Gregory`s Pediatric Anesthesia Chapter 30
advertisement
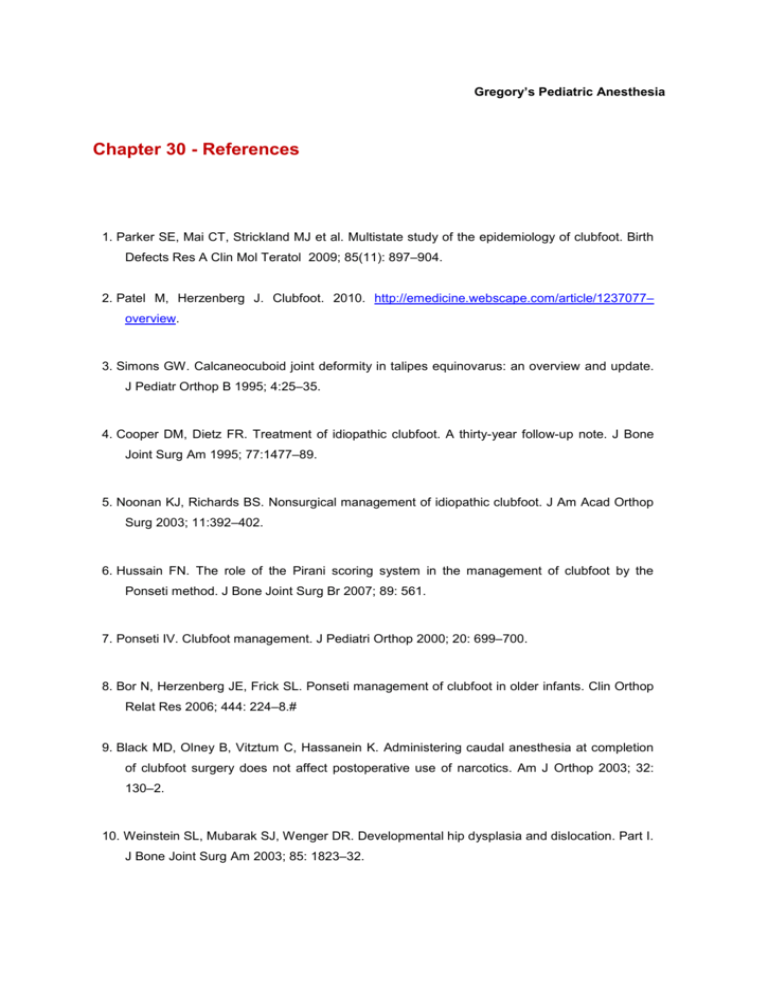
Gregory’s Pediatric Anesthesia Chapter 30 - References 1. Parker SE, Mai CT, Strickland MJ et al. Multistate study of the epidemiology of clubfoot. Birth Defects Res A Clin Mol Teratol 2009; 85(11): 897–904. 2. Patel M, Herzenberg J. Clubfoot. 2010. http://emedicine.webscape.com/article/1237077– overview. 3. Simons GW. Calcaneocuboid joint deformity in talipes equinovarus: an overview and update. J Pediatr Orthop B 1995; 4:25–35. 4. Cooper DM, Dietz FR. Treatment of idiopathic clubfoot. A thirty-year follow-up note. J Bone Joint Surg Am 1995; 77:1477–89. 5. Noonan KJ, Richards BS. Nonsurgical management of idiopathic clubfoot. J Am Acad Orthop Surg 2003; 11:392–402. 6. Hussain FN. The role of the Pirani scoring system in the management of clubfoot by the Ponseti method. J Bone Joint Surg Br 2007; 89: 561. 7. Ponseti IV. Clubfoot management. J Pediatri Orthop 2000; 20: 699–700. 8. Bor N, Herzenberg JE, Frick SL. Ponseti management of clubfoot in older infants. Clin Orthop Relat Res 2006; 444: 224–8.# 9. Black MD, Olney B, Vitztum C, Hassanein K. Administering caudal anesthesia at completion of clubfoot surgery does not affect postoperative use of narcotics. Am J Orthop 2003; 32: 130–2. 10. Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation. Part I. J Bone Joint Surg Am 2003; 85: 1823–32. 11. Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000; 8: 232–42. 12. McKinnon B, Bosse MJ, Browing WH. Congenital dysplasia of the hip: the lax (subluxatable) newborn hip. J Pediatr Orthop 1984; 4: 422–6. 13. Pavlik A. The functional method of treatment using a harness with stirrups as the primary method of conservative therapy for infants with congenital dislocation of the hip. Clin Orthop 1992; 281: 4–10. 14. Gage JR, Winter RB. Avascular necrosis of the capital femoral epiphysis as a complication of the closed reduction of congenital dislocation of the hip. A critical review of twenty years’ experience at Gillette Children’s Hospital. J Bone Joint Surg Am 1972; 54: 373–88. 15. Quinn RH, Renshaw TS, DeLuca PA. Preliminary traction in the treatment of developmental dislocation of the hip. J Pediatr Orthop 1994; 14: 636–42. 16. Gillingham BL, Sanchez MC, Wenger DR. Pelvic osteotomies for the treatment of hip dysplasia in children and young adults. J Am Acad Orthop Surg 1999; 7: 325–37. 17. Galpin RD, Roach JW, Wenger DR et al. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am 1989; 71: 734– 41. 18. Tonnis D. An evaluation of conservative and operative methods in the treatment of congenital hip dislocation. Clin Orthop 1976; 119: 76–88. 19. Wheeles C. Hip spica cast. www.wheelsessonline.com/ortho/hip_spica_cast. 20. Miller ME, Bramlet KW, Kissell EU, Niemann KM. Improved treatment of femoral shaft fractures in children. The “pontoon” 90–90 spica cast. Clin Orthop 1987; 219: 140–6. 21. Blount WP. Tibia vara, osteochondrosis deformans tibiae. J Bone Joint Surg 1937; 19: 1–29. 22. Bradway JK, Klassen RA, Peterson HA. Blount disease: a review of the English literature. J Pediatr Orthop 1987; 7: 472–80. 