction/Cast Traction/CR Cast Ratliff (1962) Cast IF Canale (1977) IF IF Quick (2005) IF CR vs OR with IF Historical treatment Internal fixation is currently the treatment of choice Lam. Fractures of the neck of the femur in children. J Bone Joint Surg Am. 1971;53:1165–1179. Ratliff. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962;44-B:528–542. Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977;59:431–443. Quick. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;(432):87–96. Type II Treatment Nondisplaced – Spica cast, if young – Use internal fixation, if older – If in doubt, treat as displaced Type II Treatment Displaced – Anatomic reduction is important, open if necessary Do not accept varus malreductions – Avoid excess traction Fracture table may be used without extreme positioning for prolonged period – Cannulated screws/ threaded pins to compress – Avoid physis But stability and reduction is first priority Type II Results Nondisplaced – Fewer complications Outcome in literature is variable – AVN in up to 50% Highest complication rate of the 4 types Improved with internal fixation İnan U, Köse N, Ömeroğlu H. Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009 May 26;3(4):259–264. Type III Cervicotrochanteric Type III Second most common – 35% of peds hip fx Second highest AVN rate – 25-30% 2/3 displaced İnan U, Köse N, Ömeroğlu H. Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009 May 26;3(4):259–264. Type III Treatment Nondisplaced – Spica cast – Follow closely for loss of reduction Displaced ORIF – Cannulated screws – Peds hip screw Avoid physes İnan U, Köse N, Ömeroğlu H. Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009 May 26;3(4):259–264. Type III Results Slightly better than II Nondisplaced – Fewer complications Outcome in literature is variable – AVN in up to 30% IF reduces coxa vara and nonunion Flynn. Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002;84:108–112. Type III Example 6 year old femal MVC Liver laceration Ipsilateral femoral neck, femur, and tibia fractures Type III Example Type III Example 8 wks post-op Union Cast removed, WBAT No AVN Type IV Intertrochanteric Type IV Not common – 10-15% of peds hip fx Fewest complications AVN still possible, but unusual Type IV Treatment Most agreement between authors Nondisplaced – Hip-spica in younger patients Displaced – Pediatric hip screw in older pts – Or in those with unstable reduction Type IV Results Generally good Fewest complications – High energy still can result in AVN (1020%) Type IV Example 14 year old male Motorcycle crash Type IV Example Type IV Example 9 weeks post-op Type IV Example 9 months post-op Type IV Example 10 months post-op After hardware removal Type IV Example 15 months post-op AVN Hip Fracture Treatment Highlights Data on nondisplaced fractures is limited – Conclusions are difficult Most nondisplaced fractures can be treated in a cast Exceptions – Older child – Type II Hip Fracture Treatment Highlights Surgery and implants available now are different than those used in older literature More recent emphasis on internal fixation – Anatomic reduction and compression is key for successful union Surgical approach should not further destabilize blood supply to femoral head Expanded indications in polytrauma pt’s Hip Fracture Complications AVN Coxa Vara Physeal Closure Nonunion Delayed Union Ratliff 42% 20% 15% 10% 24% Lam 17% 30% 15% Canale 43% 21% 62% 10% 7% Lam. Fractures of the neck of the femur in children. J Bone Joint Surg Am. 1971;53:1165–1179. Ratliff. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962;44-B:528–542. Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977;59:431–443. Hip Fracture AVN Most common and devastating complication Hip Fracture AVN 6 – 53% overall rate Type I Type II Type III Type IV 57% to 100% 50% 25% 10% Quick TJ, Eastwood DM. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;432:87–96. Hip Fracture AVN AVN may develop if – The vessels are torn in the initial injury – The vessels are kinked at due to displacement – There is intracapsular tamponade causing vascular disruption – The vessels are not protected during healing Quick TJ, Eastwood DM. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;432:87–96. Hip Fracture AVN Factors influencing rate of AVN – – – – – – Degree of initial displacement Timing of reduction and fixation Quality of reduction Stability of reduction and fixation Decompression of capsular hematoma Weight-bearing status Quick TJ, Eastwood DM. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;432:87–96. AVN Classification Ratliff 1962 Ratliff A. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962 Aug.;44-B:528–542. AVN Risk Factors Degree of Initial Displacement Timing of reduction Nondisplaced Less than 24 hours – None in most series Displaced – 43% to 88% rate -Mirdad. Fractures of the neck of femur in children: an experience at the Aseer Central Hospital, Abha, Saudi Arabia. Injury. 2002;33:823. -Morsy. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001;32:45. -Forlin. Transepiphyseal fractures of the neck of the femur in very young children. J Pediatr Orthop. 1992;12:164. – 0% to 6% Greater than 48 hours – 40% -Cheng. Decompression and stable internal fixation of femoral neck fractures in children can affect the outcome. J Pediatr Orthop. 1999;19:338. -Flynn. Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002;84:108. -Shrader. Femoral Neck Fractures in Pediatric Patients. Clin Orthop Relat Res. 2007;454:169. AVN Risk Factors Quality of reduction Excellent/anatomic reduction – 0% to 17% AVN Nonanatomic/fair/poor Capsular decompression No decompression – 50% Decompression – 0% to 10% – 70% to 100% AVN -Morsy. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001;32:45. -Shrader. Femoral Neck Fractures in Pediatric Patients. Clin Orthop Relat Res. 2007;454:169. -Cheng. Decompression and stable internal fixation of femoral neck fractures in children can affect the outcome. J Pediatr Orthop. 1999;19:338. -Ng. Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury. 1996;27:419. Coxa Vara 20-50% incidence Loss of reduction, closure of proximal femoral physis Incidence and amount of deformity decreased by internal fixation Gait abnormalities, degeneration Tx: Subtrochanteric osteotomy Eberl. Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthop. 2010 Aug.;81(4):442–445. Nonunion 5-10% incidence Less with internal fixation Treatment – Valgus osteotomy – Bone graft -Bagatur. Complications associated with surgically treated hip fractures in children. J Pediatr Orthop B. 2002;11:219. -Quick. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;432:87. Physeal Closure Variable incidence (up to 40%) Causes: AVN, implants, stimulation Leg length discrepancy often not significant, worse with AVN Tx: Contralateral distal femoral epiphysiodesis -Morsy. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001;32:45. Summary Determine Delbet type and displacement Urgent treatment with reduction and fixation as needed Treatment and implant will also be dependent on age Joint decompression has theoretical advantages, and some literature support but quality of evidence poor Summary Nondisplaced fractures will have fewer complications and will do better regardless of treatment. The more proximal the fx, the more likely to get AVN Complication rate is high. Counsel the family. Summary Internal fixation is indicated in: – – – – Displaced type I All type II Types III and IV if displaced or child is older Polytrauma Internal fixation may reduce complications Hip Dislocations Uncommon, but more common than femoral neck fractures in children Usually posterior, rarely anterior Less commonly associated with fractures than adults Results better than in adults Still potential for osteonecrosis and poor outcome Herrera-Soto. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg. 2009;17:15. Hip Dislocations Urgent reduction, closed Adequate anesthesia, relaxation Careful assessment of congruity of reduction If uncertain consider CT/MRI to rule out intraarticular fragments Protected weight-bearing following reduction until full, painless ROM Hip Dislocations Treatment Operative indications – Delayed treatment – Irreducible dislocation – Incongruous or incomplete reduction with interposed bone or soft tissue Hip Dislocations Treatment Open Reduction Approaches – Anterior (Smith-Peterson) – Anterolateral (Watson-Jones) – Trans-trochanteric Avoid posterior to prevent damage to the blood-vessels and potentially-preserved vascularity of the femoral head Trochanteric flip approach Hip Dislocations Complications Complications – – – – Avascular necrosis (8-20%) Myositis ossificans (8-15%) Sciatic nerve palsy Early secondary arthritis Factors predisposing to poor result: – – – – – Older child Severe trauma Delay in reduction (> 8 hours) Incongruous reduction AVN Herrera-Soto. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg. 2009;17:15. Hip Dislocations Summary Early diagnosis and prompt reduction Important to recognize associated fracture/ inadequate reduction Advanced imaging may be necessary Surgical approach should not further compromise blood supply AVN is still a significant risk with 8-20% incidence in skeletally immature Delay in reduction, high energy mechanism, and older age are risk factors Herrera-Soto. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg. 2009;17:15. Hip Dislocations Example 1 Hip Dislocations Example 1 Hip Dislocations Example 1 Hip Dislocations Example 1 After anterolateral open reduction Hip Dislocations Example 2 12 yr male with reduced hip dislocation and increased medial joint space Hip Dislocations Example 2 Inadequate reduction due to interposition Hip Dislocations Example 2 Open surgical dislocation: Trochanteric flip approach Hip Dislocations Example 2 Intra-articular loose tissue (post-labral piece) Hip Dislocations Example 2 6 month follow-up Hip Dislocations Example 2 15 month follow-up. No evidence of AVN. Bibliography Bagatur AE, Zorer G. Complications associated with surgically treated hip fractures in children. J Pediatr Orthop B. 2002 Jul.;11(3):219–228. Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977 Jun.;59(4):431–443. Cheng JC, Tang N. Decompression and stable internal fixation of femoral neck fractures in children can affect the outcome. J Pediatr Orthop. 1999 Apr.;19(3):338–343. Colonna PC. Fractures of the neck of the femur in children. Am J Surg 1929;6:793-7. Eberl R, Singer G, Ferlic P, Weinberg AM, Hoellwarth ME. Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthop. 2010 Aug.;81(4):442–445. Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS. Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002 Jan.;84(1):108–112. Forlin E, Guille JT, Kumar SJ, Rhee KJ. Transepiphyseal fractures of the neck of the femur in very young children. J Pediatr Orthop. 1992 Feb.;12(2):164–168. Herrera-Soto JA, Price CT. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg. 2009 Jan.;17(1):15–21. İnan U, Köse N, Ömeroğlu H. Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009 May 26;3(4):259–264. Lam SF. Fractures of the neck of the femur in children. J Bone Joint Surg Am. 1971 Sep.;53(6):1165– 1179. Bibliography Mirdad T. Fractures of the neck of femur in children: an experience at the Aseer Central Hospital, Abha, Saudi Arabia. Injury. 2002 Nov.;33(9):823–827. Morsy HA. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001 Jan.;32(1):45–51. Ng GP, Cole WG. Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury. 1996 Jul.;27(6):419–421. Quick TJ, Eastwood DM. Pediatric Fractures and Dislocations of the Hip and Pelvis. Clin Orthop Relat Res. 2005;(432):87–96. Ratliff A. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962 Aug.;44-B:528– 542. Schoenecker JG, Kim Y-J, Ganz R. Treatment of traumatic separation of the proximal femoral epiphysis without development of osteonecrosis: a report of two cases. J Bone and Joint Surg. 2010 Apr.;92(4):973–977. Shrader MW, Jacofsky DJ, Stans AA, Shaughnessy WJ, Haidukewych GJ. Femoral Neck Fractures in Pediatric Patients. Clin Orthop Relat Res. 2007 Jan.;454:169–173. Thank You If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an e-mail to ota@aaos.org E-mail OTA about Questions/Comments Return to Pediatrics Index