23. DeOrio MJ, DeOrio JK. Blount disease: treatment. http://emedicine.medscape.com/article/1250420. 24. Hofmann A, Jones RE, Herring JA. Blount’s disease after skeletal maturity. J Bone Joint Surg Am 1982; 64: 1004–9. 25. Henderson RC. Tibia vara: a complication of adolescent obesity. J Pediatr 1992; 121: 482–6. 26. Sabharwal S, Zhao C, McClemens E. Correlation of body mass index and radiographic deformities in children with Blount disease. J Bone Joint Surg Am 2007; 89: 1275–83. 27. Zionts LE, Shean CJ. Brace treatment of early infantile tibia vara. J Peditr Orthop 1998; 18: 102–9. 28. Rab GT. Oblique tibial osteotomy for Blount’s disease. J Pediatr Orthop 1988; 8: 715–20. 29. Andrade N, Johnston CE. Medial epiphysiolysis in severe infantile tibia vara. J Pediatr Orthop 2006; 26: 652–8. 30. Birch JG, Buech MF, Roach JW. Lateral tibia epiphysiodesis for adolescent Blount’s disease. Orthop Trans 1992; 16: 14. 31. Loder RT. The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop 1996; 322: 8–27. 32. Loder RT, Wittenberg B, DeSilva G. Slipped capital femoral epiphysis associated with endocrine disorders. J Pediatr Orthop 1995; 15: 349–56. 33. Loder RT, Hensinger RN. Slipped capital femoral epiphysis associated with renal failure osteodystrophy. J Pediatr Orthop 1997; 17: 205–11. 34. Murray AW, Wilson NI. Changing incidence of slipped capital femoral epiphysis: a relationship with obesity? J Bone Joint Surg Br 2008; 90: 92–4. 35. Kennedy JG, Hresko MT, Kasser JR et al. Osteonecrosis of the femoral head associated with slipped capital femoral epiphysis. J Pediatr Orthop 2001; 21: 189–93. 36. Peterson MD, Weiner DS, Green NE, Terry CL. Acute slipped capital femoral epiphysis: the value and safety of urgent manipulative reduction. J Pediatr Orthop 1997; 17: 648–54. 37. Gholve PA, Cameron DB, Millis MB. Slipped capital femoral epiphysis update. Curr Opin Pediatr 2009; 21: 39–45. 38. Jerre R, Billing L, Hansson G, Wallin J. The contralateral hip in patients primarily treated for unilateral slipped upper femoral epiphysis. Long-term follow-up of 61 hips. J Bone Joint Surg Br 1994; 76: 563–7. 39. Riad J, Bajelidze G, Gabos PG. Bilateral slipped capital femoral epiphysis: predictive factors for contralateral slip. J Pediatr Orthop 2007; 27: 411–14. 40. Weiner DS, Weiner S, Melby A, Hoyt WA Jr. A 30-year experience with bone graft epiphysiodesis in the treatment of slipped capital femoral epiphysis. J Pediatr Orthop 1984; 4: 145–52. 41. Ikuta Y. Thumb duplication. In: Buck-Gramcko D (ed) Congenital Malformations of the Hand and Forearm. London: Churchill Livingstone, 1998, pp. 225–35. 42. Manske PR, Goldfarb CA. Congenital failure of formation of the upper limb. Hand Clin 2009; 25: 157–70. 43. Kozin SH. Upper-extremity congenital anomalies. J Bone Joint Surg Am 2003; 85A: 1564– 76. 44. Netscher DT, Scheker LR. Timing and decision-making in the treatment of congenital upper extremity deformities. Clin Plast Surg 1990; 17: 113–31. 45. McCarroll HR. Congenital anomalies: a 25-year overview. J Hand Surg Am 2000; 25: 1007– 37. 46. Laub DR Jr, Ladd AL, Hentz VR. Congenital hand anomalies. In: Russell RC (ed) Plastic Surgery: Indications, Operations and Outcomes, vol. IV. St Louis, MO: Mosby, 2000, pp. 1735–48. 47. Netscher DT. Congenital hand problems. Terminology, etiology, and management. Clin Plast Surg 1998; 25: 537–52. 48. Wood VE. Congenital thumb deformities. Clin Orthop 1985; 195: 7–25. 49. James MA, McCarroll HR Jr, Manske PR. The spectrum of radial longitudinal deficiency: a modified classification. J Hand Surg Am 1999; 24: 1145–55. 50. Netscher DT, Baumholtz MA. Treatment of congenital upper extremity problems. Plast Reconstr Surg 2007; 119:101e–129e. 51. Evans H, Steele MS, Nielsen KC et al. Peripheral nerve blocks and continuous catheter techniques. Anesthesiol Clin North Am 2005; 23: 141–62. 52. Rawal N, Allvin R, Amilon A et al. Postoperative analgesia at home after amulatory hand surgery: a controlled comparison of tramadol, metamizol, and paracetamol. Anesth Analg 2001; 92: 347–51. 53. Rose JB, Finkel JC, Arquedas-Mohs A et al. Oral tramadol for the treatment of pain of 7–30 days duration in children. Anesth Analg 2003; 96: 78–81. 54. Loder RT, O’Donnell PW, Feinber JR. Epidemiology and mechanism of femur fractures in children. J Pediatr Orthop 2006; 26: 561–66. 55. Kasser JR, Beaty JH. Femoral shaft fractures. In: Beaty JH, Kasser JR (eds) Fractures in Children. Philadelphia: Lippincott Williams and Wilkins, 2006, pp. 893–936. 56. Anglen J, Choi L. Treatment options in pediatric femoral shaft fractures. J Orthop Trauma 2005; 19: 724–33 57. Epps HR, Molenaar E, O’Connor DP. Immediate single-leg spica cast for pediatric femoral diaphysis fractures. J Pediatr Orthop 2006; 26: 491–6. 58. Buehler KC, Thompson JD, Sonseller PD et al. A prospective study of early spica casting outcomes in the treatment of femoral shaft fractures in children. J Pediatr Orthop 1995; 15: 30–5. 59. Crist BD, della Rocca GJ, Murtha YM. Treatment of acute distal femur fractures. Orthopedics 2008; 31: 681–90. 60. Heinrich SD, Dravaric DM, Darr K, MacEwen GD. The operative stabilization of pediatric diaphyseal femur fractures with flexible intramedullary nails: a prospective analysis. J Pediatr Orthop 1994; 14: 501–7. 61. Bar-On E, Sagiv S, Porat S. External fixation or flexible intramedullary nailing for femoral shaft fractures in children. A prospective randomized study. J Bone Joint Surg Br 1997; 79: 975–78. 62. Morshed S, Humphrey M, Corrales LA. Retention of flexible intramedullary nails following treatment of pediatric femur fractures. Arch Orthop Trauma Surg 1997; 127: 509–14. 63. Rabin SI, Carlson D, Rabin SL. Complications of supracondylar femur fractures. Loyola U Orthop J 1995; 4: 30–8. 64. Paterson MP, Hoffman EB, Roux P. Severe disseminated staphylococcal disease associated with osteitis and septic arthritis. J Bone Joint Surg Br 1990; 72: 94–7. 65. Frank G, Mahoney HM, Eppes SC. Musculoskeletal infections in children. Pediatr Clin North Am 2005; 52: 1083–6. 66. Peltola H, Kallio MJ, Unkila-Kallio L. Reduced incidence of septic arthritis in children by Hemophilus influenzae type-b vaccination. Implications for treatment. J Bone Joint Surg Br 1998; 80: 471–3. 67. Arnold SR, Elias D, Buckingham SC et al. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J Pediatr Orthop 2006; 26: 703–8. 68. Moylett EH, Rossman SN, Epps HR, Demmler GJ. Importance of Kingella kingae as a pediatric pathogen in the United States. Pediatr Infect Dis J 2000; 19: 263–5. 69. Song J, Letts M, Monson R. Differentiation of psoas muscle abscess from septic arthritis of the hip in children. Clin Orthop Relat Res 2001; 391: 258–65. 70. Caird MS, Flynn JM, Leung YL et al. Factors distinguishing septic arthritis from transient synovitis of the hip in children. A prospective study. J Bone Joint Surg Am 2006; 88: 1251–7. 71. Yagupsky P, Bar-Ziv Y, Howard CB, Dagan R. Epidemiology, etiology and clinical features of septic arthritis in children younger than 24 months. Arch Pediatr Adolesc Med 1995; 149: 537–40. 72. Baujat G, Lebre AS, Cormier-Daire V, Le Merrer M. Osteogenesis imperfecta, diagnosis information (clinical and genetic classification). Arch Pediatr 2008; 15: 789–91. 73. Sillence D. Osteogenesis imperfecta: an expanding panorama of variants. Clin Orthop 1981; 159: 11–25. 74. Glorieux FH, Bishop NJ, Plotkin H et al. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med 1998; 339: 947–52. 75. Zeitlin L, Fassier F, Glorieux FH. Modern approach to children with osteogenesis imperfecta. J Pediatr Orthop B 2003; 12: 77–87. 76. Jones D, Hosalkar H, Jones S. The orthopaedic management of osteogenesis imperfecta. Clin Orthop 2002; 16: 374–88. 77. Cole WG. Advances in osteogenesis imperfecta. Clin Orthop 2002; 401: 6–16. 78. Burnett YL, Brennan MP, Klowden AJ et al. Pulse oximetry and blood pressure monitoring: effect of automatic tourniquets and automatic noninvasive blood pressure devices on inducing fractures in pediatric patients with osteogenesis imperfecta. Anesthesiology 1994; 81(3A): A508. 79. Darin N, Kimber E, Kroksmark AK, Tulinius M. Multiple congenital contractures: birth prevalence, etiology, and outcome. J Pediatr 2002; 140: 61–7. 80. Hall JG. Arthrogryposis multiplex congenita: etiology, genetics, classification, diagnostic approach, and general aspects. J Pediatr Orthop B 1997; 6: 159–66. 81. Chen H, Blackburn WR, Wertelecki W. Fetal akinesia and multiple perinatal fractures. Am J Med Genet 1995; 55: 472–7. 82. Banker BQ. Neuropathologic aspects of arthrogryposis multiplex congenita. Clin Orthop 1985; 194: 30–43. 83. Mennen U, van Heest A, Ezaki MB et al. Arthrogryposis multiplex congenita. J Hand Surg Br 2005; 30: 468–74. 84. Bamshad M, van Heest AE, Pleasure D. Arthrogryposis: a review and update. J Bone Joint Surg Am 2009; 91 Suppl 4: 40–6. 85. Bevan WP, Hall JG, Bamshad M et al. Arthrogryposis multiplex congenita (amyoplasia): an orthopaedic perspective. J Pediatr Orthop 2007; 27: 594–600. 86. Palmer PM, MacEwen GD, Bowen JR, Mathews PA. Passive motion therapy for infants with arthrogryposis. Clin Orthop Relat Res 1985; 194: 54–9. 87. Thompson GH, Bilenker RM. Comprehensive management of arthrogryposis multiplex congenita. Clin Orthop 1985; 194: 6–14. 88. Staheli LT, Chew DE, Elliott JS. Management of hip dislocations in children with arthrogryposis. J Pediatr Orthop 1987; 7: 681–5. 89. Bennett JB, Hansen PE, Granberry WM. Surgical management of arthrogryposis in the upper extremity. J Pediatr Orthop 1985; 5: 281–6. 90. Longo M, Hankins GD. Defining cerebral palsy:pathogenesis, pathophysiology and new intervention. Minerva Ginecol 2009; 61: 421–9. 91. Delgado MR, Hirtz D, Aisen M et al. Practice parameter: pharmacologic treatment of spasticity in children and adolescents with cerebral palsy (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2010; 74: 336–43. 92. Hepaguslar H, Ozzeybek D, Elar Z. The effect of cerebral palsy on the action of vecuronium with or without anticonvulsants. Anaesthesia 1999; 54: 593–6. 93. Dierdorf SF, McNieceWL, Rao CC. Effect of succinylcholine on plasma potassium in children with cerebral palsy. Anesthesiology 1985; 62: 88–90. 94. Theroux MC, Brandom BW, Zagnoev M et al. Dose response of succinylcholine at the adductor pollicis of children with cerebral palsy during propofol and nitrous oxide anesthesia. Anesth Analg 1994; 79: 761–5. 95. Martyn JA, White DA, Gronert GA et al. Up- and down-regulation of skeletal muscle acetylcholine receptors. Effects on neuromuscular blockers. Anesthesiology 1992; 76: 822– 43. 96. Theroux MC, Akins RE, Barone C et al. Neuromuscular junctions in cerebral palsy: presence of extrajunctional acetylcholine receptors. Anesthesiology 2002; 96: 330–5. 97. Driessen J. Neuromuscular and mitochondrial disorders: what is relevant to the anesthesiologist? Curr Opin Anaesthesiol 2008; 21: 350–5. 98. Hayes J, Veyckemans F, Bissonnette B. Duchenne muscular dystrophy: an old anesthesia problem revisited. Pediatr Anesth 2008; 18: 100–6. 99. Footitt EJ, Sinha MD, Raiman JAJ et al. Mitochondrial disorders and general anaesthesia: a case series and review. Br J Anaesth 2008; 100: 436–41. 100. Ohtani Y, Mike T, Ishitsu T et al. A case of malignant hyperthermia with mitochondrial dysfunction. Brain Dev 1985; 7: 249. 101. Fricker RM, Raffelsberger T, Rauch-Shorny S et al. Positive malignant hyperthermia susceptibility in vitro test in a patient with mitochondrial myopath and myoadenylate deaminase deficiency. Anesthesiology 2002; 97: 1635–37. 102. Laugel V, Cossee M, Matis J et al. Diagnostic approach to neonatal hyptonia: retrospective study on 144 neonates. Eur J Pediatr 2008; 167: 517–23. 103. Ross AK. Muscular dystrophy versus mitochondrial myopathy: the dilemma of the undiagnosed hypotonic child (editorial). Pediatr Anesth 2007; 17: 1–6. 104. Veyckemans F. Can inhalation agents be used in the presence of a child with myopathy? Curr Opin Anaesthesiol 2010; 23: 348–55. 105. Flick RP, Gleich SJ, Herr MMH, Wedel DJ. The risk of malignant hyperthermia in children undergoing muscle biopsy for suspected neuromuscular disorder. Pediatr Anesth 2007; 17: 22–7. 106. Gurnaney H, Brown A, Litman RS. Malignant hyperthermia and muscular dystrophies. Anesth Analg 2009; 109: 1043–8. 107. Frosch M, Roth J. New insights in systemic juvenile idiopathic arthritis. Rheumatology 2008; 47: 121–5. 108. Keegan MT, Whatcott BD, Harrison BA. Osteogenesis imperfecta, perioperative bleeding, and desmopressin. Anesthesiology 2002; 97: 1011–13.